Do you experience great pain when you have to go to the toilet?
In addition to pain, do you experience burning, tightness, or do you feel you can never completely empty yourself?
Pain during evacuation is a big red flag, which is a telltale sign of an injury somewhere in the anal or perianal area.
Read this page to find out what may be the causes of deep, intense anal pain during evacuation, and then contact Dr. Luisella Troyer, Proctologist Surgeon, for immediate help.
evacuation is not a painful act, and therefore should not cause any pain while performing straining (i.e., the abdominal and pelvic thrust necessary for defecation).
When this happens, it is always a symptom of tissue damage to the anorectal canal, which should therefore be investigated.
What is meant by pain during evacuation?

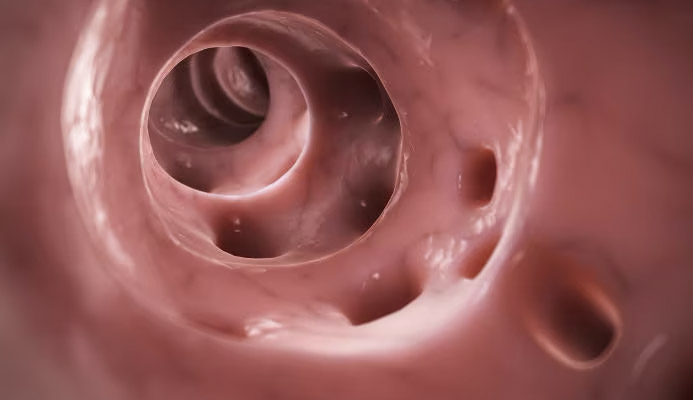
Evacuation, also called defecation, is that natural physiological act of expelling feces from the anal orifice after they have been properly formed and collected in the intestines.
More thoroughly, defecation is the last step in the long and complex journey of nutrition, that is, the act by which human beings, heterotrophic organisms (i.e., unable to synthesize organic compounds from inorganic elements), procure the chemical energy necessary for their subsistence.
With evacuation, our body expels waste substances, now devoid of any nutrient content and also deprived of fluids, which are useless for our physiological purposes.
Evacuation is therefore based on the emission of stool, which is largely composed of fiber, mucus and bacteria.
During defecation, the sphincters relax, allowing the anal orifice to open, from where the alvus exits.
In a healthy and well-fed subject, such a alvo is well formed, of good texture, soft and cylindrical in shape.
Defecation is an act often perceived as liberating, for many indeed pleasurable and relaxing, involving no pain or discomfort of any kind.
When this happens, and you experience any kind of pain, burning, generalized discomfort in the anal area right during defecation, it means that there is a problem upstream.
Pain is in fact an alarm bell of our body, warning us that, for a long series of reasons, a given area of the physique is damaged, and thus urging us not to overexert it.
Anal pain is therefore a symptom of anorectal pathology, which must therefore be investigated.
What are the possible causes of anal pain during defecation?
As mentioned earlier, having pain during defecation is not normal, it should not be there, and when it is there, it indicates some kind of injury to the tissues of the perineum area, or otherwise pathological situations.
The anus may ache, during the act of evacuation, for many causes, among which we can mention:
- Of thrombized or injured external hemorrhoids;
- Anal fissure;
- An injury or inflammation to the pudendal nerve;
- A sphincter injury;
- An anal abscess or anal fistula
Understanding exactly the origin of the pain during pouching (i.e., the act of straining to get stool out) is the first step in diagnosing the cause of the pain, as well as a necessary step for the necessary treatment.
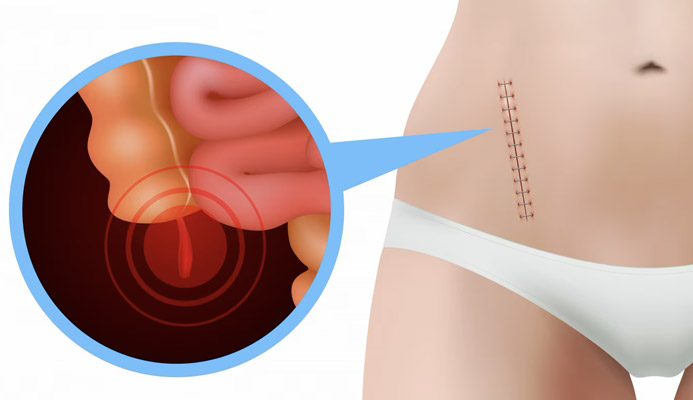
Hemorrhoidal thrombus and intense pain during defecation
Hemorrhoids are arteriovenous pads, present from birth within our anal canal.
They are basically anastomosed (i.e., fused together) arteries and veins, in which both arterial and venous blood therefore circulates.
They serve to vascularize the entire anal region and, to a small extent, help the sphincters in fecal continence.
We have three main hemorrhoidal pads: right anterior, right posterior, and right lateral, to which are added two other secondary pads of more limited anatomical significance.
Hemorrhoids, when healthy, do not give any kind of problem, and remain well within the anal canal.
When, for a long series of reasons mainly related to abdominal pressure, they bulge, that is when they extrude from their original anatomical location, leaking out and initiating what is commonly called hemorrhoidal pathology.
Internal hemorrhoids generally do not cause excessive discomfort, to wall bleeding during evacuation (due to friction of stool).
External hemorrhoids, on the other hand, because of the large innervation of the anal orifice, can easily thrombize, generating painful hemorrhoidal thrombi.
A hemorrhoidal thrombus is extremely painful, often requiring emergency surgical treatment: it creates pain for the patient during pondering, during even the slightest abdominal exertion, even while walking or during a cough.
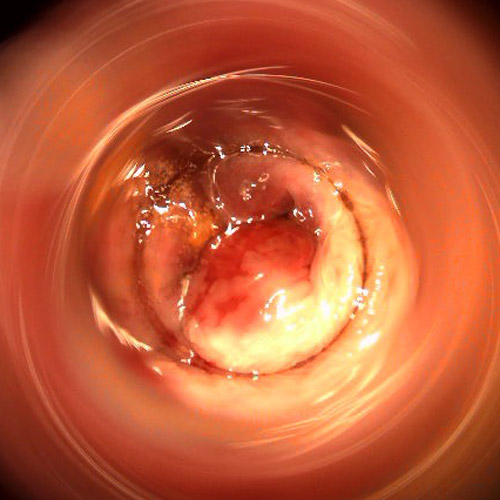
The anal fissure

An anal fissure is a wound in the anal canal that, for various reasons, fails to heal completely, eventually becoming a true ulcer.
Generally speaking, any anal canal injury that does not tend to heal within six weeks is considered an ulceration-prone wound, but this time should still be taken as a guideline, as healing capacity is still a personal factor and, often, also related to metabolism.
The reason for the slow or failure to heal is, in almost all cases, a hypertonus of the internal sphincter muscle (an involuntary muscle, thus not directly controllable), which, precisely as a result of the strain on the fissure, increases contractions and spasms, thus worsening the vasculature and generating the 'vicious circle' that prevents the injury from healing.
Anal fissure is always a vertical lesion parallel to the sagittal plane, which often blurs between the pleats of the perianal junction with the anal mucosa and, if not properly treated, causes great pain both during defecation and during normal daily movements.
Fortunately, only a small proportion of anal fissures degenerate into a permanent ulcer: most resolve spontaneously, albeit over a fairly long period of time, and medical and surgical intervention is thus relegated are to a small number of particularly problematic ulcers.
Anal abscess and anal fistula
Anal abscess is a purulent and particularly painful infection of the perianal area, originating from bacterial infection of a mucus gland.
Due to trauma, or another inflammatory event, sometimes some bacteria are able to penetrate the stratum corneum of the perianal skin, making their way to a mucus gland located between the sphincters and infecting it, thus giving rise to a violent pus-filled abscess.
Because there is no natural orifice to purge, the perianal abscess becomes abnormal and extremely painful, so much so that it brings great prostration to the patient, who is often completely debilitated by the great pain.
If not treated urgently with surgical incision and drainage, anal abscess can excavate a fistula, an artificial vent channel that gushes outward from the anal mucosa, often 'puncturing' the sphincters.
Defecation with an ongoing perianal abscess or infected fistula may be impossible: the patient's constant, great pain does not allow him or her natural pouching without great discomfort.
Anal abscess and anal fistula represent, along with hemorrhoidal thrombus, the leading cause of proctologic emergency access.
Rectocele and pain and difficulty in defecation

Rectocele is the herniation of the rectum into the vagina due to failure of the recto-vaginal wall.
It is a typical pathological condition of the already childbearing woman, which worsens with increasing age and pregnancies.
There are various levels of severity of rectocele, and the first level (mild rectocele) is considered physiological in women who have had at least one childbirth and are over 50 years old.
Along with rectocele, we often see all pelvic floor prolapse, in what is called descending perineum syndrome.
By recessing into the vagina, the rectum ceases to be straight, creating major problems during defecation, with pain and, often, the need to facilitate the release of stool manually.
Along with defecatory problems, the woman with rectocele often also experiences abdominal and pelvic pain, as well as the inability to have penetrative sex.
Inflammation of the pudendal nerve
The pudendal nerve is a peripheral innervation, originating from the sacral and pudendal plexus, from which it takes its name.
Its accomplishment is fundamental: it allows communicative termination with the external genitalia, anus and the entire perineum, as well as control of all pelvic floor muscles.
From this we can immediately see the importance of this nerve, both for sexual and defecatory functions.
Like all other nerves, the pudendal nerve can also suffer abnormal compression or injury, which can therefore damage it and cause more or less widespread neuropathy throughout the pelvic area, either temporary or permanent.
Pudendal nerve neuralgia is a sharp, intense pain, often described as difficult to bear, that severely limits both normal daily activities and specific acts, such as defecation and, in men, erection.
In women, abnormal compression of the pudendal nerve often causes a related condition known as vulvodynia.
Pain during defecation: many causes to investigate

As seen so far, pain during defecation is never within the normal range, and therefore must always be associated with an upstream pathological situation.
Therefore, in the event that you experience in suspected pain, or otherwise some kind of discomfort during evacuation, the best thing to do is to consult a Proctologist Physician, and perform a proctological examination.
A proctological examination is the medical act that can investigate the causes of pain during defecation, including making use of specific tests such as Electronic Endoscopy Videoproctoscopy, endoanal ultrasound, or anorectal manometry.
Do you suffer from pain during evacuation in Dubai? Dr. Luisella Troyer can help you

Dr. Luisella Troyer is a Proctologist Physician, specializing in all diseases of the rectum and anus.
In her clinic in Dubai, Dr. Troyer can help you understand the exact origin of your pain during evacuation, subsequently proposing the best therapy to resolve it.
Thirty years of excellence in Vascular Surgery and Proctology, a team that specializes precisely in emergencies and proctologic diseases, the safety of safe and pain-free Medicine.
To get rid of all discomfort with serenity.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- DEFECATION SHOULD NOTHURT, SHOULD NOT BURN, AND SHOULD NOT BRING WITH IT ANAL BLEEDING;
- INTENSE PAIN DURING DEFECATION ALWAYS INDICATES INJURY, OR OTHERWISE DAMAGE, TO THE TISSUES OF THE ANAL CANAL;
- THROMBIZED OR INJURED EXTERNAL HEMORRHOIDS CAN LEAD TO PAIN ON EVACUATION;
- USUALLY, VERY INTENSE PAIN DURING DEFECATION IS CAUSED BY A WOUND IN THE ANAL CANAL, CALLED ANAL FISSURE;
- ABNORMAL DAMAGE OR COMPRESSION OF THE PUDENDAL NERVE CAN ALSO LEAD TO PAIN DURING EVACUATION;
- IN THE CASE OF AN ANAL ABSCESS OR FISTULA, EVACUATION MAY BE IMPOSSIBLE, PRECISELY BECAUSE OF THE INTENSE PAIN THE PATIENT HAS TO ENDURE;
- PAIN DURING EVACUATION, REGARDLESS OF ITS NATURE, IS NEVERTHELESS ALWAYS A SYMPTOM THAT SHOULD PROMPT THE PATIENT TO A PROCTOLOGICAL EXAMINATION

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.