Have you been suffering from hemorrhoids for a long time?
Have you always been ashamed of the problem, and because of that, have you always put off a specialized proctological examination?
Hemorrhoidal prolapse, like any prolapse in the body, does not improve over time, but generally worsens.
And with it, the symptomatology of pathological hemorrhoids also becomes increasingly worse, including burning, bleeding with each evacuation, foreign body sensation in the anus, and, of course, the risk of painful hemorrhoid thrombus.
Many of these problems can be solved with modern Medicine and modern Surgery, but there is a need for a fundamental act on the part of the patient: he or she must make up his or her mind to seek treatment.
This page will tell you why you should never procrastinate on treating hemorrhoids, and why you should instead see a Proctologist Surgeon as soon as possible for their diagnosis and treatment.
Hematochezia is defined in Medicine as the loss of blood from theanal orifice.
Hematochezia can be due to a variety of pathological conditions, including hemorrhoids, but these can be either benign or malignant.
In addition to hemorrhoidal prolapse, bleeding from the anus may be due to anal fissure, intense proctitis, a violent episode of diarrhea that has irritated and lacerated the anal canal, diverticulitis, the presence of anorectal condylomata, and, although less frequent, carcinoma of the anus or rectum.
This last hypothesis scares the patient to death, but fortunately it is the least likely statistically.
Whatever condition has led to the bleeding must be properly diagnosed: sometimes a videoproctoscopy examination is sufficient, other times (if a lesion is suspected in the upper colon) a videocolonoscopy is required instead.
What are hemorrhoids?

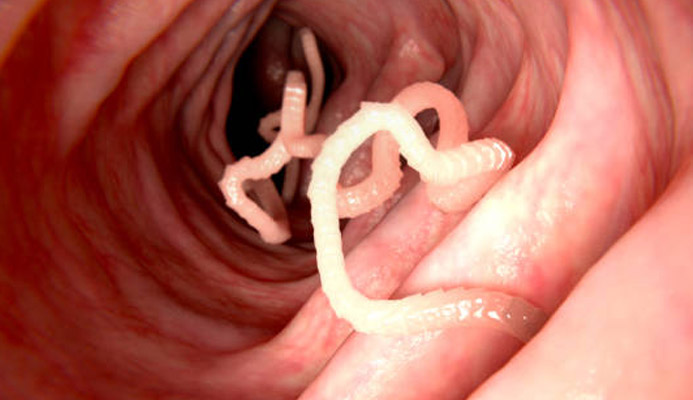
Hemorrhoids are vascular structures normally found in our anal canal, formed by an anastomosis, that is, an anatomical union, of veins and arteries.
There are three blood plexuses resembling soft pads, positioned radially around the anal canal: right anterior, right posterior and left lateral.
These three main hemorrhoids are joined by two other smaller ones, located roughly on either side of the left lateral hemorrhoid, called secondary hemorrhoids.
Hemorrhoids are formed by veins and arteries joined together, covered with a thick layer of connective tissue rich in collagen and elastic fibers, which make the plexuses soft but elastic and strong.
The primary functional task of hemorrhoids is to properly vascularize the entire anal canal and, secondarily, to aid the sphincter muscles in fecal continence.
Under normal conditions, hemorrhoids are not even perceived by the subject, and they remain to perform their silent task in the anal canal, without giving any problems.
Only when their clinical condition changes, and the plexuses begin to extrude from their original position, starting to give problems such as itching, soreness, burning, and bleeding during or shortly after defecation, we can speak of hemorrhoidal disease.
Pathological hemorrhoids and hemorrhoidal disease: why does it start?
In Medicine, hemorrhoids are defined as 'pathological' when, due to a long series of causes and triggers, the hemorrhoid plexuses begin to bulge and prolapse outward from the anal orifice, giving rise to a vast symptomatology that goes by the name of hemorrhoidal disease.
The initiating cause of this slow but steady prolapse of hemorrhoids has not yet been well framed by science, but two main theories are proposed:
- The mechanical theory, which perspectives a gradual and steady exhaustion of the fibro-muscle-elastic tissue that makes up the hemorrhoids and keeps them 'anchored' to the anal mucosal wall, which occurs through natural aging (and loss of collagen);
- The hemodynamic theory, which sees the onset of prolapse as a natural consequence of constant situations of elevated intra-abdominal pressure, such as in patients suffering from chronic constipation, obstructed defecation, or practicing certain sports or labors.
Pregnancy, childbirth and an inherited condition of venous endothelial fragility (typical of chronic venous insufficiency) are also included as triggers for this theory
These two theories are not necessarily in conflict with each other, and the occurrence of hemorrhoidal prolapse may be due to a combination, even partial, of the two causes.
Corroborating these two main theories, Medicine has long established a precise correlation of the onset of hemorrhoidal disease with a long series of so-called 'triggering' factors, which can be summarized as:
- Overweight and obesity;
- Poor diet, with nutrition too low in fiber and insufficient daily hydration;
- Sedentary lifestyle and little physical activity in general;
- Frequent episodes of diarrhea, often the result of irritable bowel syndrome or an autoimmune disease (such as Crohn's Disease and ulcerative rectocolitis);
- Laxative abuse caused by chronic constipation;
- Weightlifting, cycling, horseback riding, motorcycling;
- Fatigue work, particularly strenuous work, as well as work requiring long periods in an orthostatic position (standing and stationary)
The more hemorrhoids swell, the more they tend, by force of gravity, to prolapse outward from the anus.
Hemorrhoids now completely extruded from the anal orifice give daily problems of all kinds: from continuous irritationand inflammation to small or large lesions, which form from the hemorrhoids rubbing against undergarments.
This causes a series of continuous problems for the patient, such as anal itching, foreign body sensation in the anus, daily burning and bleeding, sometimes even without having gone to the toilet.
The formation of a painful hemorrhoidal thrombus is then much more likely in hemorrhoids that are now completely prolapsed thanin those that are more contained.
This is why one should never be reduced to the last moment to decide to treat hemorrhoids.
How common are hemorrhoids in the population?
Hemorrhoidal disease is the most common disease condition worldwide, along with dental caries.
Although the actual numbers of the phenomenon are difficult to gather, as hemorrhoids are often underestimated by patients, ignored for many years, or confused with other benign conditions, it is assumed that about half of the world's population at some point in their lives will manifest symptoms of hemorrhoidal prolapse.
Pathological hemorrhoids can appear at any age of life, even in very young patients but with low collagen production, and their incidence by gender sees a slight preference for women, almost certainly dictated by the natural condition of pregnancy and childbirth (factors often triggering prolapse).
What are the symptoms of pathological hemorrhoids?

The symptomatology of hemorrhoids is both well known to science and varied, with situations that are often confused by patients (but sometimes, even by some inexperienced Physicians) with other, often far more serious, pathological conditions (think, for example, of colon and rectal cancer).
That being said, among the main typical symptoms of hemorrhoidal disease, we can certainly include:
- Bleeding during or shortly after evacuation (hematochezia), the most typical symptom of pathological hemorrhoids, caused by the rubbing of feces on the plexuses swollen with blood.
This phenomenon often causes genuine terror in the patient, who thinks he or she is suffering from rectal or colon cancer;
- Burning during evacuation, caused by the passage of bacteria-laden feces over the injured and inflamed hemorrhoids;
- Anal itching, caused by the hyper-production of mucus in the anal canal that leads to maceration of the perianal skin.
Such hyper-production is a form of protection of the anal mucosa, which, not having a stratum corneum as the outer skin does, attempts to soothe the irritation of the hemorrhoidal plexuses by protecting them with a thick layer of mucus;
- Mechanical prolapse, which the patient notices by feeling it by touch during daily cleansing. Such prolapse may be more or less pronounced depending on the degree of staging of hemorrhoids;
- Anal tenesmus and a feeling of swelling and heaviness, with often continuous tension in the anus and a feeling of never having emptied completely after defecation;
- Anitis and proctitis, i.e., inflammation of the anorectal canal, anal orifice, and perianal skin, due to both the presence of prolapse (and its lesions) and overproduction of mucus;
- Intense and acute pain, sometimes so disabling that you cannot even walk properly, which in turn is a symptom of hemorrhoid thrombization (the famous and dreaded hemorrhoidal thrombus)
It is worth remembering that these symptoms are only a trace: the symptomatic condition of pathological hemorrhoids changes from patient to patient, and can often be confused with that of quite other conditions, such as anal fissures or anorectal carcinoma.
The intensity of these symptoms also changes according to the degree of the hemorrhoids, the patient's own sensitivity, and, not least, by the readiness to seek medical and surgical treatment.
Is there a severity scale for pathological hemorrhoids?

Yes, pathological hemorrhoids are classified according to their severity on a four-grade scale of progressive severity:
Grade I hemorrhoids
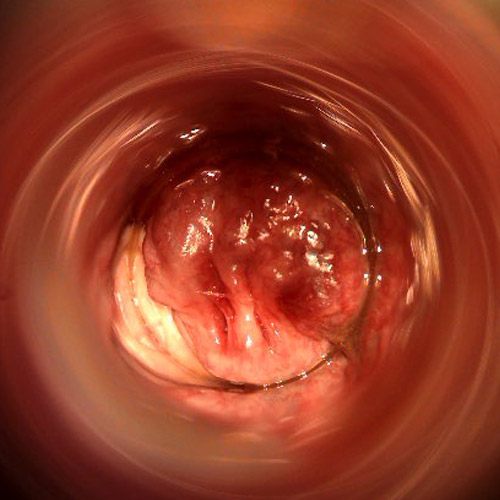
Hemorrhoid prolapse is minimal, and the hemorrhoids still remain completely inside the anal canal.
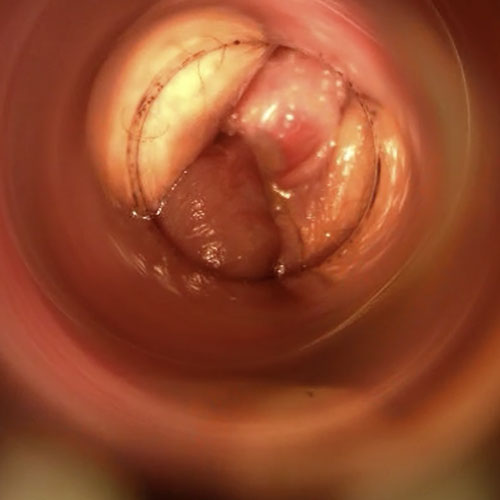
This is a condition that many patients do not even notice and is only detectable on examination by Electronic Endoscopic Videoproscopy.
Although the hemorrhoidal swelling is modest, this degree can still give rise to itching and inflammation and, although rarely, mild bleeding;
Grade II hemorrhoids
Hemorrhoid prolapse is more consistent, as is congestion of the plexuses, which leak from the anus during straining of evacuation or under conditions of particular exertion or sports.
Immediate re-entry occurs at the end of exertion, and episodes of inflammation, anal itching, bleeding, and sometimes tenesmus sensation may be present
Grade III hemorrhoids
Hemorrhoid prolapse is consistent, and hemorrhoids extrude out of the anal canal even without poncing or physical exertion.
Internal repositioning is still possible manually, and bleeding, burning, and hemorrhoid thrombus formation are common symptoms of this stage
Grade IV hemorrhoids
Hemorrhoid prolapse is permanent and irreversible, and the hemorrhoids result permanently prolapsed outside the anal canal, not being repositionable even with manual maneuvering.
It is a stage in which bleeding is almost daily, even during the day and not necessarily during defecation, because of the continuous rubbing of the hemorrhoids
Obviously, these stages are progressive, and prolapse occurs slowly (but steadily) over the years, especially if the patient does not decide to see the Proctology Physician and begin a course of treatment.
Why do hemorrhoids get worse over time?
Low-stage hemorrhoidal prolapse, indicatively up to stage II severity, especially in subjects who are still young and have good collagen and elastin production, can regress with the right conservative medical therapy.
This happens provided that the patient decides to be examined by a Proctology Physician, and therefore perform the necessary proctological medical examination.
If the early symptoms of hemorrhoidal prolapse are ignored, out of laxity or fear, generally the worsening of the condition is progressive, developing over a longer or shorter time.
The wearing away of the elastic structures you support the hemorrhoids is slow but steady, and the more the tissue wears away, the more it fills with blood, thus increasing the weight, which, under the force of gravity, tends to make the gavococci prolapse downward more and more.
This progressive worsening is accelerated by certain favoring conditions such as chronic constipation and any situation of abdominal hyper-pressure: pregnancy, childbirth, excessive abdominal strains at work or in the gym, even chronic diarrhea.
Frequent congestion and inflammation of the hemorrhoids, which easily tear as stool passes through, can also further worsen the clinical picture, increasingly increasing the severity of the condition.
Indicatively, stage III hemorrhoids are already almost impossible to get back just by diet and lifestyle modification, and recourse to medical or surgical treatment is almost always mandatory.
Why should one never procrastinate the use of proctological examination and medical treatment for hemorrhoids?

As explained just above, hemorrhoids are a chronic and degenerative condition.
The more the patient ignores the problem and delays treatment, the more the prolapse worsens, also worsening the symptoms.
The worse the prolapse gets, the more incisive and radical medical treatment must be, which sometimes is not enough and is replaced by surgery.
Often, either out of (unjustified) shame or simple fear, patients resort to medical examination only when the prolapse situation has become almost untenable, with episodes of stage III or IV hemorrhoids really severe.
This condition should be avoided, and the patient should be properly informed that treatment for hemorrhoids should be started as soon as possible.
By doing so, it is possible not only to avoid unpleasant complications and periods of pain and suffering, but the physician is also facilitated in treatment, which can therefore be much more bearable and serene for the patient as well.
How can pathological hemorrhoids be treated?

The treatment of hemorrhoids varies greatly according to their stage of severity.
Low-grade hemorrhoids require milder conservative therapies, while high-grade hemorrhoids require more vigorous, radical therapies.
Current Medicine can resolve almost any hemorrhoidal stage, but the therapy to be used varies greatly depending on the severity of the prolapse and also depending on the individual clinical case.
A first major distinction about specific treatments for hemorrhoids may be the type of approach: conservative or radical.
Conservative treatments are all those treatments or therapies that, as the name implies, do not remove the tissues of the hemorrhoid plexuses, but merely limit or reduce prolapse.
Conservative Medicine for hemorrhoids has many treatments, depending on the clinical case, which can be summarized as:
- Dietary control and decongestion of hemorrhoids, carried out by precise dietary advice, intake of the right amount of water daily, and prescription of phlebotonic drugs, as well as (if indicated) also by the application of local corticosteroids and flavonoids;
- HeLP technique, which is based on cauterizing the arterioles supplying the hemorrhoids;
- Elastic ligation of the hemorrhoidal gavage, an ancient, painful and now almost disused technique involving the application of a compressive elastic band at the base of the gavage and the subsequent necrosis and detachment of the gavage;
- Cryotherapy, which relies on freezing and subsequent necrosis of extruded gavocles (also a painful and disused therapy)
These treatments are usually indicated for mild stages of hemorrhoidal prolapse, indicatively up to stage II.
From the third stage onward, it is almost always necessary to intervene with more vigorous therapies, the goal of which is not simply the reduction of prolapse but the removal or complete destruction of the hemorrhoid plexuses themselves.
These therapies are called radical therapies, and they are almost always necessary for stages II and IV hemorrhoidal prolapse, so all other conservative therapies do not work or do not bring considerable results.
These radical therapies can be medical or surgical, and they are:
- Hemorrhoidectomy according to Milligan-Morgan, an ancient but still valid surgical therapy in which the hemorrhoidal plexuses are removed surgically, with excisions that do not involve final suturing.
The technique, if well performed, is resolving in about 95% of cases, but has the major disadvantage of being uncomfortable for the patient in the postoperative period;
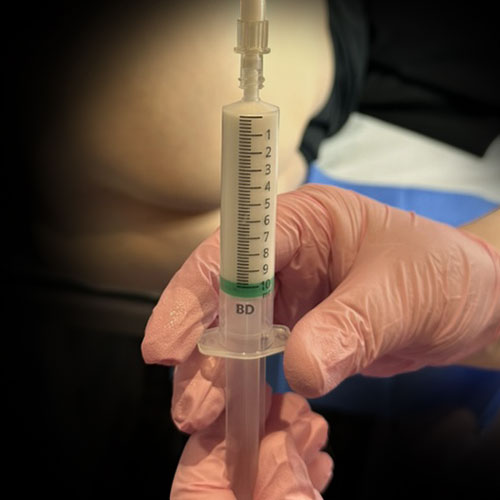
- Sclerotherapy with stabilized scleromousse, a modern and excellent therapy that involves the total closure of the gavococci by injection of polidocanol in mousse, which causes the internal walls of the hemorrhoids to sclerotize (close), thus causing their complete resolution.
Again, if successful, this therapy enables about 95% of patients to get rid of their hemorrhoids permanently
As always, it should be remembered that there is no one therapy better than the other for the resolution of pathological hemorrhoids: it is the Proctology Physician who, after the examination and after judging the patient's clinical condition to the best of his or her knowledge and belief, proposes the appropriate therapy.
What is scleromousse for hemorrhoids?

Sclerosing scleromousse therapy for the treatment of hemorrhoids is a modern medical therapy that, in recent years, is taking the place of Milligan-Morgan hemorrhoidectomy for a high number of clinical cases.
It is based on the inoculation of individual hemorrhoidal plexus using a special mousse consisting of sterile air and polidocanol (an alcohol drug), which is performed on an outpatient basis.
Polidocanol mousse clings tenaciously to the inner walls of hemorrhoids, causing controlled inflammation.
This inflammation destroys the inner tissue of the hemorrhoids and causes them to shrink, thus also closing the hemorrhoid plexuses, which permanently atrophy.
The result is a complete remission of the hemorrhoids, with permanent destruction of the prolapsed gavococci, which, as they recede, cause even partial receding of the anal mucosa, which is almost always prolapsed along with the hemorrhoids.
This leads to the patient's almost complete recovery, preventing him or her from resorting to the painful, even if effective, surgical solution.
Can scleromousse treatment for hemorrhoids be performed even on high-grade cases?

Yes, scleromousse treatment indeed was developed experimentally just for patients with a severe hemorrhoidal stage, awaiting surgery.
The therapy was developed in Italy during the COVID-19 pandemic, which essentially halted all non-emergency surgery, precisely to provide relief to patients awaiting surgery and suffering from major hemorrhoidal prolapse, beyond stage III.
Instead, the treatment, which started experimentally as a palliative, has yielded unhoped-for results: 95% of patients who underwent sclerosing treatment saw total prolapse reduction, without the need for surgical access.
That is why scleromousse for hemorrhoids can also be administered to patients with stage III or IV severity, who at one time would have been mandatorily referred for Surgery.
How are hemorrhoids diagnosed?

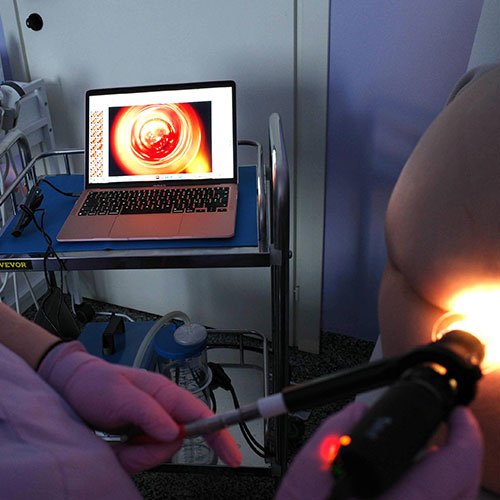
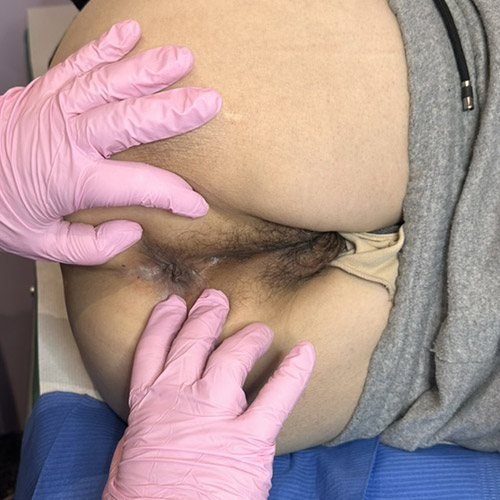
The diagnosis of hemorrhoids is clinical, and is made by a proctological examination, accompanied by a mandatory proctoscopy.
Top Proctology Physicians use for proctoscopy an examination of excellence called Electronic Endoscopic Videoproscopy: a totally digital, video-guided examination that allows analysis of the entire anorectal canal, giving the Physician high-definition, real-time, monitor-printed images.
This examination is essential for the evaluation of low-grade internal hemorrhoids, which are not visible externally and are difficult to see even with the optical anoscope.
Which doctor should be consulted to diagnose and treat pathological hemorrhoids?
Hemorrhoids and their prolapse are the expertise of Proctology, which is that part of Medicine that deals specifically with the study and treatment of diseases of the rectum and anus.
The Proctology Physician is almost always a Surgeon, who has perfected his or her training in Proctology directly in the field, with years and years of direct experience.
That is why, usually, Proctology Surgeons are all Doctors with decades of experience behind them, and only rarely turn out to be newly trained.
Therefore, the patient who wants to diagnose and start treating hemorrhoids should request a proctologic examination by a Proctologist Surgeon.
Do you suffer from hemorrhoids in Dubai? Don't wait any longer, rely on Dr. troyer

Dr. Luisella Troyer is a Proctologist Surgeon in Dubai, who has been perfecting both medical and surgical treatment of hemorrhoids for years.
At his office on , the doctor can help you diagnose exactly the degree of your hemorrhoids by means of advanced Electronic Endoscopic Videoproscopy: a modern, noninvasive exam that will allow you to discover the true state of your anal canal, as well as help the Doctor propose the most effective therapy to make you feel better.
Dr. Luisella Troyer is also an experienced Surgeon in sterilized air-stabilized sclerosant therapy: an excellent and innovative treatment that can in many cases replace surgery and lead to full resolution of hemorrhoids.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- HEMORRHOIDS ARE NORMAL ANATOMICAL PLEXUSES CONSISTING OF VEINS AND ARTERIESJOINED TOGETHER AND LOCATED IN THE ANAL CANAL;
- THERE ARE THREE MAIN HEMORRHOID PLEXUSES PLUS TWO SECONDARY ONES;
- UNDER NORMAL CONDITIONS , HEMORRHOIDS DO NOT CAUSE ANY DISCOMFORT, BUT RATHER CONTRIBUTE TO FECAL CONTINENCE;
- WHEN, FOR VARIOUS REASONS, THE HEMORRHOIDS SWELL AND EXTRUDE OUTSIDE THE ANAL CANAL, IT IS CALLED HEMORRHOIDAL DISEASE;
- OUT OF FEAR OR EMBARRASSMENT, PATIENTS OFTEN DELAY THE DIAGNOSIS AND TREATMENT OF HEMORRHOIDS, WORSENING THE CLINICAL SITUATION;
- THERE ARE FOUR STAGES OF SEVERITY OF HEMORRHOIDS, FROM FIRST TO FOURTH (THE MOST SEVERE);
- CHRONIC CONSTIPATION, CHRONIC DIARRHEA THAT HAS NEVER BEEN TREATED, CHILDBIRTH, PREGNANCY, AND CERTAIN SPORTS AND JOBS CAN BE THE TRIGGERS FOR HEMORRHOID PROLAPSE;
- MODERN MEDICINE AND SURGERY MAKE IT POSSIBLE TO SOLVE ALMOST ANY HEMORRHOID PROBLEM, AS LONG AS THE PATIENT IS DETERMINED TO GET TREATMENT;
- THERE ARE CONSERVATIVE TRATMENTS AND RADICAL TREATMENTS FOR THE TREATMENT OF HEMORRHOIDS, DEPENDING ON THE CLINICAL INDICATION;
- THE LONGER THE DIAGNOSIS AND TREATMENT OF HEMORRHOIDS IS DELAYED , THE MORE INVASIVE THE TREATMENTS NEEDED FOR CURE WILL BE

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.