Are you a woman who has entered the second decade of life, or still young but has already given birth, and are you experiencing symptoms such as urinary and fecal incontinence, feeling of never being able to empty your bladder, and frequent pelvic pain?
You may be suffering from a particular syndrome, very common in women over 50 and in women who have already given birth, called descending perineum syndrome.
Read this page written by Dr. Luisella Troyer, Vascular Surgeon, to learn about what this syndrome is, which, as the name implies, causes the pelvic floor to slowly prolapse downward, triggering a variety of often very disabling symptoms.
The solution for the problems that causes the descent of the perineum, whether ofurinary incontinence or problems with defecationbeginsat a single act: that of the proctological examination.
It seems obvious, but often the patient, for reasons of embarrassment or shame, does not go to the doctor and does not talk about it with anyone, even her closest family members, preferring to try autonomous solutions that almost always boil down to resortingto absorbent diapers or purgatives and laxatives.
This should never be done, but rather a proctological examination with pelvic analysis should be performed as soon as possible.
That is the necessary step to begin a serious course of pelvic rehabilitation.
What is descending perineum syndrome?
In Medicine, an excessive descent (prolapse) of the perineum relative to the normal anatomical repere points of the pelvis is identified as descending perineum syndrome.
Clinically and as a general rule, a prolapse of more than 1.4 cm of the ano-rectal angle with respect to the bottom of the iliac bone (the so-called 'iliac tuberosities) at resting condition is considered pathological.
During straining, i.e., straining during urination or defecation, this distance increases and is considered physiological up to 3 cm, beyond which we can begin to speak of prolapse of the perineum.
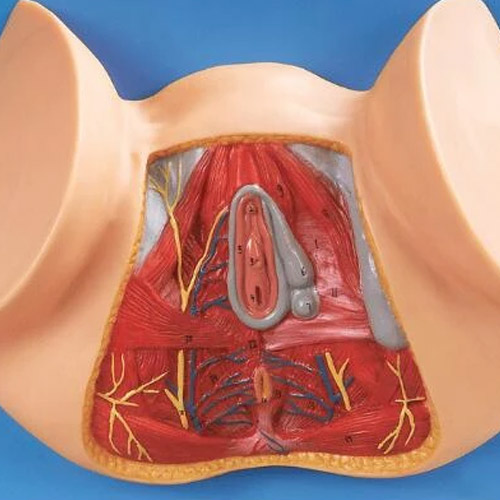
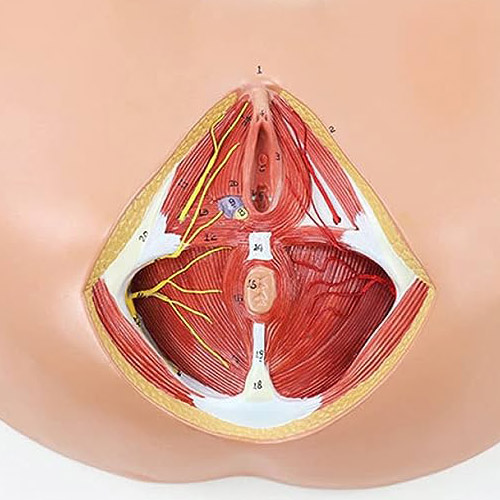
What is the pelvic floor?
In human anatomy, 'pelvic floor' refers to all those tissues, muscular, tendinous and connective, that have as their anchor points the pelvis, that is, the area below the pelvis, which is the base of the abdomen.
Given that, due to its physiological conformation, the human skeleton does not have structures dedicated to containing the internal organs of the abdomen, intestines and pelvic area, the task of this is delegated to the elastic tissues that, precisely, form as a kind of 'floor'.
On that floor rest all the internal pelvic organs, such as: the rectum, bladder, urethra, and prostate for men and the uterus for women.
The pelvic floor is a complex structure, consisting of three major muscle zones: the pelvic diaphragm, the urogenital diaphragm, and, of course, the sphincter zone (external sphincter and internal sphincter).
These core muscles are assisted by tendons and connective tissue, forming a cohesive, strong yet flexible structure, the health of which is essential to ensure the functionality of urination, defecation, and, of course, mating and pregnancy.
Why does the pelvic floor prolapse?

The set of muscles, tendons and connective tissue of the pelvic floor, having no other bony support structure, is more or less constantly under strain and pressure during daily life due to the undying action of gravity.
Although the tissues of the perineum are still designed to be elastic and resilient, like any other biological tissue they suffer from aging and slowing metabolism, which leads, inevitably, to slower cell regeneration and a drastic decline in collagen turn-over.
Collagen is that essential protein for our tissues, since, as the name of the rest suggests, it functions as a real glue.
Glue that our bodies use for many things: to make skin and panniculus adhere to the muscle tonaca, to make tendons open to bones, to make connective tissue in a good shape, and much more.
Collagen is an exceptional protein, but it has a limitation: after a while from its production, it loses its initial mechanical properties, and becomes less functional.
Because of this, our body continuously renews it, replacing old one (ce is destroyed by macrophages) with new one, in a mechanism called turn-over, not unlike the one that also continuously regenerates so many other cells in our body.
As we age, the slowdown in metabolism also results in a sharp slowdown in collagen turn-over, and this is clearly visible on our skin, for example, which sags and prolapses as it is no longer well adhered to the muscle tonaca.
The same happens to the supporting tissues of the pelvic floor: with less renewed and regenerated collagen, the whole structure gives way and prolapses downward.
This prolapse of the perineum is considered physiological within a certain limit for all people past the adult threshold of life, but under certain circumstances the prolapse is so obvious that it becomes symptomatic, and therefore pathological.
Any increase in intra-abdominal pressure is a major cause of pelvic floor prolapse and an element that, over time, worsens its degree and symptomatology.
Triggers, on the other hand, are all situations that increase intra-abdominal pressure, and consequently 'trigger' the symptomatology.
What are the triggers of prolapse of the perineum?

Speaking of pelvic floor prolapse, 'triggers' are defined as all those activities, diseases, lifestyles or physiological conditions that can increase intra-abdominal pressure, and consequently exhaust the supporting tissues of the perineum.
Therefore, they are concluded triggers:
- Aging;
- Chronic and untreated constipation;
- Some sports, such as weightlifting and body building;
- Pregnancy and childbirth;
- Obesity
Especially in multiparous women, pregnancy, so the labor and delivery, is a critical time for the entire pelvic floor structure, which is always abnormally (and quickly) stressed.
What are the symptoms of descending perineum?
The symptomatology of the descending perineum is directly related to the degree of exhaustion of the supporting muscles and connective structure.
Small prolapses, less than about 1.4 cm, are considered physiological in women who have given birth, and in women over 50 years of age.
Almost always, they are not even perceived, and therefore do not require therapy.
Only prolapses that, on average, exceed one and a half centimeters may give rise to symptomatology, more or less pronounced depending on the severity of the perineal slip.
That being said, the symptomatology of the descending perineum is complex, as, moreover, is the structure of the pelvic floor.
In general, considering that symptoms can obviously vary greatly from patient to patient and according to gender, they can be schematized into:
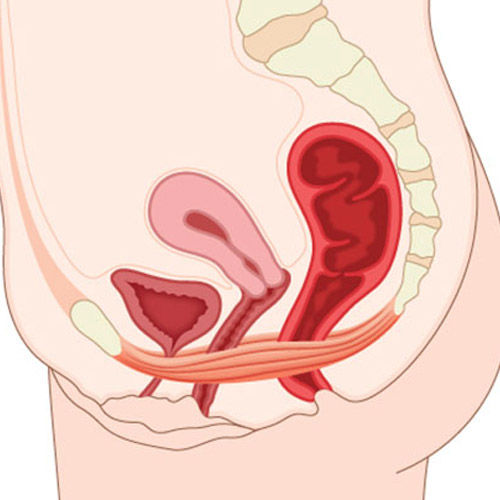
Difficulty in defecation
Moving down, the rectum becomes deformed, and stool therefore may become obstructed.
This symptom affects women the most, as the recto-vaginal wall can become strained and deformed, thus giving rise to rectocele;
Difficulty in urination
Sliding downward, the bladder loses its natural position, crushing (cystocele).
This can generate difficulty with urination, which becomes difficult and, in severe cases, a real pain for the patient;
Prostatitis and erectile dysfunction in men
Sliding downward, the bladder crushes the prostate, which becomes inflamed and thus gives rise to prostatitis, which tends to become chronic;
Difficulty during penetration in women
Sliding downward, the rectum begins to press on the vagina, as well as the uterus and urethra.
This can cause hypersensitivity of the vaginal area, with difficulty (or impossibility) to the sexual act of penetration;
Inflammation of the pudendal nerve
Sliding downward, the entire perineum begins to compress the pudendal nerve, causing chronic pain that is difficult to bear;
Fecal incontinence
The exhaustion of the sphincter muscles, chronic pudendal neuralgia, and relaxation of the connective tissues that hold up the entire peri-anal musculature causes a condition of open anus, which is the main symptom of fecal incontinence;
Urinary incontinence
More or less similarly for what happens to the sphincter muscles, the muscle compartment that regulates the bladder also deforms and relaxes, giving rise to urinary incontinence.
It should necessarily be remembered that these symptoms are a genetic trace: they are not always all present, and their degree of severity varies depending on the degree of pelvic floor prolapse, as well as the patient's general condition.
How is pelvic floor prolapse diagnosed?
Descending perineum is diagnosed by proctological examination with pelvic examination.
A key symptom for the Proctology Physician during the examination is the evaluation of the slippage of the rectum (and the pelvic floor in general) during straining.
What is the therapy for pelvic floor prolapse?
Pelvic floor prolapse requires specific therapy if and only if it is symptomatic, that is, it causes real and concrete problems for the patient.
Pelvic floor prolapses that are considered physiologic (common, for example, in women giving birth and over 50) are often asymptomatic, and therefore the patient is not even aware of them.
The therapy of excellence for prolapse of the perineum is rehabilitation therapy, which is most effective in the early stages of symptoms.
Rehabilitation techniques for pelvic floor prolapse currently considered the 'gold standard' for the condition involve a combination of four therapies:
- Dietary and bowel rehabilitation therapy to help the bowel return to soft and well-formed;
- Sensory biofeedback therapy;
- Functional electrical stimulation therapy;
- Physiokinetic therapy, for sensory-motor rehabilitation
These four techniques, neither pharmacological nor surgical, used together as directed by the Proctology Physician (and the help of experienced rehabilitation health professionals, such as physiotherapists, nurses, and massage therapists) help strengthen the muscles and tissues of the pelvic floor, bringing considerable benefit and thus reducing symptomatology.
Surgical therapy is associated only with severe cases of lacerations or complete exhaustion of the muscle-tendon supports, such as a perforated rectocele or severe cystocele.
Which Physician can diagnose and treat descending perineum?
The Physician who specializes in the diagnosis and rehabilitative treatment of pelvic floor prolapse is the Proctologist Surgeon.
He is the Physician to ask for help when you suspect you have a prolapse of the perineum, and he is the one who is qualified (also using specialized professionals) in pelvic rehabilitation protocols.
Do you need to rehabilitate your pelvic floor and are you from Dubai? Contact Dr. Luisella Troyer

Dr. Luisella Troyer is a Vascular Surgeon who has specialized in pelvic floor rehabilitation and diagnosis of descending perineum syndrome for many years.
At her Dubai clinic, Dr. Troyer is able to diagnose your pelvic floor prolapse as well as prepare the right rehabilitation therapy that can help you feel better by regressing the most troublesome symptoms of the condition.
Dr. Luisella Troyer and her associates, who are specialized in pelvic rehabilitation, operate state-of-the-art electromedical machines, combining electrostimulation with the best physical rehabilitation therapies.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- IN MEDICINE, DESCENDING PERINEUM REFERS TO AN EXCESSIVE DESCENT OF THE PERINEUM RELATIVE TO THE NORMAL RESTING POINTS OF THE PELVIS;
- BY PROLAPSING DOWNWARD, THE PERINEUM DISPLACES THE ENTIRE PELVIC FLOOR, WITH ALL ORGANS RESTING ON IT;
- THE MAIN ORGANS AFFECTED BY THE DESCENT OF THE PERINEUM ARE THE RECTUM, BLADDER, ANDUTERUS;
- THE MAIN SYMPTOMS OF DESCENDING PERINEUM VARY FROM MAN TO WOMAN, BUT MAY INCLUDE FECAL INCONTINENCE, URINARY INCONTINENCE, PAIN AND DIFFICULTY WITH DEFECATION, AND INABILITY TO HAVE SEXUAL INTERCOURSE;
- THE THERAPY OF EXCELLENCE FOR PERINEAL SLIPPAGE IS REHABILITATION, WHICH GIVES THE BEST RESULTS IN THE EARLY STAGES OF THE CONDITION;
- CONTRARY TO POPULAR BELIEF, DESCENDING PERINEUM CAN AFFECT BOTH MEN AND WOMEN, ALTHOUGH THE LATTER ARE, STATISTICALLY, MORE PRONE TO PELVIC PROLAPSE;
- INTRA-ABDOMINAL PRESSURE OF PREGNANCY AND CHILDBIRTH IS A TRIGGER, IN WOMEN, FOR THE ONSET OF THE PATHOLOGY

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.

















