
Do you bleed from the anus when you have a bowel movement?
Do red streaks of live blood remain on the toilet paper, or does blood drip profusely immediately after defecation?
Do you notice reddish streaks on your stool that make you worry and for which you cannot give an explanation?
Hematochezia, or blood loss from the anus, is a clear symptom, indicating a lesion in the anorectal canal or colon.
Read this page written by Dr. Luisella Troyer to find out what the main causes of anal bleeding are, and what you should do to begin to remedy it.
Finding traces of blood on feces or toilet paper is an experience that many patients find terrible and distressing.
Sometimes, one immediately thinks of very serious conditions, such as ano-rectal carcionoma, but in reality, statistics fortunately say thathematochezia, or anal bleeding, is more attributable to benign conditions such as hemorrhoidal prolapse and anal fissure.
That is why it is extremely important to remain calm in case of anal bleeding, not to panic but to book a specialized proctological examination as soon as possible.
What is anal bleeding?

In Medicine, anal bleeding refers to a condition of hematochezia, a loss of blood from the anus, usually (but not exclusively) referable during or shortly after defecation.
This condition is pathological, as in normal human physiology defecation is not an act that involves bleeding, just as it does not involve pain or discomfort but rather is an act considered liberating and fulfilling.
Hematochezia refers to small bleeding, which can stain toilet paper or streak stools, but can also lead to direct dripping from the anus.
When this dripping becomes actual bleeding, with copious loss of blood, hematochezia takes the more appropriate name of rectorrhagia.
What are the causes of anal bleeding?

Anal bleeding is always a symptom of an injury to the anorectal or intestinal mucosa, the origins of which can vary widely, and are included in a long list of pathologies.
Among the many pathological conditions that can cause bleeding from the anus we can mention:
- Pathological hemorrhoids and hemorrhoidal prolapse;
- Anal fissure;
- Proctitis and anitis;
- Anal warts;
- Carcinoma of the rectum and colon;
- Intestinal abscess;
- Diverticulitis;
- Ulcerative rectocolitis;
- Crohn's disease;
- Rectal or intestinal polyps
The list of all conditions that can injure the mucosa of the colon, rectum, and anus is extensive, and this list represents only those conditions that, statistically, are present in the largest percentage among all cases of anal bleeding.
What does anal bleeding look like?
Anal bleeding can be different depending on the pathology that generates it, or rather depending on the pathology that generates the lesion that bleeds.
Broadly speaking, we can divide the symptomatology of anal bleeding into:
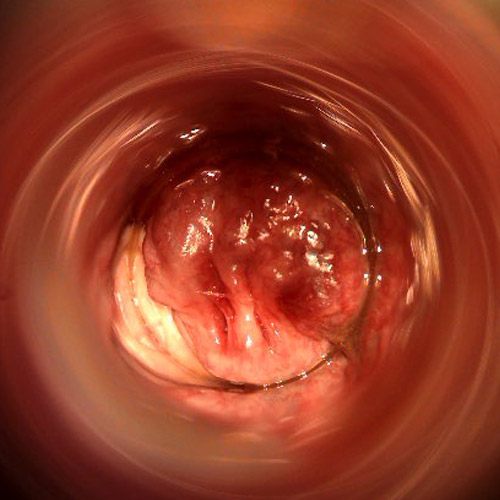
Bright red blood, dripping
This type of bleeding occurs at the end of defecation, and is bright red in color.
This bleeding indicates a fresh lesion, usually located in the lower part of the rectum or in the rectal canal.
This is a typical condition of the laceration of hemorrhoidal prolapses.
This bleeding may be accompanied by a strong burning sensation, which may disappear after a few minutes or continue for several hours.
In this case, suspicion of anal fissure should always be considered;
Streaked blood on toilet paper
This type of bleeding is almost intangible, there is no dripping, and there are no traces on the stool.
One notices the blood only because it remains, in the form of streaks, on the toilet paper after defecation cleaning.
This type of bleeding is typical of inflamed and slightly injured hemorrhoids;
Streaked blood on stool
The blood does not drip from the anus and remain on the toilet paper, but remains evident as streaks on the stool, bright red in color.
It may signify a lesion of the anorectal canal, perhaps due to particularly hard and constipated bowel, inflammation (proctitis), or tumor-like neoformations of the last part of the intestine;
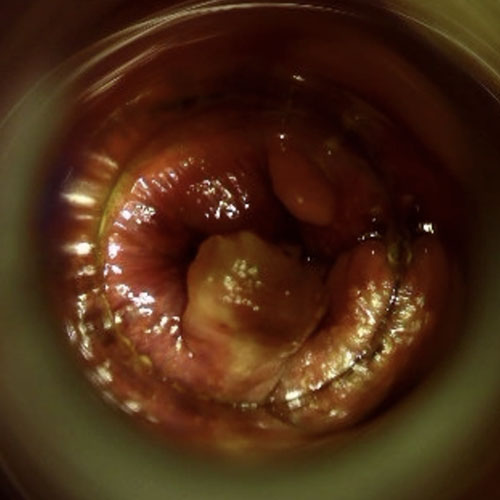
Dark red blood on stool
Traces of blood are present in the form of streaks on the stool, but these appear particularly dark in color.
It is a typical symptom of an alteration of the upper colon such as a small hemorrhage, diverticulitis, large intestinal polyps, tumor formation, or congenital autoimmune diseases such as ulcerative rectocolitis and Crohn's disease.
Small vascular lesions, afferent to the inner wall of the intestinal mucosa, also can be the origin of this type of bleeding;
Black blood (clotted)
Traces of black, clotted, practically solid blood should always raise suspicion of serious gastrointestinal pathology, such as diverticulitis, carcinoma of the intestine, severe intestinal injury, etc.
These conditions generally require immediate hospitalization of the patient;
Blood with diarrhea and mucus
Traces of blood in the presence of heavy diarrheal discharges are considered physiological, as acidified feces often and willingly damage the delicate intestinal mucosa and anorectal canal, tearing it and thus giving rise to proctitis and bleeding.
This happens as a result of infection by intestinal bacteria or viruses or, in noninfectious diseases, in the presence of irritable bowel syndrome, celiac disease, ulcerative rectocolitis, and Crohn's disease;
Bright red and copious blood in the absence of defecation
The loss of bright red blood from the anus even if defecation has not taken place, especially if in copious amounts, is a symptom that goes beyond hematochezia, and is called rectorrhagia.
This is a serious condition, requiring immediate hospital access, as it is a symptom of vascular bleeding in the intestines, sometimes caused by poorly treated diverticulitis.
However, this list of different bleeding-related symptoms should be taken as a general outline, and not as a strict classification.
The symptomatology of anal bleeding is truly vast to categorize, and many conditions have features that overlap with other conditions, making diagnosis as to the real causes of bleeding difficult unless done by an experienced Proctologist Physician.
Some pathologies are totally benign, such as hemorrhoidal prolapse and anal fissure, while others are tumor-like neoformations (such as carcinoma of the rectum) or the result of autoimmune diseases (e.g., ulcerative rectocholitis-AS).
In all cases, they may have the same bleeding symptoms, which may be confusing to the patient.
That is why in any situation where anal bleeding is experienced, it is imperative not to prevaricate or proceed with 'do-it-yourself' treatments, but to perform a specialized proctological examination as soon as possible.
Why can hemorrhoids bleed when going to the bathroom?
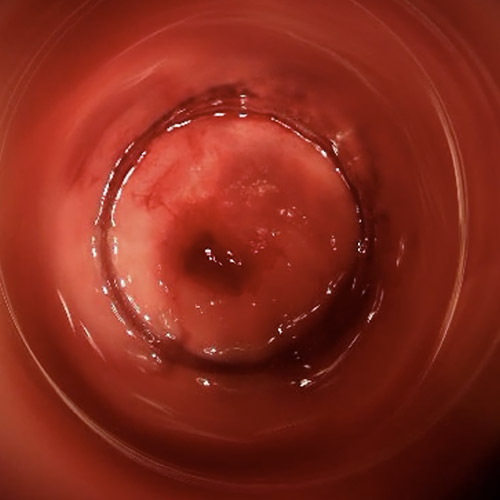
Hemorrhoids are pads formed by veins and arteries, richly vascularized, normally present in our anal canal.
There are three main ones (right front, right rear and left side), to which two more secondary ones are added.
Under normal conditions, hemorrhoids are not even perceived and dissolve their function of vascularizing the anal canal and, secondarily, helping the sphincters to maintain fecal continence.
It happens, however, that due to genetic predisposition and triggering factors (such as chronic constipation, a woman's labor and delivery, or natural aging) the hemorrhoidal plexuses try out of their original anatomical location, swelling and giving rise to hemorrhoidal pathology.
Sometimes, even in the absence of true prolapse, hemorrhoids may still extrude slightly and become inflamed: this is common, for example, during violent diarrheal discharges in cases of gastrointestinal infection.
Extruded or inflamed hemorrhoids are easily injured, and this happens as stools pass through, especially if they are particularly hard (such as those of patients with chronic constipation) or acidified, such as precisely those with diarrhea.
Thus, most cases of anal bleeding due to benign causes are attributable precisely to hemorrhoids, and their prolapse or inflammation.
The anorectal mucosa is extremely delicate, since (like every other mucosa in the body) it is not protected by thestratum corneum epithelium.
This is why it takes very little to tear it, such as a particularly hard discharge of stool.
The resulting bleeding, which is totally benign, is therefore an obvious result of an injury to the walls of the anorectal canal.
What is anal fissure, and why does it bleed?
An anal fissure is essentially an ulcer of the anorectal canal that, like any sore, demonstrates a very slow or, in some cases, completely absent ability to heal.
It manifests as a vertical wound, roughly following the pleats of the anal orifice, and its major (and most feared) symptom is very high pain, both during defecation and during particular movements (even of common daily life).
Conventionally, an anal wound that shows no signs of healing in about six weeks after its symptomatic onset is considered a 'fissure'.
Fortunately, only a small proportion of anal canal injuries turn into fissures, and an even smaller proportion require medical or surgical treatment.
A fissure, being for all intents and purposes an open sore, bleeds (even profusely) when it comes in contact with stool, and in addition to bleeding there is often burning and sharp pain, which in many cases lingers even after defecation.
But can anal bleeding be a symptom of rectal, anus, or colon cancer?
Yes, anal bleeding can be a symptom of a neoplasm to any part of the intestine, but unfortunately almost all cases of rectal or colon cancer are, at least in the early stages, asymptomatic.
This means that the tumor, which always originates from the intestinal mucosa, can grow and develop without any particular symptoms, thus even without the bleeding that is the prerogative of advanced stages of the disease.
That is why, while anal bleeding may still be part of the symptomatology of colon and rectal cancer, in the differential diagnosis the Proctologist should also take into account the age of the patient and the possible presence of concurrent diseases that, statistically, are often the main cause of hematochezia, such as pathological hemorrhoids and anal fissure.
Contrary to what is still (mistakenly) thought, the proctological examination is not painful, is not embarrassing, and is carried out without the slightest discomfort for the patient.
Therefore, one should not tergiversate and, in case of anal bleeding, book a specialized proctological examination as soon as possible, which is the only one that can clearly shed light on the problem.
Can anal fistula give rise to anal bleeding?
An anal fistula is the evolution of a neglected or complicated anal abscess, and manifests as an artificial 'tunnel' that, from the original site of infection (a mucus gland in the perianal area) carves an alternative route through the sphincters to the anorectal canal.
Usually, purulent, foul-smelling material, and not blood, instead present in the lesions of pathological hemorrhoids and fissures, exits from the fistula.
What is occult blood in stool?
Occult blood in stool, as the name implies, is the presence in feces of blood traces invisible to the naked eye.
This is a situation that may raise suspicion of a lesion in the upper digestive tract, an intestinal polyp or the onset of colon cancer.
This occult blood is detected by stool examination and microscopic observation, and is a diagnostic that is usually prescribed in patients over 50 in whom the physician suspects an unobservable lesion of the high bowel or colon.
Often, such an examination, if positive, is accompanied by a colonoscopy and gastroscopy to thoroughly and completely investigate the entire gastrodigestive tract.
Is it normal to bleed from the anus after having violent bouts of diarrhea?
Yes, tearing of the anorectal canal following consecutive episodes of acute diarrhea is considered physiological.
This is because diarrheal stools are acidified, and they injure and irritate the anorectal wall, including the hemorrhoids, which become inflamed and, torn, bleed.
These are often isolated episodes, occurring in violent diarrheal attacks following food poisoning (e.g., salmonella poisoning) or intestinal viruses.
Sometimes, however, in individuals with chronic autoimmune pathologies, such as celiac patients and those with ulcerative rectocolitis, such conditions come to be recurrent, dependent on the course of their triggering pathology.
What should you do if you experience an episode of anal bleeding?
A single episode of anal bleeding generally should not alarm or frighten.
Most often, it depended on a small tear in the anorectal mucosa, given by a particularly major constipation episode or multiple bouts of diarrhea, the result of food poisoning.
Or, it depended on a small hemorrhoidal inflammation, which is transient in nature and resolves spontaneously.
That said, considering that even these small episodes often trigger patients' terror, it is always a good thing to remain calm and rational, and to book a specialized proctological examination.
Only the specialized proctological examination, correlated by the Electronic Endoscopic Videoproscopy examination, can give a clear answer to the diagnostic questions and reassure the patient, or direct him or her to the appropriate therapy that can cure the origin of the lesion that led to the anal bleeding.
Which Physician should be referred to for a proctological examination after an episode of anal bleeding?

The health professional who specializes in the study and treatment of all disorders of the anorectal canal is the Proctologist Physician.
It is therefore to him that one must turn when one is the victim of one or more episodes of anal bleeding: the Proctologist is the Doctor who has great experience in all the pathologies of the last part of the intestine, as well as using the appropriate diagnostic tools to perfectly frame the origin of the problem.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- HEMATOCHEZIA IS ANAL BLEEDING AFTER OR DURING EVACUATION;
- WHEN THE BLEEDING IS COPIOUS, SIMILAR TO AHEMORRHAGE, IT IS INSTEAD NAMED RECTORRHAGIA;
- ANAL BLEEDING IS ALWAYS A SYMPTOM OF A LESION IN THE BOWEL, EITHER AT A HIGH LEVEL OR TOWARD THE END, THAT IS, IN THE RECTAL OR ANAL CANAL;
- SOME PROCTOLOGIC DISEASES HAVE ANAL BLEEDING AS A SYMPTOM SPECIFICALLY;
- PROLAPSED HEMORRHOIDS CAN TEAR EASILY, GIVING RISE TO ANAL BLEEDING;
- ANAL FISSURE, BEING FOR ALL INTENTS AND PURPOSES A WOUND, ALSO USUALLY BLEEDS WHEN STOOL PASSES;
- ANAL BLEEDING COULD ALSO INDICATE THE PRESENCE OFNON-BENIGN PATHOLOGIES, SUCH AS CARCINOMA OF THE RECTUM;
- IN CASE YOU EXPERIENCE ANAL BLEEDING AFTER EVACUATION, THERE IS NO NEED TO PANIC, BUT YOU SHOULD BOOK A PROCTOLOGICAL EXAMINATION AS SOON AS POSSIBLE

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.

















