There is a particular disease that, each year, affects more than 15 million people worldwide, still causing thousands of deaths, often from delayed surgery. I
is a disease known since ancient times that, before the advent of modern Surgery, always gave lethal outcomes, and was therefore feared.
Even in the present day, if not treated quickly, it can still give a fatal course, although this extreme occurrence, in countries with advanced and low-cost health care systems, is usually rare now.
Inflammation of the vermiform appendix of the large intestine, called appendicitis, is now easily treatable with minor surgery, but it can be a problem if it is underestimated or delayed in resolving treatment, called appendectomy.
Read this page to find out what appendicitis is, what are its original causes, and what are the treatments, medical and surgical, to resolve it.
The function of the appendix pendula and its real utility are still unclear to Medicine.
This appendix is also present in other mammals (notable, in size, is that of rabbits, for example), but its evolutionary origin is still not perfectly clear.
However, its function of lymphatic absorption is negligible (not to say insubstantial, being a crude and nonfunctional apparatus ), and therefore it can be removed without any problems, in case of appendicitis, causing no functional consequences.
What is appendicitis?
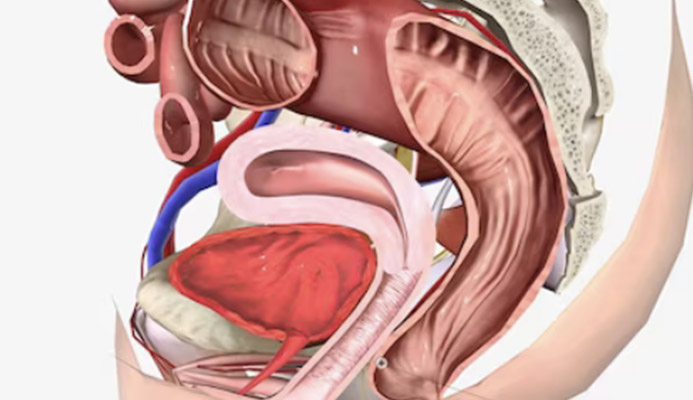
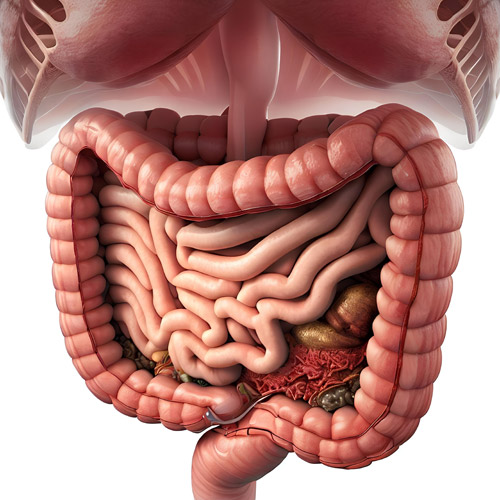
In Medicine, appendicitis is identified as the inflammation, or infection, of the distal tract of the large intestine, opposite the anus, called the cecal appendix (or vermiform appendix).
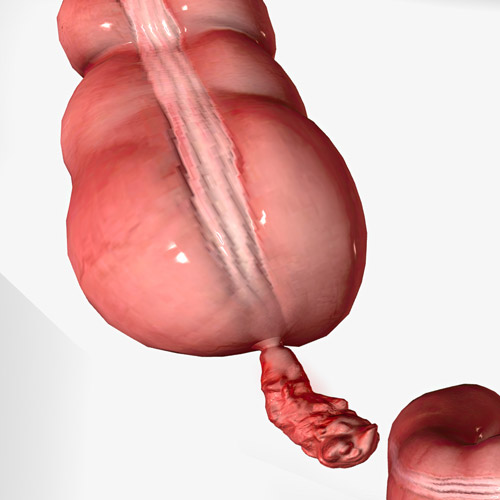
The norms hint well at the shape of this curious anatomical part, which extrudes from the cecum of the colon worm-like, and is usually 5 to 9 cm long (but there are cases of even longer appendages).
This appendix is essentially composed of a large number of lymphatic vessels joined and compacted together, lined with muscular tonaca and intestinal mucosa.
This particular conformation makes the appendix a true lymphatic filter, unable to absorb chyle (the food already processed by the small intestine).
It only takes a few organic fragments that are the result of digestion, happened to be in the appendix by chance, or even fecal residues from the colon, to inflame it and trigger what is called appendicitis.
Although it is always present near the cecum, the vermiform appendix can change, spatially, positioning, depending on the individual's own peculiarities, and this also determines its predisposition to become inflamed or not.
Why does the appendix flare up?

As mentioned just above, the appendix is a crude lymphatic organ that is lined with intestinal mucosa but has no assimilatory properties.
Its presence in humans and many other mammals has not yet been well explained, but it is assumed to be an evolutionary legacy that has now atrophied.
The atrophy of the appendix makes it extremely narrow in diameter: in fact, the lumen of the pendulous worm is tiny, and it only takes a few fragments of organic debris to obstruct it, and thus set off inflammation or, in some cases, directly an infection.
Premised on this primary cause, the triggers that can occlude the lumen of the vermiform appendix are:
- Chyle residues, i.e., food already stripped of nutrients from the small intestine, which have become hard and stony (coprolites);
- Undigestible or maldigested residues such as seeds and seedlings, grapes, etc;
- Intestinal bacteria and parasites, which cause swelling (hypertrophy) of the lymphatic tissue, thereby occluding the lumen;
- Gallstones;
- Abnormal compression, such as a tumor mass growing by pressing on the appendix
Given that the lumen of the appendix is, as mentioned, extremely contained, a total obstruction of it is an event that causes a lack of vascularization of the area and, consequently, tissue necrosis.
Necrosis, or tissue death, is an extremely dangerous situation: the appendix can burst or perforate, thereby releasing bacteria and infection into the peritoneal cavity, causing potentially fatal peritonitis.
Peritonitis, always a serious event, if not treated promptly leads to septicemia (bacterial infection directly into the bloodstream) in a short period, which in turn results in a lethal outcome.
How quickly does appendicitis develop?

nflammation of the appendix, again given by the occlusion of the lumen and the absence of vascularization, is a gradual process, which has been divided in the clinical setting into three stages:
Catarrhal phase
This is the absolute first phase of the inflammatory process, which is still well circumscribed.
The interior of the lumen is swollen with great mucus production.
It is the only phase in which antibiotic treatment can take effect, before the necessary surgical intervention;
Phlegmon phase
Congestion increases and causes the vessels to thrombize, which are therefore unable to properly supply the appendix with blood.
There is total swelling of the entire appendix, with the emission of purulent material and, often, fecal debris.
Surgery should be performed urgently, before there is a risk of perforation and subsequent peritonitis;
Gangrenous phase
A lack of blood supply causes tissue necrosis, and the entire appendix is swollen, black or greenish-gray, pus-laden, and ready to burst at any time.
Often, pus contaminates the peritoneum even without perforation, causing it to lose its natural luster.
This is a medical code red situation, requiring immediate surgical intervention.
Unfortunately, there is no universal time frame for the evolution of inflammation from the catarrhal to the gangrenous phase: the disease can degenerate even within hours, making surgical access mandatory and immediate.
Other times, however, the gangrenous stage is reached after a few days, giving more time to intervene.
Spontaneous regression of inflammation is an extremely rare event, and in any case not sufficient to procrastinate medical treatment.
The risk of appendix perforation, peritonitis, and sepsis of the abdominal cavity (an event that is always fatal to the patient) do not justify delay in treatment.
What are the symptoms of appendicitis?

Common classic symptoms are abdominal pain, vomiting, nausea with poor appetite, fever, general exhaustion, diarrhea, or stubborn constipation (even in patients who have never had constipation problems).
The abdominal pain usually occurs localized in the right iliac fossa (it may vary, however, depending on the anatomical positioning of the appendix) and is usually reported as similar to that, intense, of renal or biliary colic.
Appendectomy is now considered a commonplace (in fact, no surgery, even the smallest, ever is), or at any rate routine, but it should be remembered that, for centuries, inflammation of the end of the cecum of the colon was one of the leading causes of death from infection in the population.
Even today, especially in health-deprived areas of the world, it is estimated that millions of people a year die because of lack of access to appendectomy surgery.
How is appendicitis diagnosed?

Diagnosing appendicitis may not be easy at first glance, as its symptoms are varied and common with those of other conditions, such as a gastroenteritis.
However, even a non-specialist Physician, with adequate clinical insight, can diagnose appendix inflammation through the use of special abdominal maneuvers.
These maneuvers start from a simple concept: the appendix is nothing more than an inflamed and often infected part of the intestine, and as such, when stressed, can trigger a painful impulse.
This impulse is elicited by the famous Blumberg maneuver: a slow, progressive pressure on the abdominal wall in the direction of the appendix, which is followed by a rapid retraction of the hand.
This movement causes the appendix to 'slam' onto the peritoneum, causing violent and intense pain to the patient.
The positivity of this maneuver alerted the Physician, and prompted him to suspect the diagnosis of appendicitis.
Another very useful maneuver, often associated with the Blumberg maneuver, is the Rovsing maneuver, in which the Physician performs a gradual upward pressure on the left iliac fossa, which 'moves' the bowel just enough to touch the appendix and thus cause pain and relative positivity on examination.
These maneuvers are usually sufficient for the physician to prescribe the patient's hospitalization, which is usually done on an urgent basis.
However, it is possible, often directly in the hospital, to perform a blood leukocyte count test and, in the case of preoperative doubts, an abdominal ultrasound or pelvic CT scan, the latter performed only in the case of diagnostic doubts or situations that the surgical team considers special.
What is the treatment for appendicitis?
The first-line therapy, often performed as an emergency, is surgical, and involves removal of the now infected or inflamed appendix.
This operation, called appendectomy, is performed under general anesthesia, laparoscopically or, if the situation is particularly complex (as in the case of pre-perforations or peritonitis) by laparotomy.
Obviously, lacking a true surgical cut, laparoscopic surgery provides the shortest recovery time (a few days, with discharge within 48 hours if there are no complications).
However, even surgery using the classic laparotomy technique, which involves a small abdominal cut, has been hyper-perfected over the centuries: since the late 1700s, when it was first perfected, such surgery has become less and less invasive and effective, with smaller and smaller incisions and faster and faster recoveries.
The two techniques, both laparoscopic and classic laparotomy, are equivalent in terms of results, and still have, regardless of the type of access, the same surgical protocol: vascular ligation of the arteries supplying the appendix and dissection of the appendix, with suitable suturing of the intestinal cecum.
Appendectomy surgery is, by far, the second most performed surgery worldwide.
Drug therapy for appendicitis, based on the administration of antibiotics, is proposed only in sporadic cases, and in any case has an effect only in the first stage of inflammation.
Whom should you turn to if you suspect appendicitis?
Any physician, even a generalist, if equipped with a good clinical eye and decent intuition, can diagnose appendicitis.
Thus, in general, the first access physician to whom one should turn is the primary care physician or, in children, the Pediatrician.
Appendectomy surgery is a classic of both General Surgery and Coloproctologic Surgery, and is often performed by an Emergency Surgeon, Colonproctologist, or otherwise General Surgeon, in a hospital setting.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- THE VERMIFORM APPENDIX IS THE LAST PART OF THAT AREA OF THELARGE INTESTINECALLED THE CECUM;
- THE APPENDIX IS A CRUDE AND VIRTUALLY ATROPHIED LYMPHATIC ORGAN , CONSISTING OF COMPACTED LYMPH VESSELS COVERED BY MUCOSA AND INTESTINAL MUSCULATURE;
- THE APPENDIX HAS A VERY SMALL INTERNAL LUMEN , AND IS NOT CAPABLE OF ABSORBING ORGANIC DEBRIS THAT MAY EVENTUALLY SEEP INTO IT;
- FOOD OR FECAL DEBRIS MAY OBSTRUCT THE LUMEN OF THE APPENDIX, THUS CAUSING INFLAMMATION OR BACTERIAL INFECTION;
- INFLAMMATION OF THE APPENDIX RARELY RECEDES ON ITS OWN, BUT RATHER IN ALMOST ALL CASES DEGENERATES INTO A FULL-BLOWN INFECTION, SOON LEADING TO NECROSIS OF THE ORGAN;
- SYMPTOMS OFAPPENDICITIS, I.E., INFECTION OR INFLAMMATION OF THE APPENDIX, INCLUDENAUSEA, VOMITING, DIARRHEA, ABDOMINAL PAIN AND SPASMS, POOR APPETITE, AND FEVER;
- GENERALLY, TREATMENT FOR APPENDICITIS IS SURGICAL, INVOLVING REMOVAL OF THE INFECTED APPENDIX;
- ANTIBIOTIC TREATMENT IS RARELY EFFECTIVE, AND SHOULD BE RESERVED ONLY FOR THE EARLY STAGES OF APPENDICITIS;
- SURGICAL REMOVAL OF THE INFECTED APPENDIX IS CALLED APPENDECTOMY, AND CAN BE PERFORMED EITHER LAPAROSCOPICALLY OR LAPAROTOMY;
- IF ACTION IS NOT TAKEN IN TIME, THE INFECTED APPENDIX MAY BURST OR PUNCTURE, SPREADING THE INFECTION INTO THE PERITONEUM AND THUS LEADING TO DANGEROUS PERITONITIS

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.