Do you happen to have an unsightly marisca on the edge of your anal orifice that, in addition to the purely cosmetic annoyance, occasionally flares up or gets caught in your underwear?
Anal marisca is a totally benign conformation that does not necessarily need surgical removal, but nevertheless it can be performed when, for cosmetic or functional reasons, excess perianal skin causes problems or embarrassment to the patient.
Dr. Luisella Troyer, Proctologic Vascular Surgeon, with her high degree of totally painless outpatient surgery, can help you remove your anal marisca safely, without discomfort.
Read this page to find out how to remove your anal marisca without any harm.
What is anal marisca?

Anal marisca is an excess of perianal skin, manifesting as a soft, usually elongated protuberance that extrudes from the anal orifice.
This is a totally benign lesion formed by excess skin, which may be congenital in nature (i.e., present as early as birth) or, much more commonly, acquired during life.
In contrast to other more dangerous lesions that are infectious in nature (such as anal warts), cutaneous marisca is predominantly a cosmetic problem that rarely gives rise to functional problems.
In some cases, however, its presence can create some discomfort for the patient, such as itching, frequent irritation, and sometimes even mechanical problems, as (although more rarely) sometimes the marisca can become entangled in undergarments and clothing, thus giving rise to small lesions or, in more extreme cases, small necrosis.
What is anal marisca caused by?
Anal marisca may be an excess of anus skin of primitive origin (i.e., already present at the time of birth) or, more commonly, secondary to some triggering factor that has forced the body to protect the anal orifice with more skin.
In the latter case, the most common triggers that can lead to the onset of anal marisca are continuous irritation or otherwise inflammation of the anal region, such as pathological hemorrhoids or frequent anitis (inflammation of the anus).
Sometimes, an anal marisca forms as a natural attempt to protect the mucosa in conjunction with an anal fissure, that is, a small, slowly healing anal canal wound.
In that case, a hypertrophic papilla first forms, which, as it becomes chronic, can develop into a full-fledged marisca.
Frequent cases of chronic diarrhea, perhaps due to irritable bowel syndrome, can also lead to consecutive proctitis (inflammation of the entire anorectal canal), resulting in the development of anal marisca.
Is anal marisca dangerous?
No, anal marisca is an absolutely benign lesion that is not related to other diseases.
Often the affected patient is very frightened, thinking that the extrusion is a tumor formation or a wart, or of an onset of hemorrhoidal prolapse, and this often leads him or her to request an emergency proctological examination.
The chances of an anal marisca turning into a malignant lesion (a cancer of the anus) are absolutely remote: the available literature reports only very rare cases of it, and therefore the lesion should not be considered (as opposed to anal warts) pretumoral.
What symptoms can an anal marisca give?
Generally, anal marisca is totally asymptomatic.
Apart from the extrusion of the skin forming it, it gives no other problems, and therefore the patient can live with it peacefully.
Sometimes, however, marisca can 'trap' some fecal debris, and thus make cleaning the anus more complicated.
In these cases, perianal dermatitis may develop due to maceration of the skin, causing itching and a feeling of irritation.
These are rare cases, it should be specified, but nevertheless they are one of the reasons why the patient often requests surgical removal of the marisca.
How can anal marisca be removed?
As it is natural to assume, being an excess of skin, the only therapy to eliminate marisca is surgical.
Removal of an anal marisca is almost never a functional prescription, but is often done for mere cosmetic reasons.
In fact, often the patient does not like the appearance of the skin hypertrophy, and therefore asks the physician for its removal.
When functional, on the other hand, the procedure is performed to permanently resolve the problems of irritation and itching that, although infrequent, marisca can lead to.
Anal marisca removal surgery is performed on an outpatient basis under local anesthesia.
The marisca is removed by the Proctologist Surgeon using surgical scissors or scalpel, and the wound then cauterized with laser or electrosurgery.
The procedure is totally painless, and generally takes only a few minutes.
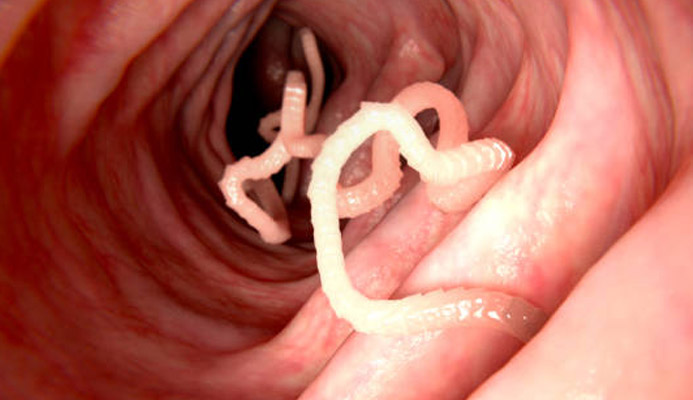
Anal marisca or warts?
Anal marisca is often confused with another pathology of the anal canal and perianal area, anal warts.
However, these two lesions are distinct and different: marisca is a benign hypertrophy of the perianal skin, while condylomata are the immune system's response to a Human Papilloma Virus (HPV) infection.
Anal marisca is not a pretumoral lesion, while condylomata are: this means that a marisca cannot turn into a tumor of the anus (except in cases so rare as to be essentially irrelevant), while condylomata can, though rarely.
The two conditions are therefore extremely different, and are often confused by the patient, but instead appear well apparent to the experienced Proctology Physician.
Is it true that anal marisca removal surgery is very painful?
Absolutely not.
Removal surgery is a small procedure performed under local anesthesia, thus totally painless.
Postoperative discomfort is also really contained: it lasts only a few days and can be safely kept under control with common local painkillers (if needed).
Perianal skin usually heals very quickly, and in about two weeks there is almost complete healing.
But do I have to remove the anal marisca?
No: removal of the anal marisca, if it is not symptomatic, is a purely cosmetic procedure, and therefore is at the patient's complete discretion.
Only in cases where the marisca becomes easily inflamed or irritated, thus giving discomfort and itching, is there a functional indication to remove it.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- ANAL MARISCA IS AN EXCESS OF SKIN OF THEANAL ORIFICE;
- ANAL MARISCA IS A TOTALLY BENIGN LESION THAT SHOULD NOT BE OF CONCERN TO THE PATIENT;
- THE CAUSE OF ANAL MARISCA MAY BE CONGENITAL OR, MORE COMMONLY, ACQUIRED;
- HEMORRHOIDAL PROLAPSES, FISSURES, FREQUENT ANAL INFLAMMATION, ANDANAL SEX CAN LEAD TO EXTRUSION OF A MARISCA;
- ANAL MARISCA RARELY CAUSES FUNCTIONAL PROBLEMS, BUT IN SOME CASES MAY GIVE RISE TO ITCHING AND INFLAMMATION;
- ANAL MARISCA SHOULD NOT BE CONFUSED WITH ANAL CONDYLOMAS;
- REMOVAL OF ANAL MARISCA IS SURGICAL, AND IS PERFORMED THROUGH A SMALL OUTPATIENT PROCEDURE

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.