Do you suffer from burning, pain and bleeding when you go to the body?
Do you notice traces of bright red blood on the toilet paper, and feel strange growths around your anus?
Pathological hemorrhoids are the most common disease in the world, second only to dental caries.
They are a problem that can affect everyone, that has many causes and triggers, and that is often underestimated by the patient, who only turns to the Physician when the situation has become unbearable.
Read this page written by Dr. Luisella Troyer, Proctologist Surgeon, to understand what pathological hemorrhoids originate from, how they are diagnosed, and what can be done, medically or surgically, to treat and resolve them.
Hemorrhoids and their prolapse are, along with dental caries, the number one disease in the world.
This alone should give an idea of the numbers of hemorrhoidal disease, which does not look social status or ethnicity in the face, and affects millions of people every year.
However, this is in contrast to the number of treatmentsieffectivelydelivered to combat it, especially in advanced health care countries such as Italy.
In fact, not all patients with hemorrhoids turn to the Proctologist to treat them, but rather, they often delay treatment until the very last, when the situation is now very compromised.
What are hemorrhoids?

Hemorrhoids are athero-venous plexuses, resembling soft pads, located within the anal canal.
They are not arteries and are not veins proper, but are a mixture of them joined seamlessly (anastomosed, in medical jargon).
Their main function is to provide of adequate nutrition and oxygenation to the tissues of the anal canal and, secondarily, to participate in fecal containment.
There are three main hemorrhoidal pads, recognized by their location in the anal canal: right anterior, right posterior, and left lateral hemorrhoids.
In addition to these three main plexuses, there are two secondary, smaller hemorrhoids.
In normal situations, hemorrhoids do not give any problems, and they remain well inside the anal canal, so their presence is not even perceived.
Only when, due to a variety of causes and triggers, they increase in volume and prolapse out of their original location, we can speak of hemorrhoidal pathology, or pathological hemorrhoids.
What is hemorrhoidal pathology?
Hemorrhoidal pathology is the condition of abnormality of the hemorrhoidal plexuses that, due to different triggers and physiological causes, prolapse out of their original position, swelling and giving rise to a very specific symptomatology.
Swelling with blood, hemorrhoids increase in volume and extrude from their original anatomical bed, slowly prolapsing out of the anus.
This prolapse causes a variety of symptoms, sometimes very disabling: bleeding during defecation (hematochezia), burning, sense of swelling and foreign body in the anus, and often severe cases of intense pain due to thrombization of one or more hemorrhoidal plexuses.
Contrary to popular misconception, low-stage hemorrhoids can be effectively treated with the right anti-inflammatoryand anti-congestant therapy, combined with an appropriate diet.
If caught early, low-stage hemorrhoids can be treated with little difficulty and no pain, so it is important to diagnose them as early as possible and begin treatment immediately.
What are the actual causes of hemorrhoidal prolapse?

The actual causes of extrusion and prolapse of hemorrhoids are still being studied by Medicine.
At present, there are two main hypotheses that can help explain the phenomenon:
- The hemodynamic theory, which hypothesizes a slow exhaustion of the internal tissues of the hemorrhoids caused by increased blood pressure in the plexuses themselves (such as that which occurs during childbirth, during efforts to defecate, in certain types of sports or activities, etc.);
- The mechanical theory, which hypothesizes a physiological slow exhaustion of tissues by tissue aging and abdominal hyper-pressure, which converge pathological hemorrhoids into the broad spectrum of pathologies caused by pelvic floor prolapse
One theory does not exclude the other, however: they can scientifically coexist, and both can be causes of hemorrhoidal prolapse.
Associated with these two hypothesized main causes are also well-known triggers of hemorrhoidal disease, long known to science, which are:
- Chronic constipation or chronic diarrhea;
- Obesity or overweight;
- Multiple parts;
- Familiarity with chronic venous insufficiency (the varices);
- Feeding imbalances causing abnormal stool changes;
- Some types of sports, such as horseback riding, motorcycling and weightlifting
Root causes and triggers can obviously mix, increasing the risk of the onset of hemorrhoidal prolapse and, substantially, aggravating it.
What are the most obvious symptoms of pathological hemorrhoids?

Pathologic hemorrhoids can present with a wide range of symptoms, which can often be confused with other, not quite benign, diseases.
That is why, when in doubt, it is always a good idea to have a specialized proctological examination, with a complementary proctoscopy.
That being said, the symptoms reported by patients as most frequent in the case of pathological hemorrhoids are:
- Anal bleeding during or shortly after defecation (hematochezia), leaving traces on stool or streaks on toilet paper;
- Anal itching;
- Anal tenesmus, this is the feeling of never having emptied completely after defecation;
- Prolapse and extrusion of the hemorrhoids, which, often together with the anorectal mucosa, protrude from the anus, remaining outside it until manually repositioned or, in severe cases, permanently;
- Anitis, that is, inflammation of the peri-anal skin and anal mucosa;
- Pain, usually present in cases of thrombosed external hemorrhoids or in conjunction with anal fissure
All of these symptoms are not always present, and the severity of these symptoms is often directly proportional to the degree of hemorrhoid prolapse.
The so-called pectinate line, also called the pectinea line or dentate line, is the area where the rectum ends, and the short anal canal begins, which then leads to the orifice.
The pectinate line is so called because the anal papillae that form its mucosa have the unusual appearance of being almost oblong, forming a circle around the anorectal canal that resembles, precisely, a comb (or a series of long teeth).
Its anatomical importance is relevant, in Colon-Proctologic Surgery: in fact, beyond it, then toward the rectum and deep bowel, pain receptors are completely absent, and therefore the patient can endure without discomfort any proctologic procedures, even without anesthesia.
For example, sclerosing therapy with scleromousse for hemorrhoid reduction is performed precisely by taking advantage of the absence of pain receptors, as the injection into the hemorrhoid plexuses is performed well beyond the pectinate line.
What are SO CALLED complicated hemorrhoids?
In Proctology, we talk about complicated hemorrhoids when hemorrhoidal prolapse is accompanied by other problems that complicate the clinical picture, worsening the situation for the patient.
Such problems may be the concomitant presence of an anal fissure, anal warts, or a hemorrhoidal thrombus.
These complications can worsen the symptomatology of hemorrhoids, and make their treatment more hostile, which often needs to be supplemented with other specific therapy.
Is there a severity scale for hemorrhoids?
Yes, conventionally, pathological hemorrhoids are classified according to an increasing scale of severity, based on their prolapse status:
Grade I hemorrhoids
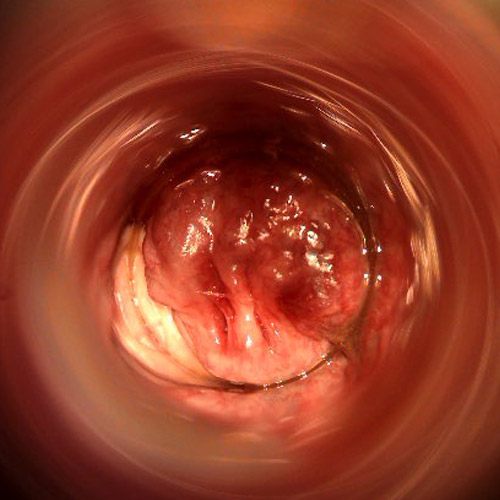
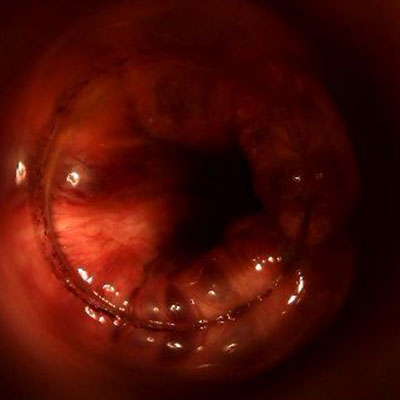
Hemorrhoids still reside in the anal canal, prolapsed hemorrhoids are invisible externally, and can only be observed with videoproctoscopy;
Grade II hemorrhoids
Prolapsed hemorrhoids exit the anal canal only during defecation, or only during excessive straining, and then spontaneously re-enter as soon as the abdominal pressing act is finished;
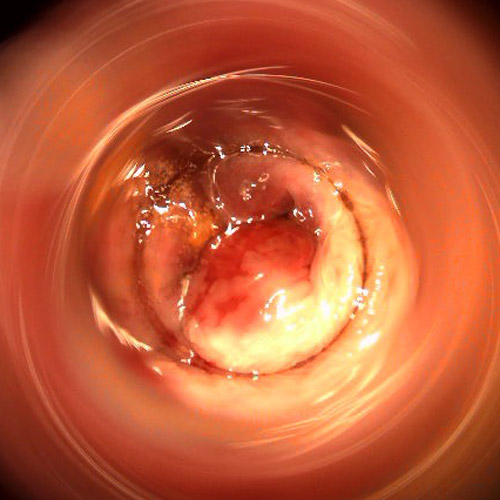
Grade III hemorrhoids
Hemorrhoids leak from the anal canal even without effort, but are able to re-enter with manual repositioning;
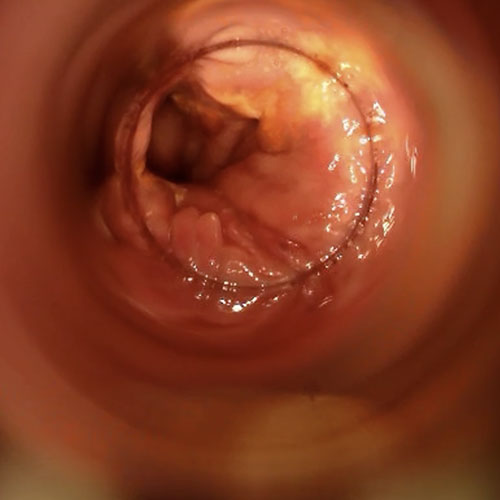
Grade IV hemorrhoids
Hemorrhoids are permanently prolapsed outside the anal canal, and do not return even with manual repositioning.
Of course, similarly to other diseases, there are ranges of severity between grades, and often the patient's actual condition straddles two stages.
One should always pay close attention to advertisements, both on television and in any other media, pertaining to phantom 'hemorrhoid creams.'
These advertisements always omit to say that any hemorrhoid prolapse cream, at best, can only have palliative effects, and never curative.
This is because prolapse of hemorrhoids is caused by the wearing away of their tissues, which in turn is generated by intra-abdominal hyper-pressure.
No cream in the world can reverse what is an exquisitely mechanical problem.
Many creams for hemorrhoids, usually over-the-counter products, give only a palliative feeling of well-being solely because of their small content of lidocaine (an anesthetic), which thus gives momentary relief to patients.
But, of course, once the anesthetic has worn off, the discomfort recurs, unchanged.
How are pathological hemorrhoids diagnosed?

Pathologic hemorrhoids are diagnosed quite simply by a proctologic examination.
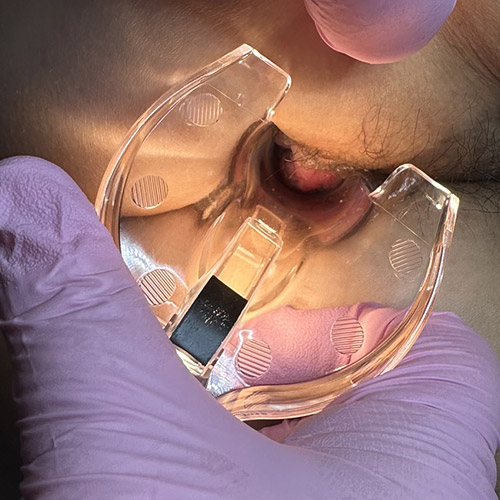
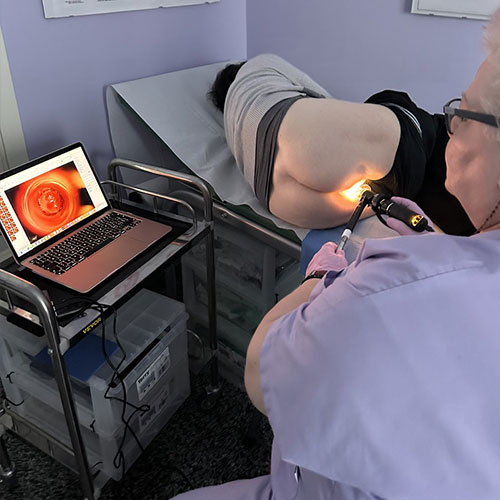
This examination is carried out by the Proctologist, and is based not only on clinical examination but also on a special instrumental examination called proctoscopy.
In the proctoscopy examination, which nowadays advanced medical offices perform digitally, by means of videoproctoscopy, the proctologist inspects the entire anorectal canal with a video camera, detecting not only external and visible hemorrhoids, but especially internal ones, even in the early stages.
Videoproctoscopy, which magnifies the anorectal canal by an average of 20X, is the only useful examination to diagnose internal, grade I hemorrhoids.
What are the treatments for pathological hemorrhoids?

Pathological hemorrhoids have, for millennia, plagued human beings.
Their symptomatology was already known to Hippocrates of Koos, the legendary father of modern Medicine, who had already guessed their nature as a vascular problem of blood overflow, and proposed the first (quite bloody) surgical treatments.
This preamble to say that, over the centuries, countless therapies, some decidedly imaginative and some extremely painful, have been used to try to solve the problem of hemorrhoidal prolapse.
Equally numerous are the current therapies available from modern Medicine and Surgery, which can be summarized succinctly into conservative therapies and radical therapies.
The choice of the right treatment approach is decided by the Proctologist Physician and is based on a thoughtful analysis of the patient's situation, considering the actual status of the hemorrhoidal prolapse.
Conservative therapies, as the name implies, aim to reduce the volume of the hemorrhoids, then retract them, while still maintaining their original anatomical structure.
Their use is effective in mild stages of hemorrhoids, stage I or II (rarely stage III), while it is not recommended in advanced stages.
These are treatments that have the virtue of mini-invasiveness: they have a rapid or very rapid recovery time, and can usually be performed on an outpatient basis as well.
Conversely, because they are not radical but conservative treatments, they can give rise to recurrences of hemorrhoidal prolapse.
Minimally invasive techniques include:
- Elastic binding;
- The HeLP technique (the selective dearterization).
- Infrared coagulation;
- Cryo-therapy
Radical techniques, on the other hand, aim to remove the root of the problem by removing all the hemorrhoidal plexuses.
This type of surgery, called hemorrhoidectomy, was first developed by British Doctors Dr. Milligan and Dr. Morgan, and more than a hundred years after the protocol was standardized, it is still used virtually unchanged, under the name hemorrhoidectomy according to Milligan-Morgan.
Hemorrhoidectomy is a radical procedure with a low recurrence rate (if well performed) and definitive, but it has all the typical disadvantages of surgical access, including a postoperative course that is not always smooth for the patient.
Then there is a third route for the treatment of hemorrhoids, which has similar characteristics to radical surgery but can be performed on an outpatient basis, with a very smooth and painless postoperative course.
It is sclerotization by sterilized air-stabilized scleromousse, a modern and innovative treatment that has been supplanting minimally invasive techniques for the past few years and is also playing a role as a viable alternative to hemorrhoidectomy.
What is scleromousse for the treatment of hemorrhoids?

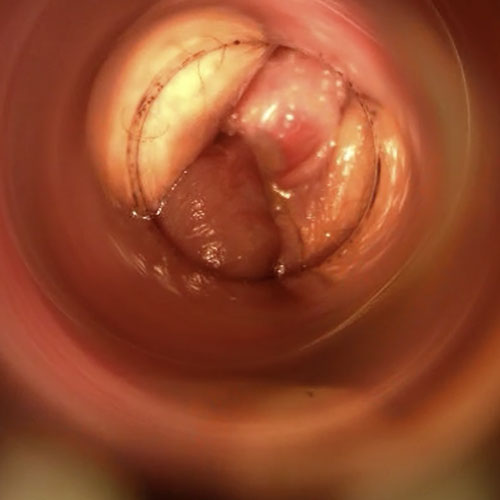
Sclerotizing scleromousse treatment is an outpatient medical treatment to permanently solve the problem of prolapsed hemorrhoids, including high-grade ones.
It is based on the injection, directly into the hemorrhoidal gavage, of a mousse composed of polidocanol and previously sterilized air, mixed with a special pump.
This mousse, injected inside the hemorrhoids, causes a chemical irritation of the endothelium, i.e., the inner tissue of the plexuses, which shrinks until it closes completely (it sclerotizes, medical jargon said).
Sclerotization of the hemorrhoidal plexuses results in recession of the prolapse, and with it the anal mucosa, effectively eliminating the problem of hemorrhoids at the root, without the need for Surgery.
Is scleromousse treatment for hemorrhoids effective?
Sclerosing treatment with stabilized scleromousse is extremely effective: medical statistics report a success rate of over 95%.
A statistic comparable to that of Milligan-Morgan hemorrhoidectomy, but without the postoperative discomfort of the same.
How many sclermousse sessions does it take to eliminate hemorrhoids?

The total number of scleromousse sessions is decided by the Proctologist Physician after the proctological examination, and depends largely on the degree of plexus prolapse.
Usually, at least three sessions are needed, carried out about 10 to 14 days apart.
The patient, however, need not worry about the total number of sessions, as each is painless anyway, with instant returns to daily activity.
Is it true that low-grade hemorrhoids can be resolved with the right diet and medical therapy?
Yes, low grade hemorrhoids, I or II, can recede with the right diet modification, and with the right medical support.
The administration of flavonoids, supplementation of adequate fiber intake, and proper daily hydration can be a very effective therapy to regress hemorrhoids even without surgery, provided their prolapse is low grade.
Hemorrhoids grade II-III and up generally need a more assertive medical or surgical approach, including resorting to stabilized scleromousse.
Is it true that hemorrhoids cannot be cured?

No, it is totally wrong information, the result of old knowledge (and beliefs), which unfortunately still circulate among people.
It is true that hemorrhoidal prolapse, when initiated and never treated, tends to worsen over time (like any other prolapse, for that matter), but today's Medicine and Surgery always allow the problem of hemorrhoids to be resolved, albeit at different times.
The advent of scleromousse, for example, has radically changed the medical approach to hemorrhoids, making the use of Surgery limited to far fewer cases than in the past.
Careful diet and taking the right dietary supplements, then, can regress low stages of hemorrhoids without recourse to other treatments.
In short, modern Medicine and Surgery can always solve the problem of pathological hemorrhoids, but they need only one great support: the patient must decide to get treatment.
Often, out of foolish shame or fear of being in pain, the patient comes to the Proctologist only when the hemorrhoidal disease is already at its advanced stage, and this greatly complicates the treatment.
Treatment that, on the other hand, is much smoother, faster and even cheaper when the hemorrhoid problem is addressed immediately, in the early stage.
This is why hemorrhoids can always be cured, but it takes willpower to do so.
As well as, of course, the competent Physician.
Which physician specializes in pathological hemorrhoids?
The Proctologist is the medical professional of choice for the diagnosis and treatment of pathological hemorrhoids.
This is a Physician who is particularly specialized in the last part of the intestine, i.e., the rectum and anus, with the necessary experience to make diagnoses and, no less important, to proceed to the appropriate treatments, both medical and surgical.
Dr. Luisella Troyer is a Proctologic Vascular Surgeon who has specialized for years in the diagnosis and treatment, both medical and surgical, of pathological hemorrhoids.
In her Dubai clinic, Dr. Troyer can help you diagnose pathological hemorrhoids and their stage of severity with a quick and painless examination, Electronic Endoscopic Videoproctoscopy.
With this advanced, totally digital examination, Dr. Troyer can help you solve your hemorrhoid problem, without any kind of pain, with the best medical and surgical treatments available.
Treatments such as sterilized air-stabilized scleromousse, which can totally solve your hemorrhoid problem in a short time, without any pain and with an immediate return to sports and work activities.
For more than 30 years, Dr. Luisella Troyer has been the leading Proctology Surgeon for medical excellence against pathological hemorrhoids.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- HEMORRHOIDS ARE ARTERIOVENOUS PADS, LOCATED ANATOMICALLY WITHIN THE ANAL CANAL;
- IN NORMAL SITUATIONS, HEMORRHOIDS DO NOT GIVE ANY PROBLEMS, AND THEY ADEQUATELY VASCULARIZE THE ENTIRE ANUS;
- DUE TO MANY CAUSES AND TRIGGERS, HEMORRHOIDS CAN SWELL AND EXTRUDE FROM THE ANAL CANAL, GIVING RISE TO HEMORRHOIDAL PATHOLOGY;
- SWOLLEN AND PROLAPSED HEMORRHOIDS CAN EASILY BLEED AND TEAR, MAKING DEFECATION PAINFUL;
- ALONG WITH DENTAL CARIES, HEMORRHOIDAL PATHOLOGY IS THE NUMBER ONE ABSOLUTE DISEASE WORLDWIDE;
- THERE ARE DIFFERENT STAGES OF SEVERITY OF HEMORRHOIDS, DEPENDING ON THEIR SWELLING AND TOTAL PROLAPSE;
- MILD STAGE HEMORRHOIDS CAN BE EFFECTIVELY TREATED WITH DRUG TREATMENT AND THE RIGHT DIET MODIFICATION;
- HIGH-STAGE HEMORRHOIDS MUST BE TREATED SURGICALLY, OR WITH SPECIAL SCLEROSING TREATMENTS;
- IN RECENT TIMES, MILLIGAN-MORGAN HEMORRHOIDECTOMY MAY BE OFFERED AS AN ALTERNATIVE TO MILLIGAN-MORGAN HEMORRHOIDECTOMY WITH STERILIZED AIR SCLEROMOUSSE SCLEROTHERAPY;
- HEMORRHOIDS ARE A PROLAPSE THAT CAN BECOME CHRONIC AND, IF LEFT UNTREATED, CERTAINLY WORSEN OVER TIME;
- THE PROCTOLOGIST IS THE HEALTH CARE SPECIALIST INDICATED TO TREAT PATHOLOGICAL HEMORRHOIDS;
- IN THE EVENT OF A HEMORRHOID CRISIS, AVOID USING OVER-THE-COUNTER ANESTHETIC AND CORTISONE-BASED OINTMENTS, BUT BOOK A PROCTOLOGICAL EXAMINATION AS SOON AS POSSIBLE

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.

















