Do you have difficulty with regular bowel movements?
Since you were young, have you always had problems with daily evacuation, and can never empty freely, no matter what diet you follow?
Have you gotten to the point where you can no longer evacuate always the use of enemas, purgatives or laxatives?
Is your mood and quality of life now hopelessly compromised by your bowel activity, which is coming to severely affect your activity even at work?
Chronic constipation is a serious problem and a disabling condition that is often totally ignored, prompting patients to seek 'do-it-yourself' methods that, in most cases, always prove ineffective or even deleterious.
Read this page to find out what chronic constipation is, and what can be done to counter it, with the help of modern bowel rehabilitation.
Single, sporadic episodes of constipation are common to everyone, and should not alarm.
Often, the bowels slow down for small reasons that usually resolve within a short time, and are therefore not dangerous.
Sometimes these reasons are not physiological in origin, but psychological.
For example, it is quite normal to have small episodes of constipation when traveling, or when attending an unfamiliar place for the first time.
The reasons for this are changes in diet (on vacation or travel, one usually eats different food than usual),long periods of immobility while traveling, even the psychological perception of 'not being' in one's comfort zone.
What is constipation?

Constipation is the inability to provide for regular, daily evacuations of soft, well-formed stools that are of the right consistency and give the feeling of complete bowel emptying and well-being.
In adult humans, the daily defecatory act is considered physiological and normal, with the emission of about 150 g of stool (European and North American average), which is soft and cylindrical, not excessively malodorous and well compacted.
It should be noted, however, that variations to this average are very frequent, and are often physiological for the subject, without necessarily bordering on actual constipation.
So, any evaluation and eventual diagnosis of constipation must have rather elastic parameters, and should always be hypothesized, however, taking into account the patient's strictly personal habits.
What is clinically meant by constipation?

Still considering the necessary elasticity of judgment when defining the concept of constipation, at the clinical level we tend to diagnose a state of true constipation when at least two of these symptomatic manifestations occur within 12 month:
- Less than two evacuations every seven days;
- At least one in four evacuations is difficult, painful, and requires a great deal of effort on the part of the patient to get the stool out;
- At least one in four evacuations sees hard, volute-increased and so-called 'goat' shaped stools that are extremely difficult to evacuate;
- At least one out of four times there is a feeling of incomplete or unsatisfactory emptying
What are the actual causes of constipation?

Constipation is an enormously complex alteration of alvus that varies greatly, in intensity and symptom relevance, from patient to patient.
Because of this, the causes of pathology can also vary greatly, and are often not well defined, even in the face of impeccable medical histories.
A first distinction of constipation can be made on its origin: primary (idiopathic) or secondary.
Primitive constipation is constipation that is in many cases congenital, occurring even in childhood (about 3% of all primitive constipation is pediatric in nature).
It is in turn divided into simple constipation (the most common), from colon inertia, obstructed defecation (rectal constipation), colic constipation, from irritable bowel syndrome, from coli inertia, and pregnancy constipation.
Simple constipation is closely linked to a low-fiber diet, a congenital predisposition that worsens over time (the patient becomes accustomed to holding stool), and, often, a sedentary lifestyle.
It can also occur in patients who are not originally predisposed, but who as a result of particular behaviors or diseases (excessive weight loss diets or anorexia, for example) change their bowel habits, becoming constipated.
Irritable bowel constipation, another congenital manifestation, is associated with abdominal pain, meteorism, anxiety, depression, and periods of relative quiet interspersed with recrudescence of the condition.
Constipation called inertia coli exclusively afflicts women, is among the most severe forms (less than two evacuations every 7-8 days), and has a hormonal disruption as its supposed origin.
This form is also suspected to occur as pregnancy constipation, and after the delivery is over, it usually resolves spontaneously.
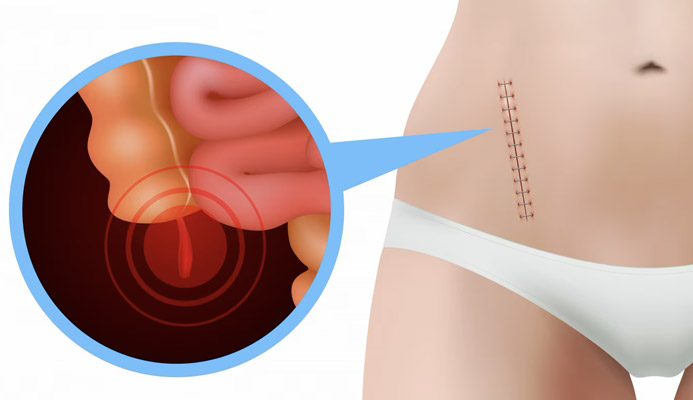
Rectal constipation, or obstructed defecation, on the other hand, is the inability to provide for the proper explosion of stool due to purely mechanical problems, such as a congenital deviation of the rectum, its obstruction, or a malfunction of the sphincter and pubic muscles.
In women, this issue often coincides with rectocele and pelvic floor release.
Colic constipation is caused by impaired and sluggish mobility of the colon, with slow peristalsis and, as a result, longer transit of stool in the intestine, which causes hyper-absorption of fluids and, consequently, excessive hardening of stool.
What are the symptoms of constipation?

Regardless of its origin, all constipation, of whatever kind, shares the same underlying problem (as well as symptom): the inability to evacuate satisfactorily and regularly, without fatigue or pain.
Fatigue and pain are two key related symptoms, to identify constipation and get a good understanding of patients' suffering.
In fact, the constipated patient often has to resort to excessive straining (the pushing of the pelvic floor muscles) during evacuation, and this often causes pain, fatigue, and a number of related conditions that, in the long run, almost all constipated patients experience (e.g., rectal prolapse and pathological hemorrhoids).
Then add to this the whole psychophysical outfit that chronic constipation brings with it, which is well known to sufferers: depression, irritability, insomnia, headache, halitosis, flatulence.
How is constipation diagnosed?
Diagnosis of constipation is never easy, because the condition tends to be reported by the patient as a cause for embarrassment and ridicule, and is therefore often self-diagnosed and self-cured, almost always with unnecessary or indeed harmful treatments (such as laxative abuse).
This worsens the pathology because it prevents its proper framing, resulting in a delay in treatment.
Not surprisingly, almost all constipated patients who present to the Doctor do so after many years of suffering, often telling stories of great prostration and difficulty.
Diagnosis of constipation involves a complete colonproctological examination, with a precise and careful medical history and, if necessary, specific instrumental tests.
Such supportive examinations may be a defecography, colonoscopy, abdominopelvic CT scan, anorectal manometry, endoanal ultrasound, pelvic floor MRI, or perineal EMG.
The complexity of the pathology requires a highly personalized approach, even at the investigation stage.
Constipation should not be an object of ridicule or irony: it is a real intestinal pathology, which makes the quality of life, for patients suffering from it, very complicated.
Unfortunately, being a non-life-threatening condition, it is often underestimated or ignored, even by Doctors themselves, who do not know (and do not want to learn how to) treat it, solving it by prescribing purges and laxatives.
This not only worsens the patient's bowel condition, but further lowers his or her perceptual level at the urge to defecate, in fact further complicating constipation.
Which chronicizes, and becomes increasingly disabling.
What is the treatment for constipation?
Treatment of constipation is directly related to the type of constipation, and it should therefore be clarified as a starting point whether the patient has primary or secondary constipation.
Many cases of constipation have depended on an unsuitable diet low in fiber and necessary and sufficient hydration: in these cases, modification of diet and eating habits in general should always be prescribed.
Whatever the cause of the constipation and whatever therapeutic approach the physician decides, however, laxatives and purgatives should be avoided at all costs.
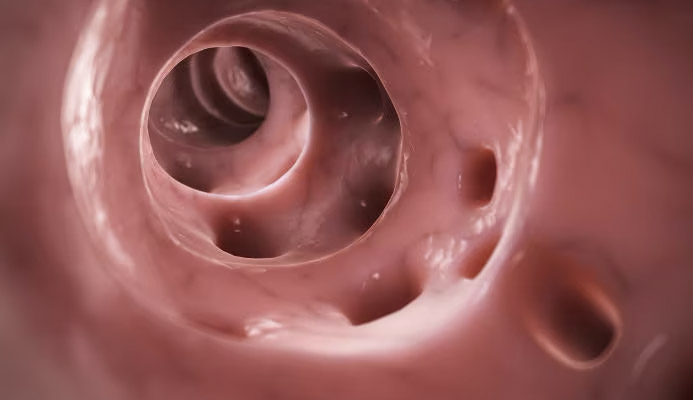
Enemas and laxatives are never a solution: they worsen bowel mobility, irritate the mucosa, and cause, over time, addiction and dependence.
Any other pharmacological aid, not necessarily laxative, must also be well thought out, and prescribed for time-limited use in any case.
In general, modern colonproctology protocols for constipation aim to rehabilitate the bowel, resolving the problem at its source.
This bowel rehabilitation is achieved using different physiotherapeutic methodologies:
- Physiokinesiotherapy;
- Electrostimulation;
- Biofeedback
Physiokinesiotherapy refers to all those physiotherapeutic practices of strengthening and re-elasticizing the pelvic floor, with free or counter-resistance exercises.
Associated with this gymnastics is muscular electrostimulation, performed by means of special electromedical devices, which na aim to improve muscle contraction.
This therapy is judged to be the Gold Standard for flaccid constipation.
Biofeedback, on the other hand, is a true bowel re-education, performed by means of special computerized equipment that generates outputs (visual, auditory or sensory) that can help the patient understand and regain bowel sensitivity, especially by means of learning sphincter capacity.
Biofeedback, when well executed, is capable of yielding excellent results: at the end of therapy, about 92% of patients returned to regular bowel activity, with no further use of laxatives or purgatives.
It should necessarily be emphasized that, in order to achieve appreciable results, the patient must perform all therapy (physiokinesitherapy, electrostimulation and biofeedback), in the sessions scheduled and prescribed by the Physician, with perseverance and commitment.
Bowel rehabilitation is a long journey that requires self-denial and painstaking follow-up, with impeccable patient compliance.
Do you suffer from chronic constipation and are you from Dubai? You can stop suffering, with the help of Dr. Luisella Troyer
If you have been experiencing evacuation problems for years and suffer from chronic constipation, with now a necessary and irreplaceable overuse of purgatives and laxatives, know that, your intestines do not like this.
Continued use of enemas, purgatives, and laxatives irritates the intestinal mucosa, worsens peristalsis, and acidifies stools, thus worsening the clinical picture.
Dr. Luisella Troyer's practice specializes in gut rehabilitation with innovative protocols based on physiokinesitherapy, electrostimulation and biofeedback.
You will then be able to return to regular bowel activity, even with restful diet control followed by the Doctor, freeing you forever from the use of laxatives and purgatives.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- CONSTIPATION IS THE MOST COMMON BOWEL DYSFUNCTION, AFFLICTING A LARGE PERCENTAGE OF PEOPLE WORLDWIDE;
- CONSTIPATION MANIFESTS AS THE INABILITY TO PROVIDE ALLEREGULARDAILY EVACUATIONS;
- A HEALTHY ADULT HUMAN BEING PRODUCES ABOUT 150 G OF WELL-FORMED, SOLID, SOFT STOOL EACH DAY;
- VARIATIONS TO THIS AVERAGE ARE COMMON, HOWEVER, AND NEED NOT BE PATHOLOGICAL AND BE CONSIDERED CONSTIPATION;
- THERE ARE A WIDE VARIETY OF TYPES OF CONSTIPATION, WHICH CAN, HOWEVER, BE DISTINGUISHED INTO IDIOPATHIC CONSTIPATION AND SECONDARY CONSTIPATION;
- USUALLY, CONSTIPATION IS A PATHOLOGICAL CONDITION NEGLECTED BY MEDICINE, AND THE MEDICAL SUPPORT THE PATIENT OFTEN RECEIVES IS INSUFFICIENT OR POOR, RELEGATED ALMOST ALWAYS TO THE USE OF PURGATIVES AND LAXATIVES;
- SUMMARIZING, THERE ARE CONSTIPATION FROM POOR COLONIC MOBILITY AND CONSTIPATION FROM OBSTRUCTED DEFECATION;
- THE ROLE OF DIET IN SIMPLE CONSTIPATION IS CRUCIAL, AND IS OFTEN THE UPSTREAM CAUSE OF CONSTIPATION;
- THE PATIENT WITH CONSTIPATION NOT ONLY EVACUATES LATE, BUT ALSO LABORIOUSLY;
- CONTINUOUS USE OF PURGATIVES AND LAXATIVES IS HARMFUL TO THE INTESTINES, AS IT IRRITATES THE COLON WALLS AND ACIDIFIES THE STOOL;
- IN THE LONG RUN, CONSTIPATION CAUSES A NUMBER OF PROCTOLOGICAL CONDITIONS RELATED TO INCREASED INTRA-ABDOMINAL PRESSURE, SUCH AS PATHOLOGICAL HEMORRHOIDS AND PROLAPSE OF THE RECTUM;
- MODERN BOWEL REHABILITATION PROTOCOLS, UNFORTUNATELY LITTLE PRACTICED IN ITALY, AIM TO REHABILITATE THE COLON, AND RE-EDUCATE THE PATIENT TO THE STIMULUS TO DEFECATION;
- THE APPROPRIATE THERAPY TO RESOLVE CONSTIPATION IS REHABILITATION, AVOIDING THE USE OF PURGATIVES AND LAXATIVES

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.