Have you ever experienced that nagging feeling of not being able to empty completely during evacuation?
Do you often experience a feeling of bloating and bowel heaviness while regularly providing daily defecation?
Tenesmus is the medical name of a condition that, contrary to popular belief, can afflict even perfectly healthy people without obvious intestinal disease.
Read this page written by Dr. Luisella Troyer to find out what tenesmus is, when it occurs, and what can be done to treat it.
Single episodes of tenesmus, or sporadic episodes perhaps in conjunction with other known conditions (e.g., after gastroenteritis) should not be frightening: they are possible for everyone, and usually do not require specific therapies.
Instead, the proctologist should be contacted when these episodes begin to become frequent and systematic, such that they affect not only defecation but also daily life.
What is rectal tenesmus?
In Medicine, rectal tenesmus is defined as the sensation, reported almost always as extremely unpleasant, that prompts the urge to defecate, but without, however, reaching evacuation.
Alternatively, evacuation may be there, but it is perceived by the subject as unsatisfactory, of small quantity, and still leaving the sensation of not completely emptying the intestinal ampulla.
Sometimes, the urge to defecate is constant throughout the day, thus giving no respite to the patient who never, however, manages to satisfy it with complete and sufficient evacuation.
What is rectal tenesmus caused by?
Rectal tenesmus is caused by an abnormal contraction of the sphincter muscles, actual spasms, which simulate the normal stimulus of a full ampulla and thus prompt the patient to search, ineffectively, for evacuation.
In turn, these sphincter spasms are a symptom of an upstream problem of intestinal or proctological origin.
Some of the most common causes of rectal tenesmus include:
- Irritable bowel syndrome;
- Episodes of anxiety and poorly managed stress;
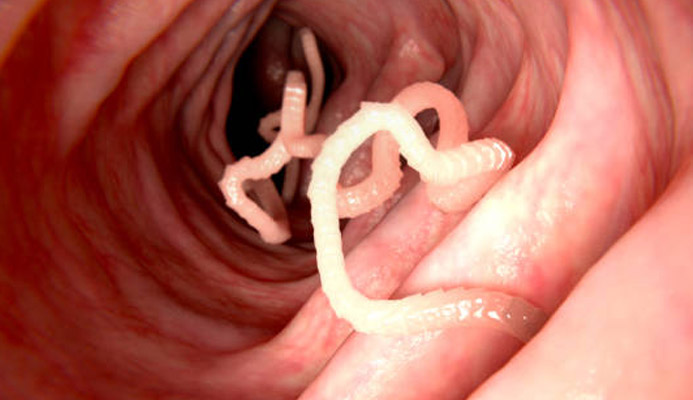
- Parasitic and bacterial infections such as chlamydia and gonorrhea;
- Spastic colitis;
- Ulcerative rectocolitis;
- Chronic constipation never treated;
- Proctitis and anitis;
- Anal fissure;
- Colorectal cancer and cancer of the anus;
- In women, rectocele and cervical cancer.
These pathologies, or otherwise pathological conditions, are only a small part of the causes that can lead to tenesmus.
What are the symptoms of tenesmus?
Tenesmus is itself a symptom, and manifests itself as the inability, albeit in the presence of stimulus, to perform complete and satisfactory defecation.
Patients with tenesmus often complain how, even after the act of defecation, it is impossible or very difficult for them to feel their intestinal muscles relaxed, thus manifesting, even without needing to, the urgency to defecate.
Sometimes, this sensation is accompanied by abdominal cramping and pain, meteorism and flatulence, and, in the case of proctitis and anitis, often also by anal burning and itching.
How is anal tenesmus diagnosed?
The diagnosis of tenesmus is clinical, and is made by the Proctologist Physician during the specialized proctological examination.
Even at the history stage, the symptoms reported by the patient put the Physician on the right track, directing the Clinician to the right diagnosis.
Nevertheless, proctologic examination is always necessary, more so to investigate the cause of tenesmus, which may originate from a proctologic problem that was never resolved or otherwise underestimated over time.
How is rectal tenesmus treated?
The treatment of rectal tenesmus is, playfully, linked to the treatment of the cause that creates the sphincter hyper-spasm.
The patient's medical history should be thoroughly investigated, and the entire colon should sometimes be examined (by colonoscopy) to make sure there are no polyps or cancerous lesions that could be the root of the problem.
In case of a lack of physiological reasons, it is imperative to investigate, also with the support of a Psychologist, any psychological issues of the patient, since many proctological diseases (such as irritable bowel syndrome) have their psychosomatic origin.
Which Physician can diagnose and treat rectal tenesmus?
The clinical specialist with great experience in all diseases of the rectum and anus is the Proctologist Physician.
Therefore, it is to him that one should turn when experiencing the symptom of rectal tenesmus, and it is to him that one should seek a specialized proctological examination.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- TENESMUS REFERS TO THE CONDITION IN WHICH THE URGE TO EVACUATE DOES NOT CORRESPOND TO A COMPLETE DISCHARGE, WITH THE SENSATION OF NOT HAVING COMPLETELY EMPTIED THE BOWEL;
- TENESMUS IS A SYMPTOM OF SPHINCTER MUSCLE DISTRESS, THE ORIGIN OF WHICH CAN VARY;
- THERE ARE MANY CAUSES THAT CAN LEAD TO TENESMUS, SOME DUE TO CHRONIC INFLAMMATORY CONDITIONS, SOME TO ACUTE DISEASE STATES;
- SINGLE SPORADIC EPISODES OF TENESMUS SHOULD NOT BE A CAUSE FOR CONCERN, AS THEY ARE ALWAYS POSSIBLE FOR EVERYONE, BUT RECURRENCE SHOULD MAKE ONE SUSPICIOUS;
- TENESMUS MAY GIVE SENSATION OF BLOATING, CRAMPING, ABDOMINAL PAIN AND METEORISM

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.