Do you experience bright red bleeding every time you take a bowel movement, perhaps accompanied by burning and discomfort?
Is this blood found on toilet paper, on feces, or even in the toilet bowl, because maybe it drips directly from the anus?
The color of bright red blood on toilet paper and stool often puts genuine terror in the patient, who often thinks he or she is afflicted with malignant diseases, such as colon and rectal cancer.
In fact, statistics say that most episodes of hematochezia, that is, the anal bleeding that typically occurs after evacuation, are attributable to prolapsed hemorrhoids.
If you've panicked after seeing bright red blood on your stool or toilet paper, try to remain calm: book a proctology visit and, in the meantime, read this article written for you by Dr. Luisella Troyer, Proctology Surgeon in Dubai.
There are some jobs that playfully require long periods of standing, in what is called orthostatic position.
Jobs such as, for example, cooking, hairdressing, and bartendingoften needorthostatic position for hours on end, with minimal muscle movement.
This is not good for the tissues of the anorectal canal, which, due to the force of gravity, tend to exhaust and prolapse downward, especially in individuals who are no longer very young.
This can be a trigger for the onset of hemorrhoidal pathology.
What are hemorrhoids?

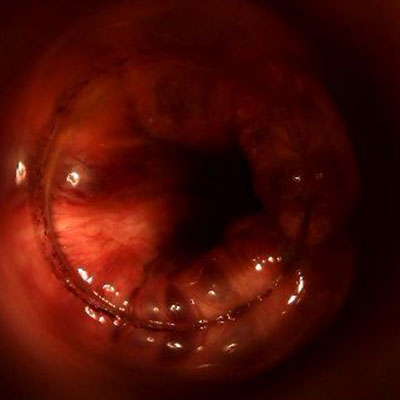
Hemorrhoids are small pads formed by veins and arteries joined together, located inside the anal canal.
We all have three main hemorrhoid plexuses: right anterior, right posterior, and left lateral, to which are added a couple of smaller secondary plexuses.
The physiological task of hemorrhoids is the proper vascularization of the anorectal canal and, to a lesser extent, also to aid the sphincter muscles for fecal containment.
Under normal conditions, therefore, it is completely normal to 'have hemorrhoids', as they are anatomical elements naturally present from our birth.
Only in the event that the hemorrhoids should, for a long series of reasons, extrude, become inflamed, swell, or tear, can we speak of hemorrhoidal disease, which is a real pathology.
Why do hemorrhoids become pathological and give problems?
In Medicine, we speak of 'hemorrhoidal disease' exclusively when hemorrhoids begin to give obvious symptoms, both at the Physician's inspection and in relation to symptomatology for the patient.
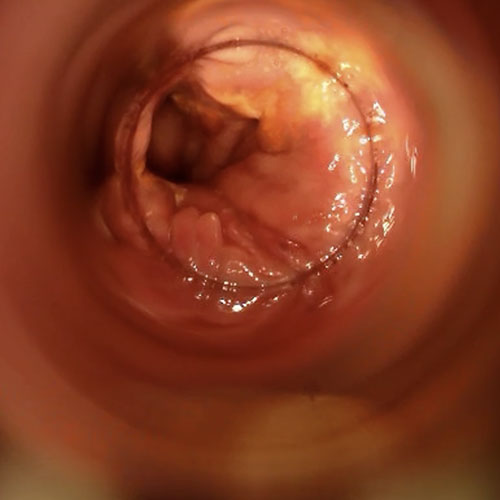
This hemorrhoidal disease presents as a slow but steady prolapse of the hemorrhoidal plexuses, resulting in their swelling.
This causes the hemorrhoids to escape from their seat in the anal canal and, by the gravitational pull, to prolapse downward out of the anal orifice.
Such prolapse is usually slow, but inexorable once initiated and not treated expeditiously with the right medical therapy: the hemorrhoids swell and prolapse outward more and more, often reaching truly critical cases of great pain and suffering for the patient.
The exact cause of the onset of hemorrhoidal prolapse is not yet fully known to science, and there is no unified opinion in the scientific community.
For years now, two main theories have been proposed that attempt to explain why hemorrhoids swell and begin to prolapse:
- The mechanical theory, which hypothesizes natural tissue failure due to declining collagen, natural aging, and specific triggers that increase intraabdominal pressure (such as chronic constipation);
- The hemodynamic theory, which hypothesizes a swelling of the plexuses due to an incontinence of the internal tissues of the plexuses, not very dissimilar to that which causes chronic venous insufficiency, and which can lead to a fragility of the internal walls of the hemorrhoids and their exhaustion by blood pressure, which thus causes them to prolapse
It is good to note that the two theories, however, are not necessarily at odds with each other, and may in fact be both sides of the same coin.
What are the triggers of hemorrhoids?
The two hypothesized main theories as to why hemorrhoids begin to prolapse, however, require what are called 'triggers', that is, concrete and real concauses for the hemorrhoid plexuses to become exhausted, initiating their prolapse.
These triggers have been known to Medicine for many years, and they are:
- Chronic constipation;
- Chronic diarrhea;
- A diet low in adequate hydration and fiber;
- Pregnancy and childbirth;
- Some laborious, particularly wearing jobs;
- Some professions where, playfully, one is forced to stand and stand still for long periods of time;
- Some sports, such as weightlifting, cycling and motorcycling;
- Some bad habits, such as spending too much time on the toilet reading or straining to go bodily
These triggers are the ones that, if the patient is predisposed, usually initiate hemorrhoidal disease.
Bright red bleeding during defecation is always a symptom of injury to the anorectal canal or, at any rate, to thefinal part of the intestine.
This is because injuries to the upper intestine, thus toward the cecum or ascending colon, result in inevitable digestion of blood, which thus becomes dark, sometimes almost clotted.
It must be said, however, that although anal bleeding is a typical symptom of hemorrhoids, they are not the only absolute cause: there are also many other diseases that can injure the anorectal mucosa, such as anal fissure, ulcerative rectocolitis, mucosal polyps or even the presence of condylomata.
That is why, in case of bleeding during evacuation, it is always advisable to have a specialized proctological examination.
Why do hemorrhoids bleed?
Hemorrhoids prolapsed out of their original anatomical location are easily injured by stool transiting the anorectal canal.
Passing feces, laden with bacteria and bacterial fermentation material, especially if they are too hard, injure the hemorrhoids and cause genuine wounds, which give rise to anal bleeding.
Such bleeding usually occurs during evacuation or soon after, and the obvious symptom is bright red blood stains on toilet paper, stool, or even a trickle of blood on the toilet.
Sometimes the bleeding is present in the form of streaks in the stool, other times, especially in cases of high grade hemorrhoidal prolapse (grade IV irreducible even with manual maneuvering), bleeding may occur spontaneously even without evacuation, only with friction of the hemorrhoids with the clothing.
In medical jargon, anal bleeding is called hematochezia, and it is an episode that greatly frightens the patient and causes him to think that he is carrying some non-benign disease of the rectum or anus.
When the bleeding is really profuse, much like a hemorrhage, it is called rectorrhagia.
Fortunately, episodes of rectorrhagia attributable to hemorrhoids are decidedly rare, and much more common are small daily losses on evacuation, falling under simple hematochezia.
Is bright red blood from the anus a good sign?

Any anal bleeding is suspicious and should be investigated.
Leaking blood from the anus, a little or a lot, during or shortly after defecation is not natural, and always indicates the presence of an intestinal injury.
The large intestine, i.e., the colon, is a long, wide tube about 7 meters long that can suffer from many diseases, benign and otherwise.
Any part of its delicate inner mucosa can become injured, and for a wide variety of reasons: from inflammatory states to cancerous lesions, the possible causes of intestinal injury are many indeed.
Usually, the presence of bright red blood during or immediately after defecation means that the wound that surely occurred, however, concerns the last part of the intestine, and not an upper tract of the intestine.
Generally, lesions present in the small intestine or in the first parts of the colon, i.e., the ascending colon and transverse colon, give as a symptom the emission of black, almost clotted blood, a sign of the digestion that took place on the long journey to the anus.
Although, in itself, blood coming out of the anus is never a 'good sign', statistics tell us that it is almost always due to a benign pathology of the anorectal canal, such as precisely pathological hemorrhoids or, sometimes, anal fissure.
This may not deter the patient from making the necessary proctologic examination to truly ascertain the benign diagnosis: although more rarely, hematochezia may be the warning light of situations deserving immediate treatment, such as carcinoma of the rectum and anus, or dangerous diverticulosis.
Is there a severity scale for hemorrhoids?

Yes, conventionally hemorrhoids are divided into four stages of severity, depending on the volume of their prolapse:
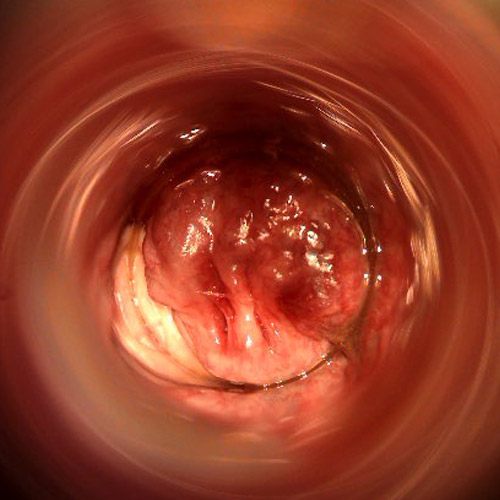
- Grade I hemorrhoids, hemorrhoids inside the anal canal, detectable are by proctoscopy;
- Grade II hemorrhoids, hemorrhoids that extrude from the anal canal only during evacuation ponzament, or under some strains, but immediately reenter the canal spontaneously;
- Grade III hemorrhoids, hemorrhoids that extrude from the anal canal but can still be reinserted in with a manual maneuver;
- Grade IV hemorrhoids, hemorrhoids that extrude completely outside the anal canal and are no longer reducible within, even with appropriate manual maneuvering
Obviously, this severity scale is an indicative outline: some hemorrhoid stages are not categorically defined, and there are 'ring' severity situations between stages.
How can hemorrhoids be treated?

Treatment for hemorrhoids varies according to their severity status.
Low-grade hemorrhoidal prolapses, especially in individuals who are still young and in whom tissue collagen production is still excellent, can be reduced with the right diet, pharmacological decongestion of the anal area, and the use of flavonoid supplements.
Often in fact, those who suffer from mild, yet chronic, hemorrhoid prolapses also turn out to have widespread anitis and proctitis (the inflammation of the anorectal canal), which worsens the condition of the mucosa and does not allow the tissues to regenerate, thus fueling hemorrhoid congestion.
By flushing the area and ensuring that the patient provides regular normoformed and soft evacuations, low-grade hemorrhoids often recede, causing their symptoms to also recede.
High degrees of hemorrhoids, or those that do not respond adequately to drug treatment, always require medical or surgical intervention.
The treatments available for chronic hemorrhoids are essentially of two types: conservative or radical.
Conservative treatments, as the name otherwise implies, aim to reduce the symptomatology and volume of prolapse, but leave the tissues of the hemorrhoid plexuses intact.
These are generally useful treatments only for mild stages, in which the hemorrhoid tissues have not yet fully exhausted.
Among conservative treatments we can mention:
- Hemorrhoidal ligation, a now obsolete, quite painful technique in which the hemorrhoidal gavage is tied by an elastic band at the base.
Such a rubber band causes a constriction of the arterial circulation, resulting in necrosis of the plexus and detachment of the plexus;
- HeLP technique, where the hemorrhoids remain intact, but the arterioles that supply the plexuses are cauterized, by laser.
The technique, on which many hopes were placed when it was first released, has not yielded the desired results, and the high number of recurrences advises against its use on hemorrhoid stages beyond grade II;
- Cryotherapy, in which hemorrhoids are frozen by means of nitrogen.
A fairly painful technique, again from the high number of recurrences, which has been essentially abandoned in recent times
Radical treatments, on the other hand, are all treatments that involve the destruction or removal of the hemorrhoidal plexuses.
These treatments are the only viable treatments for those with high-grade hemorrhoids, or for those with low-grade hemorrhoids who have not reported benefit from drug treatment.
Radical treatments for hemorrhoids are:
- Hemorrhoidectomy according to Milligan-Morgan, which is the surgical removal of the hemorrhoid plexuses according to the protocol invented, more than a century ago, by the British Doctors Milligan and Morgan.
The hemorrhoids are tied at the base of the gavage and the artery supplying them cauterized, after which the plexuses are surgically removed, including the mucosa adjacent to them.
The wounds are not sutured, but left free to heal by second intention.
Healing occurs in about three months, and the postoperative course can be uncomfortable for the patient, as the open lesions come, playfully, into contact with bacteria from the stool adorned evacuation.
Until the advent of the new sclerotherapy with scleromousse, this type of surgery was the only one possible to treat severe cases of hemorrhoidal prolapse;
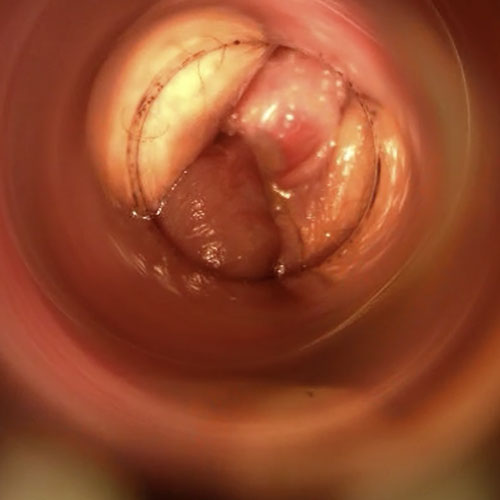
- Sclerotherapy with sterile air-stabilized scleromousse, in which hemorrhoids are destroyed (sclerotized, in the medical setting) by a mousse containing sterile air and polidocanol, an alcohol-based drug.
This mousse, produced on the spot by the Physician by means of special pumps that sterilize the air, clings to the internal walls of the hemorrhoids and causes their chemical inflammation, which destroys the internal tissues, and causes retraction of the plexuses.
Along with the hemorrhoids, the mucosa above them also recedes, so there is a double operative benefit.
Three injections of mousse are usually required to complete the treatment, but the number varies from patient to patient.
This treatment is not painful, is quick, and has success rates comparable to those of hemorrhoidectomy (over 95%), thus allowing a drastic reduction in costs and an enormously smoother post-surgery for the patient
The choice of one treatment over another is decided by the proctology physician after evaluating the patient's condition during the specialized proctological examination.
Can hemorrhoids be cured permanently?

Yes, healing from hemorrhoidal prolapse is not only possible but is always recommended to the patient.
Prolapsed hemorrhoids are a pathological and unnatural condition: although their bleeding upon defecation is nonetheless modest, and (apart from very rare cases) not life-threatening, recurrent infections and inflammations of the anal area are still possible, giving rise to frequent proctitis and anitis.
Again, the bruised hemorrhoids can easily thrombize, resulting in an extremely painful and very time-consuming hemorrhoidal crisis.
In the long run, the more prolapse increases the more discomfort and suffering for the patient: bleeding becomes more frequent and copious, anal itching becomes chronic (the result of proctitis caused by bacterial attacks and overproduction of mucus), episodes of hemorrhoidal crisis more likely and increasingly painful.
That is why it would be recommended not to hesitate too much about the problem, and not to delay the mandatory proctological examination performed by an experienced and trained Proctology Physician.
Very often, many patients, out of unwarranted fear or shame, put off seeing the doctor to the extreme, resorting to it only when the situation has become untenable.
This is always to be avoided, since great prolapses, in addition to the great suffering they bring, perforce then necessitate more vigorous and, game-changingly, more expensive and time-consuming therapies.
Can there be any benefit to using soothing ointments for hemorrhoids?

Hemorrhoids and their prolapse are a mechanical and vascular problem.
Prolapse begins due to the wearing away of the supporting structures of the plexuses (i.e., the collagen-rich tissues that hold the hemorrhoids attached to the anal wall), and worsens with increased blood supply, and the associated swelling of the hemorrhoid pads, which always tends to worsen over time.
As long as hemorrhoids are supplied by arterial blood and the structures containing them are incontinent - not unlike leg varicose veins - the problem can never be resolved.
Creams and ointments for hemorrhoids are designed and sold for soothing and symptomatic purpose:they have no curative power whatsoever over the origin of prolapse, but at best give momentary relief from symptoms.
Some ointments, of excellent quality and with natural active ingredients, are useful because, by soothing the inflamed mucosa, they allow decongestion of the plexuses, and this can lead, when combined with the right diet and the administration of specific medications, to a remission of small hemorrhoid stages, especially in young subjects.
For advanced hemorrhoid stages, or for uncontested but now large volume hemorrhoids, soothing ointments are of little use.
Some ointments, especially those sold with large advertising budgets and thumping promotional campaigns, give illusory and momentary benefit because, within them, they have a small percentage of lidocaine, a local anesthetic that temporarily soothes the pain and discomfort of congested and inflamed plexuses.
However, the well-being is short-lived, and when the anesthetic's effect is over, the situation returns as before.
That is why, in the event of the onset of hemorrhoidal prolapse, creams and ointments shouldn't never be self-prescribed cures
Can bleeding after defecation also be a symptom of other diseases?
Bleeding during evacuation is a wake-up call, signifying that somewhere in the intestines there is an injury.
Pathological hemorrhoids are not the only cause of bleeding, although they are definitely the most common cause of it.
There are other pathological conditions, some not benign, that can lead to hematochezia, and therefore the patient should never underestimate or minimize this symptom.
Among the possible causes of anal bleeding, we can briefly mention:
- The presence of polyps in the intestine or anorectal canal;
- The presence of condylomatous lesions;
- The presence of anal fissures;
- Violent proctitis, with lacerations of the anorectal mucosa;
- Crohn's disease;
- Ulcerative rectocolitis;
- Carcinoma of the intestine or rectum;
- Diverticulosis;
- A bowel injury, etc.
Which Physician should be consulted in case of blood loss from the anus?

The health specialist with expertise in pathological hemorrhoids and, in general, all colonproctological problems is the Proctologist Surgeon.
Usually, given that hemorrhoidal prolapse is an exquisitely vascular problem, the Proctologist Surgeon is a Physician specializing in Vascular Surgery, but can also be a specialist from Geastroenterology or General Surgery.
Do you bleed when you have a bowel movement? Don't be alarmed, but contact Dr. Luisella Troyer

Dr. Luisella Troyer is a Proctology Surgeon in Dubai, specializing in Vascular Surgery.
Dr. is an expert in the diagnosis and treatment of pathological hemorrhoids, including advanced techniques such as sclerosing treatment with sterile air-stabilized scleromousse.
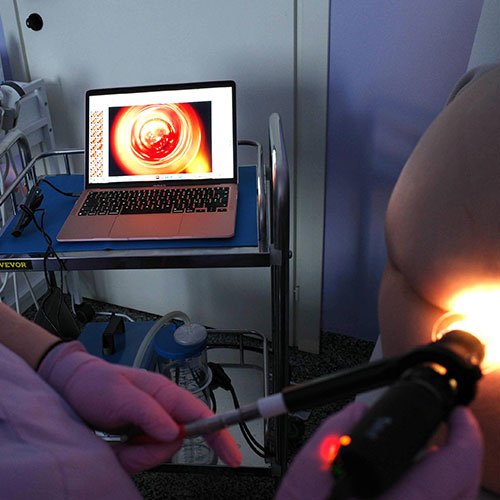
In her clinic in Dubai, Dr. Troyer can diagnose your hemorrhoidal prolapse totally painlessly, thanks to the use of the electronic videoproctoscope.
You can then not only get the right diagnosis for your anal bleeding, but also begin to treat it and stop having burning and discomfort with every evacuation.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- HEMORRHOIDS ARE NATURAL ARTERIOVENOUS PLEXUSES PRESENT IN OUR ANAL CANAL;
- THE JOB OF THE HEMORRHOIDS IS TO PROPERLY VASCULARIZE THE ANAL CANAL AND, TO A LESSER EXTENT, TO ASSIST THE SPHINCTERS IN FECAL CONTINENCE;
- HEMORRHOIDS BECOME A PROBLEM ONLY WHEN THEY BECOME INFLAMED AND EXTRUDE FROM THEIR ORIGINAL SITE, GIVING RISE TO HEMORRHOIDAL PATHOLOGY;
- THERE ARE DIFFERENT DEGREES OF HEMORRHOIDS, DEPENDING ON THEIR PROLAPSE AND VOLUME;
- THE TRIGGERS OF PATHOLOGICAL HEMORRHOIDS ARE CHRONIC CONSTIPATION, CHRONIC DIARRHEA, SMOKING, PREGNANCY AND CHILDBIRTH, OVERWEIGHT OR OBESITY, SOME STRENUOUS JOBS OR SOME SPORTS THAT INCREASE INTRA-ABDOMINAL PRESSURE;
- OFTEN, OUT OF SHAME OR FEAR, THE PATIENT DELAYS PROCTOLOGICAL EXAMINATION AND TREATMENT, RESORTING TO THE DOCTOR ONLY WHEN THE PROLAPSE SITUATION IS VERY SERIOUS;
- BLEEDING DURING EVACUATION IS A TYPICAL SYMPTOM OF HEMORRHOIDAL DISEASE;
- ANAL BLEEDING DUE TO HEMORRHOIDS IS USUALLYBRIGHT RED IN COLOR, MORE OR LESS INTENSE;
- ANAL BLEEDING IS MEDICALLY CALLED HEMATOCHEZIA, AND SHOULD ALWAYS RAISE SUSPICION OF AN INTESTINAL OR ANORECTAL CANAL INJURY;
- THE DIAGNOSIS OF PATHOLOGIC HEMORRHOIDS REQUIRES SPECIALIZED PROCTOLOGIC EXAMINATION, WITH THE NECESSARY ELECTRONIC ENDOSCOPIC VIDEOPROCTOSCOPY;
- MILLIGAN-MORGAN HEMORRHOIDECTOMY IS OFTEN BEING REPLACED BY THE NEW STERILIZED AIR-STABILIZED SCLEROMOUSSE SCLEROTHERAPY;
- IF WELL TREATED, HEMORRHOIDS NOT ONLY RECEDE BUT ARE PERMANENTLY ELIMINATED

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.

















