Ulcerative rectocolitis is, along with Crohn's disease and celiac disease, one of the already severe autoimmune diseases of the intestine.
Those affected experience acute periods to periods of remission, with violent pain and diarrheal discharges almost always accompanied by copious blood loss (rectorrhagia).
Diagnosis of ulcerative rectocolitis is difficult, as is treatment: being an autoimmune disease, its exact origin is currently unknown to science.
Modern medicine, however, although not yet able to cure the disease, can greatly improve patients' quality of life.
Read this page to find out more about ulcerative rectocolitis, and what can be done to treat it.
What is ulcerative rectocolitis?

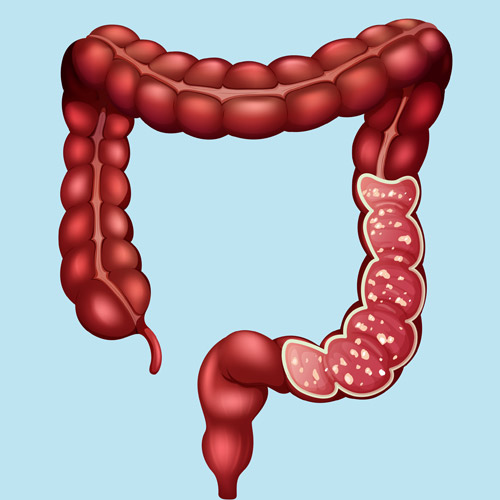
Ulcerative rectocolitis, also simply called ulcerative colitis, is an inflammatory bowel disease, chronic in nature, extremely selective in that it affects only the mucosa of the colon (with preference given to the rectal).
The inflammation has a tendency to remain confined to the rectum (hence the name), but can still spread throughout the entire colon, mainly in the descending segment.
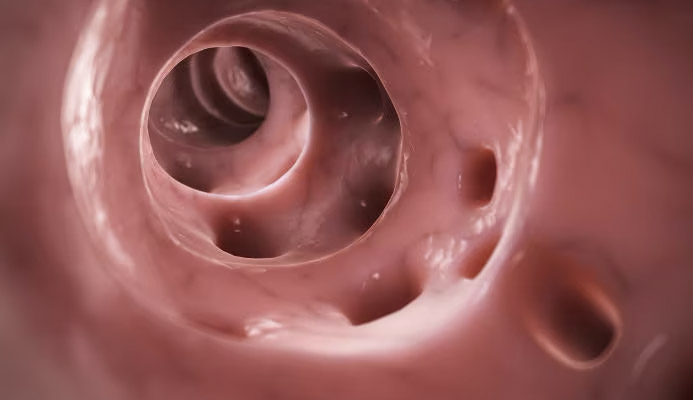
The mucosa afflicted with ulcerative colitis loses its physiological pinkish coloration and becomes inflamed, covering itself with purulent ulcers, which are in fact the last stage of the disease.
What is ulcerative rectocolitis caused by?
Ulcerative rectocolitis is, in the current state of Medicine, considered an idiopathic disease, with unknown original causes.
Statistically speaking, it makes no sex distinction or preference, is more common in industrialized countries, and strikes at any age, with some predilection for the adult and senile segments of life.
These characteristics of it, coupled with the fact that it turns inexplicably against a very specific organ in the body, lead one to suspect an autoimmune origin.
Like all autoimmune diseases, ulcerative rectocolitis is shown to be an exaggerated response of the body to generally harmless environmental factors, such as the presence of physiological gut microbes, which are generally present in symbiosis with our digestive activity.
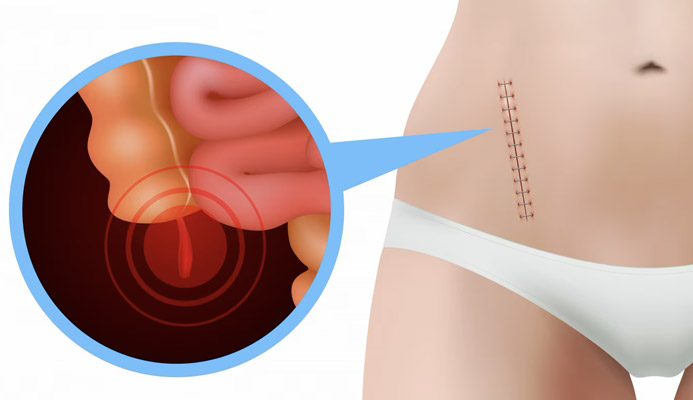
In Colonproctological Surgery, colectomy is the tout-court removal of the colon.
The surgery, performed exclusively as a last resort with regard to ulcerative rectocolitis, brings with it inevitable discomfort and limitations for the patient, but it is really used as a last weapon when none of the supportive pharmacological therapies work.
The pain and suffering of acute attacks of ulcerative rectocolitis, in these very severe cases, therefore justify the use of this extreme surgery.
Fortunately, modern anti-inflammatory and immunosuppressive therapies have really minimized this type of surgical therapy.
What are the symptoms of ulcerative rectocolitis?
The main symptom of ulcerative rectocolitis is diarrhea, which takes the form of violent attacks with scattered and cramping, often followed by actual anal bleeding (rectorrhagia).
These attacks can be so violent that hospitalization is required to administer emergency therapy with corticosteroids, antibiotics, and immunosuppressants.
During attacks, the patient totally loses hunger and thirst, partly because of the intense intestinal pain, and this causes, along with violent diarrheal discharges, dehydration.
Accompanying these main symptoms, there may then be extraintmestinal localized problems, such as dermal rushes ulcers in the lower extremities (also purulent), arthritis of both peripheral joints and spine, and the appearance of reddish, painful nodules.
The origin of these side symptoms is not yet known to science, but they disappear upon remission of the main symptoms of ulcerative rectocolitis.
Diarrheal discharges and chronic ulcerations in the rectum can then lead to a whole range of related conditions, such as chronic proctitis, possibility of perinatal abscesses and anal fistulas, development of hemorrhoidal pathology, and painful fissures, which do not heal spontaneously.
How is ulcerative rectocolitis diagnosed?
The diagnosis of ulcerative rectocolitis is particularly difficult, especially because it can be confused symptomatically with other chronic inflammatory bowel diseases, such as Crohn's disease.
The first-line examination for its diagnosis is therefore colonoscopy, accompanied by an intestinal biopsy.
What is the treatment for ulcerative rectocolitis?
At present, Medicine cannot explain the exact origin of ulcerative colitis, and as a result, even the cure is therefore not possible.
Be that as it may, a number of palliative therapies are available that, although not sufficient to eradicate the disease, can still bring great relief to the patient, and lessen the symptoms of acute attacks.
Thus, the aim of this therapy is to alleviate the symptoms of ulcerative rectocolitis while limiting its attacks, possibly diluting them over time into less and less frequent episodes.
To do this, mesalazine, a powerful drug that acts directly on the intestinal mucosa, flaring it, may be prescribed.
Mesalazine should also be combined with the appropriate immunosuppressive therapy, which goes to act directly on the lymphocytes responsible for attacking the intestinal walls.
Excellent in this regard are aztioprine and 6-mercaptopurine, two molecules that are capable not only of regressing inflammatory symptoms but also of blocking new attacks for long intervals of time.
In case of resistance to drug treatments, new synthetic drugs capable of selectively blocking lymphocytes and helping to flare the mucosa may be administered during acute phases.
Colectomy, that is, surgical removal of the entire colon, is the radical operation that is prescribed only as a last resort, only when the patient does not respond to any of the drug therapies and the acute attacks present themselves chronically and increasingly dramatically, such that they prevent him from any work or even social activity.
Who to contact if you suspect you have ulcerative rectocolitis?
The medical specialist with the greatest experience in ulcerative rectocolitis is the Proctology Physician, but the Gastroenterology Physician is also decidedly familiar with the condition, and can therefore be consulted.
Given the severity of the symptoms and the need to intervene promptly with appropriate palliative therapy, it is wise for patients who suspect they have ulcerative rectocolitis not to initiate 'do-it-yourself' therapies of any kind, but to see a competent physician exclusively.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- ULCERATIVE RECTOCOLITIS IS A CHRONIC INFLAMMATORY-BASED DISEASE THAT AFFLICTS THE WALLS OF THE INTESTINAL MUCOSA, ESPECIALLY THE SECTION OF THE RECTUM AND DESCENDING COLON;
- THE DISEASE LEADS TO CONSTANT ULCERATION OF THE INTESTINAL WALL, GIVEN BY THE SELF-ATTACK OF LYMPHOCYTES ON THE MUCOSAL CELLS THEMSELVES;
- IT IS ASSUMED THAT THE ORIGIN OF THE DISEASE IS AN EXAGGERATED ATTACK AGAINSTCOMMON INTESTINAL BACTERIA, WHICH INSTEAD TURNS INTO SELF-AGGRESSION;
- SYMPTOMS FOR THE PATIENT WITH ULCERATIVE RECTOCOLITIS ARE SEVERE CRAMPING AND ABDOMINAL PAIN, VIOLENT DIARRHEAL DISCHARGES ACCOMPANIED BY ACTUAL ANAL BLEEDING;
- LIKE MANY OTHER AUTOIMMUNE DISEASES, A DEFINITIVE CURE FOR ULCERATIVE RECTOCOLITIS IS CURRENTLY UNKNOWN;
- SUPPORTIVE THERAPY FOR ULCERATIVE RECTOCOLITIS AIMS TO REGRESS SYMPTOMS, FLUSH THE INTESTINAL MUCOSA, AND RESTORE COLONIC BALANCE TO ACCEPTABLE LEVELS FOR THE PATIENT;
- NEW IMMUNOSUPPRESSIVE DRUGS AND MODERN SYNTHETIC ANTIBIOTICS USUALLY GIVE EXCELLENT RESULTS, AND ALLOW THE PATIENT A RETURN TO A NORMAL LIFE, DECREASING, OVER TIME, THE INCIDENCE OF RECURRENCE;
- COLECTOMY, I.E., SURGICAL REMOVAL OF THE ENTIRE COLON, IS RESERVED EXCLUSIVELY FOR VERY SEVERE CASES, WHICH DO NOT RESPOND TO DRUG THERAPY

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.