Do you think you are suffering from anal condylomatosis?
n the peri-anal area, that is, around the anal orifice, do you notice strange growths, similar to 'cockscombs'?
Do you have anal itching, frequent dermatoses, which you think are due to HPV infection?
Read this page to learn all about anal warts, including modern treatments to cure them.
The HPV virus is unable to survive outside cells, but indirect infection (i.e., through contaminated objects) is always possible, although rarer.
This is because on objects and places it is always possible for there to be biological traces of the infected patient, such as fragments of epithelium, on which a high viral load is still present.
The virus survives in cells detached from the host for about 20 minutes: all in all, enough time to infect a new host, if the condition permits.
This is why swimming pools, showers, saunas and public places, especially if not well sanitized, can be a source of infection for the Papilloma virus.
What are anal warts?

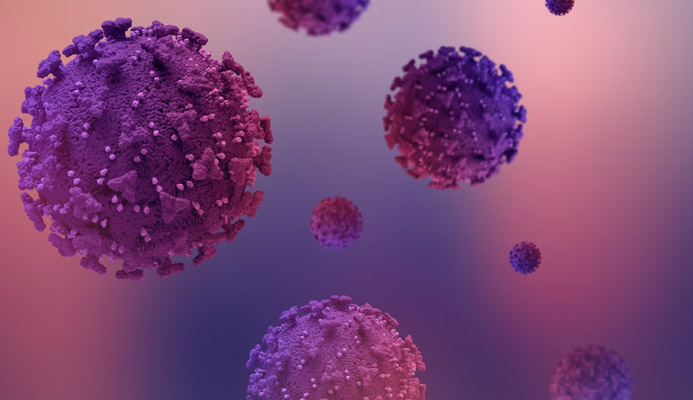
Anal condylomata, also called ano-genital warts, are pre-cancerous lesions of a benign nature, caused by an extreme response of our immune system to the infection of a virus, Human Papilloma Virus (HPV).
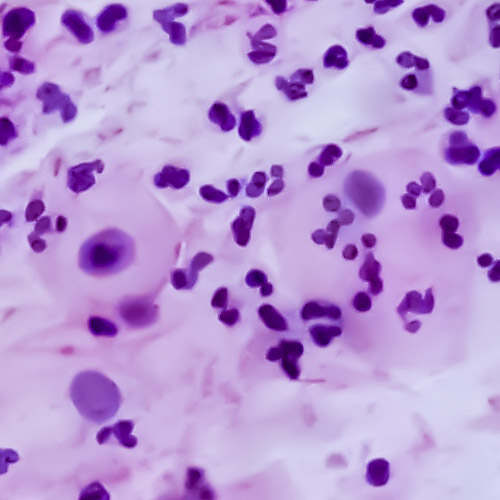
HPV, a virus classified as 'naked virus', without a protective outer pericapsis, is an opportunistic virus that includes many specific types (more than 120, at the current state of research), divided into as many as 16 groups.
Papillomavirus is a dermatological virus, that is, it primarily attacks skin cells, and is transmitted by direct contact with infected surfaces.
This type of infection, which requires direct contact, makes it rightfully part of the long list of Sexually Transmitted Diseases, or STDs.
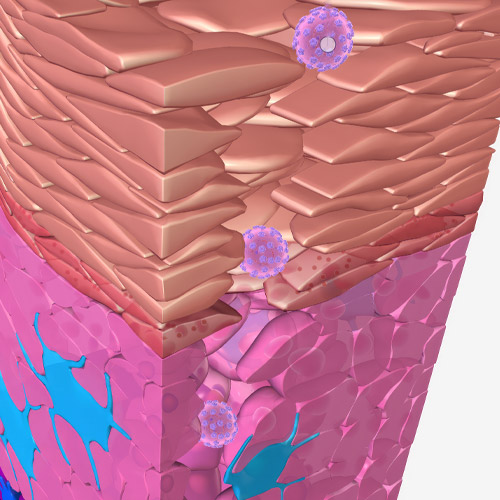
Anal condylomata are the immune system's response to an HPV infection that, for many reasons, the immune system itself has failed to sufficiently contain.
Overwhelmed by the virus, the body therefore decides to 'push' the infected cells outward, on the skin's surface, thus causing the condylomatous lesions to erupt.
The process of anal condyloma formation is not unlike that of common warts, which are also caused by HPV infection, albeit of a different type.
What are the causes of anal warts?
Anal condylomata are true pre-cancerous lesions, formed directly by our immune system attempting to isolate and confine the virus to the outside of the body.
For this to happen, the virus must find an immune system, however, deficient, depressed, either from temporary causes or from chronic infections.
In a healthy immune system, of a healthy, adult person, the HPV virus as it is passed, without being symptomatic, and without thus raising the host's suspicion (which, almost always, is not really aware of the infection).
Warts occur exclusively when the virus finds a suitable environment for its overgrowth, without being effectively thwarted by the immune response.
This is why the highest frequency of condyloma occurrence (60% to 80% of cases) occurs in people with inadequately treated HIV infection, which gives rise to Acquired Immunodeficiency Syndrome (AIDS).
However, the virus can spread unchecked even in perfectly healthy people who are, however, undergoing a period of mental and physical stress, such as after a long antibiotic treatment, chemo or radiotherapy, heavy flu, broncho-pneumonia or pneumonia, or, in any case, a disease that has debilitated the body and thus lowered the immune system.
But is HPV infection common in the world?
HPV infection is a great problem: WHO estimates that about 75% of the entire adult human population has contracted the Human Papilloma virus at least once in their lifetime, but a large proportion of this percentage is still asymptomatic.
This incredible rate of infection can be explained by the relative ease of transmission of the virus (simple direct contact, even with the genital mucous membranes) and the small viral load it takes to trigger an infection that is dangerous to our bodies.
As a virus belonging to the STDs, sexual intercourse is still the preferred means for Papillomavirus, even the protected ones.
In fact, even in the presence of adequate prophylactic, it is still not sufficient to ensure total protection from the virus, and therefore infection (although less likely) is still possible.
Are there any categories that are at greater risk of HPV infection?
As a sexually transmitted virus that prefers to attack debilitated hosts, it is possible to establish a category of people who, probabilistically, have a greater chance of infection.
They are:
Homosexual subjects
The virus penetrates more easily into the anal mucosa because it is not protected by the stratum corneum of the skin.
Likewise, the micro-lesions that invariably occur during anal intercourse weaken the mucosal defense, making it easier for the virus to gain access;
HIV-infected individuals who are not adequately treated
HIV-infected patients who do not follow regular antiviral therapy constantly see their immune systems engaged in counteracting the viral infection, and this generates, in the long run, chronic immunodepression, which in its final stages turns into AIDS.
This is helpful for the HPV virus, which then finds fertile ground to thrive.
Modern antiviral therapy is able to minimize HIV infection by returning immunological parameters to levels comparable with the uninfected, and therefore should be started immediately, and be continued steadily, according to the maintenance plan decided by the Immunologist;
Sex workers (sex workers)
HPV is transmitted primarily, but not exclusively, sexually through direct skin/mucosal contact.
This possibility of infection is greatest in the anal and genital areas, as they lack epidermis.
Mechanical contraceptive protection, with the use of condoms, unfortunately does not guarantee total impermeability to the virus: contagion is always possible, although the rates are much lowered.
This is why so-called sex workers, i.e., individuals who habitually engage in the profession of meretriciousness, are potentially more exposed to HPV infection (with all other STDs);
People in promiscuous relationships
For the same reasons stated above regarding sex workers, individuals in casual, polyamorous, or otherwise promiscuous relationships are also more likely to become infected has HIV
Unhygienic people and frequenters of gyms, saunas and swimming pools, or public baths
HPV can be transmitted sexually but also by simple contact with infected surfaces.
Public places, therefore, where there may be mingling of towels or personal effects, are places of danger, especially if surfaces are not well disinfected.
In a healthy and healthy subject (non-smoker), HPV infection as it comes... It goes away, without giving any symptoms.
In fact, the human papilloma virus is a typical opportunistic virus, which prefers to attack hosts with low immune defenses.
An efficient immune system can always effectively counteract it, and prevent its hyper-proliferation (and the development of anal warts).
What are the symptoms of anal warts?
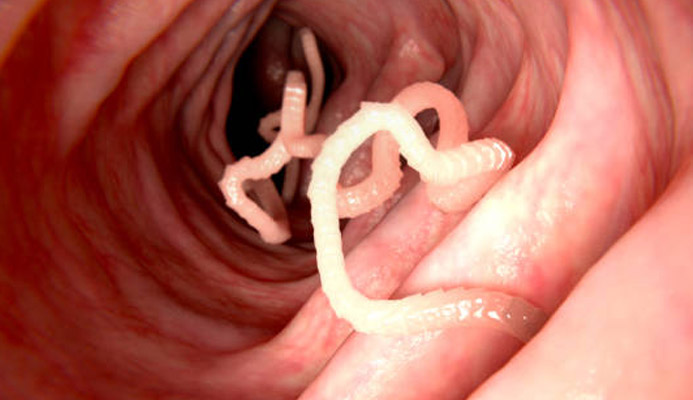
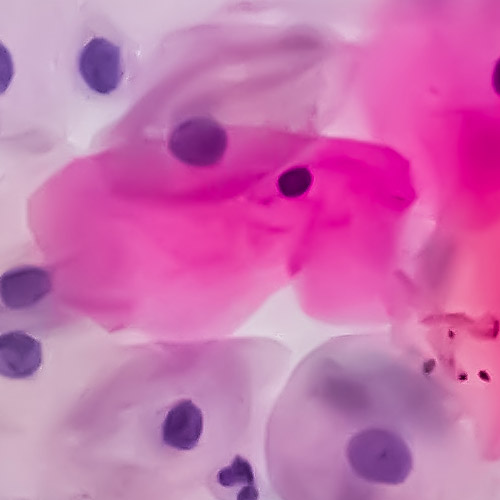
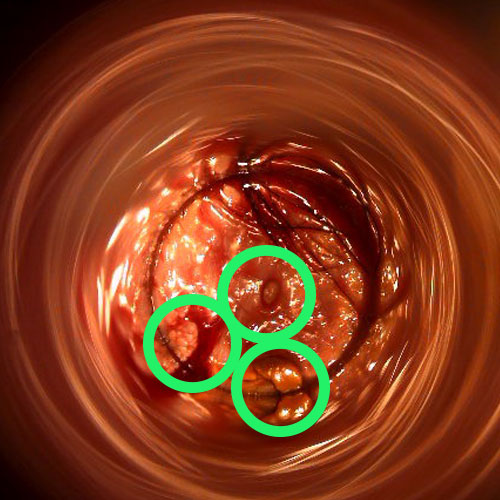
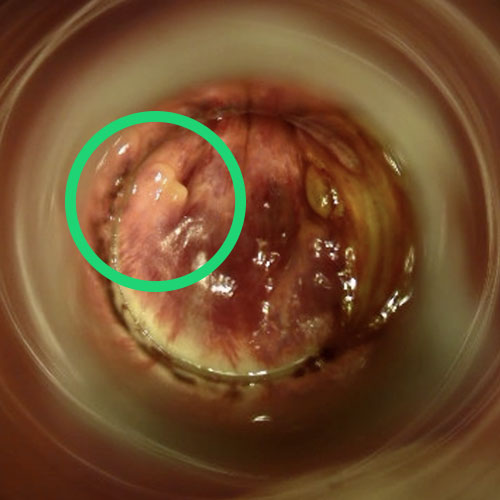
Anal condylomata appear as growths of varying shape and color, located around the anus or sometimes even inside it.
In fact, HPV infection can spread almost anywhere in the skin and mucosa, even reaching the rectal canal.
Their shape is essentially of two types: acuminate (also called 'cockscombs') or flat.
Their size is variable: from a few millimeters to even more than a centimeter, and their evolution cannot be predicted.
Their coloration varies from whitish/pinkish to brown/dark, again following unpredictable evolutions.
Apart from their presence as neoformations, anal condylomata rarely give rise to other symptoms, but in sporadic cases they can still give rise to anal irritation and itching.
This is because the anal mucosa, in an attempt to protect itself from the virus, increases mucus production, thus causing the phenomenon of wet anus, which leads to maceration of the skin, thus causing bothersome dermatitis.
Warts may rarely bleed, especially if present inside the anal canal, from laceration due to passage of stool.
How are anal warts diagnosed?
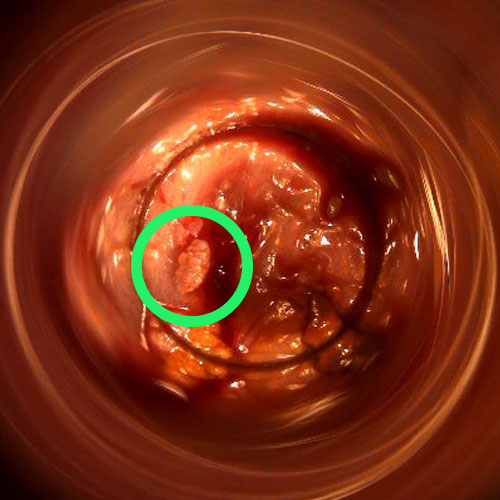
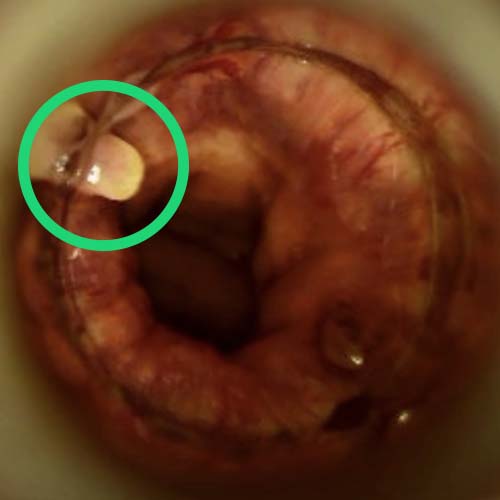
The diagnosis of anal condylomata is basically clinical, and is performed during the proctological examination.
A proctology examination, accompanied by Electronic Endoscopic Videoproscopy examination, is sufficient for the experienced proctology physician to diagnose condylomatous lesions.
Usually no other examinations are necessary, not even colonoscopy: the expansion of condylomata may afflict the mucosa of the rectum, but beyond that it does not go, so there is no need to investigate further with endoscopy.
However, the Proctology Physician may prescribe immunological investigations for the patient, usually including an HIV test, to assess the status of his or her immune system.
In the current state of Medicine, there is no specific antiviral therapy for HPV virus.
This means that it is the host's immune system that, in the long run, must defeat the virus, and stop the infection.
However, this can take time, during which it is good practice to help the body by decreasing the viral load contained (at very high levels) in anal warts.
Is there a treatment for HPV infection?
Currently, there is no specific antiviral treatment for HPV infection, so its eradication is left entirely to the host's immune system.
This makes that, of course as in all viral diseases, prevention is preferred in an absolute sense.
An effective and safe Papillomavirus vaccine has recently been developed and should be given to everyone (male and female) before the age of 15.
If infection has occurred, however, it is necessary to wait for the immune system to defeat the virus, even with the help of immunostimulant therapy.
Is there a treatment for anal warts?
Although there is no therapy to eradicate HPV infection, however, there are a variety of therapies to remove anal warts.
Such therapies can be essentially pharmacological (topical) or surgical.
Eradication of warts is always suggested to the patient, as they are true pre-tumor lesions that, although in rare cases, can degenerate into actual cancers in the long run.
This risk arises because, especially with some types of HPV virus, in the long run the presence of the antigen in the dermal cell can cause it to form tumors, giving rise to carcinoma.
Among topical therapies, administration of podophilin, an anti-tumor agent capable of destroying Papillomavirus-infected cells, is generally the first-line solution, at least for infections that are not too extensive.
Cryotherapy with liquid nitrogen can be practiced successfully, and it gives the best results when condylomatous lesions are confined to the peri-anal area.
Surgical therapy, on the other hand, becomes necessary when condylomata are located within the anorectal canal or when their size and extension are considerable.
The purpose of eradication surgery is to reclaim the diseased skin but, at the same time, also to avoid unnecessary scarring and pain for the patient.
To do this, any tools deemed most appropriate by the Surgeon can be used: the cold-blade scalpel, high-frequency laser, electrocautery, or even the plasma lance.
Can warts recur?

Like all warts caused by the HPV virus, condylomata can recur once removed.
This can happen regardless of the surgeon's skill in removing the lesions: some individual cells, not visible to the human eye and impossible to detect by any other method, may still remain during eradication, then giving rise to a new infection.
Statistically, recurrences of warts are very common: they usually appear within three months of eradication surgery, and although they may recur then even years later, their recurrence in the long term is less likely.
Do you think you are suffering from anal warts in Dubai? Dr. Luisella Troyer can help you

Dr. Luisella Troyer is a Proctologist Surgeon with experience in the diagnosis and treatment of anal condylomatosis.
In her clinic in Dubai, Dr. Troyer can accurately diagnose anal warts not only externally, but also internally, using Electronic Endoscopic Videoproctoscopy.
With Dr. Troyer you will also find all the latest medical and surgical therapies for eradication of anal warts.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- CONDYLOMATA ARE THE EXTREME RESPONSE OF OUR PHYSIQUE TO A PARTICULARLY AGGRESSIVE ATTACK GIVEN BY THE HUMAN PAPILLOMA VIRUS (HPV), WHICH IS NOT ADEQUATELY CONTROLLED BY THE IMMUNE SYSTEM;
- HPV IS AN OPPORTUNISTIC VIRUS THAT IS TRANSMITTED BY DIRECT CONTACT, ESPECIALLY THROUGH SEXUAL CONTACT;
- IN A HEALTHY, NONSMOKING INDIVIDUAL, HPV IS ESSENTIALLY ASYMPTOMATIC;
- CONDYLOMATA ARE FLESHY, FLAT OR SHARP LESIONS THAT ARE CONSIDERED PRE-CANCEROUS;
- CONDYLOMATA CAN OCCUR ANYWHERE ON THE SKIN OR MUCOSA, ANAL OR ORAL, AND USUALLY HAVE A TENDENCY TO FORM IN CLUSTERS;
- BEING PRE-CANCEROUS LESIONS, THERE IS A RISK, ALTHOUGH RARE, OF THEIR MALIGNANT DEGENERATION;
- SOME TYPES OF HPV ARE MORE ONCOLOGICAL THAN OTHERS;
- CONDYLOMAS OCCUR ALMOST EXCLUSIVELY IN IMMUNODEPRESSED PERSONS, MOMENTARILY OR TEMPORARILY, DUE TO ANTIBIOTIC TREATMENT, ONCOLOGY, PERIODS OF PARTICULAR STRESS OR TENSION, OR VICTIMS OF RECENT PREVIOUS BACTERIAL OR VIRAL INFECTION, WHICH HAS EXHAUSTED THE IMMUNE SYSTEM;
- THERE IS NO SPECIFIC ANTIVIRAL CURE FOR HPV, BUT THERE ARE EFFECTIVE TREATMENTS TO ERADICATE CONDYLOMATA;
- ANAL CONDYLOMAS CAN OCCUR ON THE EDGE OF THE ANAL ORIFICE, IN THE PERI-ANAL AREA , OR EVEN INSIDE THE ANAL CANAL TO THE RECTUM;
- TREATMENT FOR ERADICATION OF CONDYLOMATA CAN BE MEDICAL OR SURGICAL, DEPENDING ON THEIR LOCATION, QUANTITY, AND SIZE;
- CONDYLOMAS MAY RECUR AFTER TREATMENT, BUT THIS SHOULD NOT DISCOURAGE THE PATIENT: IN THE LONG RUN, ALL TREATMENTS ARE SUCCESSFUL IN ERADICATING THEM

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.