Diverticulitis is one of the most statistically frequent nonautoimmune-based inflammatory diseases and, along with anal fistula and perianal abscess, is among the major causes of emergency colonprotcology access.
f not treated promptly, diverticulitis can be life-threatening, causing major intestinal infections that, in severe cases, can lead to deep ulceration, with danger of intestinal sepsis.
Read this page to learn what diverticulitis is, how it can be diagnosed, what can be done to prevent it, and how it can be treated.
Diverticulosis is a physiologic condition that can be well diagnosed with virtual videocolonoscopy.
This examination, conceptually similar to traditional videocolonoscopy, is often preferable to the latter because of easier preparation for the patient.
What are diverticula?

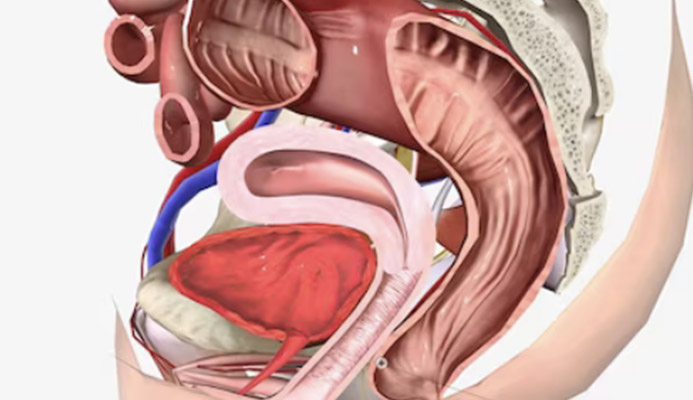
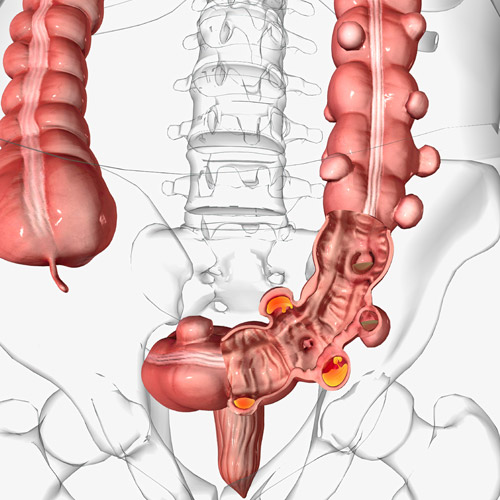
Diverticula are small sac-like anatomical conformations that can occur as protrusions of the mucosa and submucosa of the large intestine (the colon).
They are not a real pathology, rather an anatomical conformation, which may or may not be present, either as a congenital peculiarity or, no less, manifesting even in the adult part of life.
Their presence, therefore, is not necessarily symptomatic, and their observation is, in many cases, occasional, secondary to a colonoscopy that aims instead to investigate another issue.
The presence of diverticula in the colon, which is statistically shown to be greater in its descending part and in the sigma, is called diverticulosis.
Diverticulosis, it should be repeated, is not a pathological condition per se, and it does not give rise to any symptoms per se.
Only in case of precise processes of diverticulum inflammation can the term diverticulitis be used, which instead indicates a pathological condition of diverticulosis.
Why do diverticula occur?
There is still no precise explanation medically as to why diverticula are present in some people and not in others.
It should be clarified that diverticulosis can be congenital, thus naturally present at birth, or it can occur later, even in adulthood, with the peak of extrusion being greater in individuals over 50 years of age.
However, Medicine has proven, without any doubt, that the occurrence of diverticula in adulthood is related to diet and lifestyles.
Diets with excessive red meat, lack of adequate fiber, and sedentary lifestyle seem to promote the occurrence of diverticulosis, and this appears to be evident in the North American and European population, where diverticulosis appears in higher incidence than in the rest of the world.
Another theory that attempts to explain the occurrence of diverticula wants that a high pressure of the parts of the colon (endoluminal, in medical circles) may be responsible for the extrusion that gives rise to diverticula, although this does not have necessary connections with diet and lifestyles.
It should be specified that more than 80% of patients with diverticulosis have no problems of any kind in the intestines, nor do they compulsorily demonstrate the senses of diverticulitis.
What is diverticulitis?

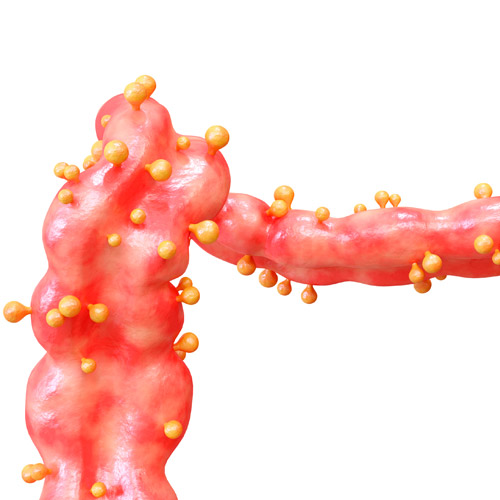
In contrast to diverticulosis, as mentioned an anatomical variation in itself asymptomatic of the mucosa of the colon, diverticulitis is instead a pathology, indicating inflammation, or infection, of one or more diverticula.
In 20% of cases, the origin of this infection is bacterial, while a non-negligible percentage is from the abuse of NSAID (non-steroidal anti-inflammatory) drugs.
Finally, a percentage varying between 30 percent and 40 percent is given by fecal debris, which, stuck in the diverticulum sacs, gives rise to inflammation of the mucosa, with stenosis of the small sacs and consequent lack of oxygenation, which, in severe cases, gives rise to true ulcers.
Diverticulitis occurs predominantly in individuals over 50, but can indifferently affect any person of any age with established diverticulosis.
What are the symptoms of diverticulitis?
The main symptom of diverticulitis is intense and acute abdominal pain, in Caucasian patients generally directed toward the left side of the colon, and in Asian patients toward the right side.
The pain appears suddenly, without warning, and immediately manifests as very sharp, often reported as comparable to that of renal colic.
Associated with pain are spasms, diarrhea (or constipation), nausea, vomiting and inappetence, hematochezia (blood from the anus during defecation), and fever, often high.
Nausea and abdominal pain greatly prostrate the patient, who routinely refuses both food and water.
The fever is often intermittent, and is associated with (or interspersed with) icy chills, which leave support for the septic origin of the temperature change.
In the most severe cases, requiring hospitalization and emergency surgery, there is perforation of the colon, with purulent material being released into the peritoneum as a result of the rupture of the diverticulum, thus resulting in peritonitis.
Such an inauspicious event requires immediate surgical intervention, and the risk of septicemia and subsequent death is always very high.
How is diverticulitis diagnosed?
Diagnosis of diverticulitis is not easy, as the symptoms are common to those of other diseases (e.g., gastrointestinal infection caused by bacteria or viruses, or even appendicitis).
A great help to the physician is to be aware or unaware of the patient's diverticulosis condition, but this information is often ignored by the patient.
Therefore, certain confirmation of the diagnosis is possible only by instrumental examination, which is abdominal and pelvic CT scan with water-soluble contrast.
This examination is of great clinical precision, and can accurately confirm the presence or absence of diverticular inflammation or infection.
Colonoscopy is not possible during an acute attack, but may be prescribed a few months after the inflammatory phase has resolved, more so to rule out the presence of any intestinal polyps or carcinomas.
In patients with established diverticulosis, colonoscopy is not an examination that can be performed as a periodic screening.
The presence or absence of diverticula is not affected by video examination, and diverticulum formations do not spontaneously regress, so colonoscopic inspection brings no real diagnostic benefit-in fact, it is often dangerous as it may even puncture one of the diverticula.
What is the treatment for diverticulitis?

Therapy for diverticulitis can change greatly depending on the origin of the inflammation or inflammation as well as its actual state of severity.
The use of antibiotic treatment, once practically always prescribed treatment, is now relegated only to complicated cases, as it has been found that in mild cases it is not only ineffective, but may also worsen the overall condition.
Mild cases of diverticulitis are treated with absolute rest and an exclusively liquid diet.
In case the patient presents with unbearable pain, very high fever that does not recede even with medication, and leukocytosis (i.e., a sustained and abnormal increase of leukocytes in the bloodstream) hospitalization is always mandatory.
In cases of confirmed abscess, minimally invasive CT-guided drainage can be used, which gives excellent results for diverticula greater than 2cm.
Surgery is relegated only to severe cases of diverticulitis, that is, when there is a perforation or burst diverticulum or when there is no improvement following drug or dietary therapy.
This usually occurs in 15% to 20% of cases.
Surgery may also be considered suitable following systematic recurrences of diverticulitis in areas of the colon that periodically become inflamed and do not respond to drug treatment.
Ways of surgical access change according to the surgeon's preference, but generally resection of the part of the colon affected by the infection is performed, with related anastomizing (suturing).
Temporary colostomy, i.e., temporary detour of the colon to an artificial external access, is reserved only for very severe cases with severe inflammation that does not allow safe anastomosis.
Which Physician should be referred to if diverticulitis is suspected?
Diverticulitis is a colonproctologic condition, so the Physician who specializes in diagnosing and treating it is the Colonproctology Surgeon.
However, the Gastroenterology Physician also has the expertise to intervene effectively.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- DIVERTICULA ARE SMALL SACS THAT EXTRUDE FROM THE INTESTINAL MUCOSA, CONSIDERED NONPATHOLOGICAL ANATOMICAL VARIATIONS;
- THE PRESENCE OF DIVERTICULA IN A HEALTHY INDIVIDUAL IS CALLED DIVERTICULOSIS, AND MAY BE PRESENT AT BIRTH OR OCCUR LATER, EVEN IN ADULTHOOD;
- IT IS UNCLEAR WHY DIVERTICULA FORM, BUT ONE OF THE MOST PLAUSIBLE THEORIES INVOLVES INCREASED ENDOLUMINAL PRESSURE CAUSED BY LIFESTYLES AND DIET;
- DIVERTICULITIS IS THE INFLAMMATION OR INFECTION OF ONE OR MORE DIVERTICULA, CAUSED BY A RESIDUAL ORGANIC FRAGMENT OF FOOD, OR EVEN FECES, INSERTING ITSELF INTO A DIVERTICULAR SAC, TRIGGERING INFLAMMATION;
- DIVERTICULITIS OCCURS MAINLY IN INDIVIDUALS OVER 50;
- THE SYMPTOMATOLOGY OF DIVERTICULITIS OCCURS SUDDENLY, WITH SEVERE ABDOMINAL PAIN, DIARRHEA, VOMITING, FEVER, POOR APPETITE, AND SOMETIMES ANAL BLEEDING;
- THERAPY FOR DIVERTICULITIS IS LIQUID DIET AND REST, BUT IF THERE IS PERFORATION OR BURSTING OF A DIVERTICULUM, SURGERY IS NECESSARY

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.