Do you notice traces of blood on stool after you finish defecating, which remain imprinted on the toilet paper?
Have you noticed blood streaks on the stool, bright red in color?
Anal bleeding is always a symptom of an internal injury to the delicate anorectal canal, but it often has benign origins, such as pathological hemorrhoids.
Read this page to find out what anal bleeding after evacuation may be due to, and which Doctor can help you diagnose the cause.
A single sporadic episode of anal bleeding, although often causing terror in the patient, usually has a benign origin, and is often coincident with a small mucosal tear.
Perhaps, caused by particularly harsh bowel movements (common in constipated patients).
What should be done, in the case, is not to become frightened or agitated, but to book a specialist proctological examination.
What is anal bleeding?

In Medicine, anal bleeding (hematochezia) is defined as the condition of anal bleeding after or during evacuation, which goes so far as to soil both the toilet paper and the stool itself, leaving reddish streaks on them.
On the other hand, when the blood loss is copious, and occurs not necessarily during defecation, it is more properly referred to as rectorrhagia.
Statistically, most cases of hematochezia are due to benign diseases of the anorectal canal, such as pathological hemorrhoids and anal fissures.
Major cases of rectoragia, on the other hand, should always suggest a serious rectal or bowel injury, and are usually a typical proctological urgency.
Bleeding caused by hemorrhoidal prolapse

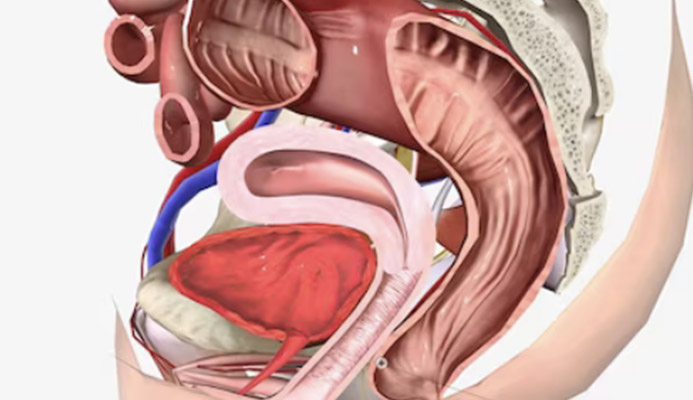
Hemorrhoids are athero-venous plexuses, resembling swollen pads of blood, located internally in the anal canal.
There are three main ones: right front, right rear and left side.
Their function is to properly vascularize the entire anal canal and, secondarily, to assist the sphincters in fecal continence.
In normal situations, hemorrhoids do not give any kind of problem, and their presence is therefore not even felt by our body.
Problems begin when, due to a variety of causes and triggers, these pads become pathologically swollen, extrude from their original anatomical location, and protrude from the anal canal, giving rise to what is called hemorrhoidal pathology.
Extruding out of their seat, the hemorrhoids, which are swollen with blood, then become liable to chafing and tearing due to the passage of stool, which worsens under special conditions, such as in the case of particularly harsh stool, as in that of constipated patients.
Chronic diarrhea conditions, with particularly acidified stool production, is also a trigger for hematochezia and tearing of the hemorrhoidal wall.
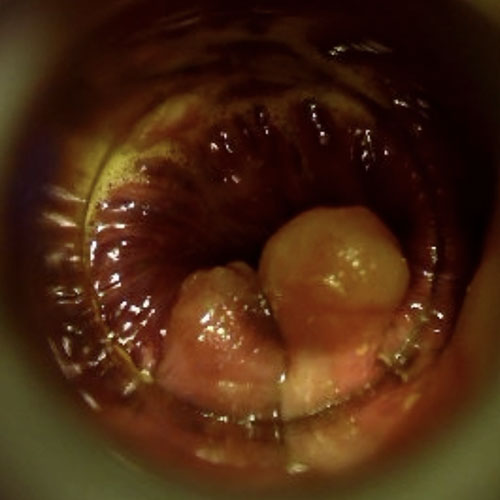
What does blood due to tearing of hemorrhoidal plexuses look like?

Hemorrhoids torn by feces may also bleed profusely, with recurrent hematochezia occurring with each evacuation.
The blood appears as bright red, and may remain on the toilet paper during cleaning or even streak the stool.
In cases of major hemorrhoidal prolapse, true copious dripping is not uncommon, which often frightens and terrifies the patient.
Anal bleeding is often associated with burning, even intense burning, a symptom of the irritation that bacteria in the stool cause on the injured mucosa of the hemorrhoids.
In contrast to hematochezia, i.e., minor bleeding during or after evacuation, rectorrhagia is extremely copious bleeding, a true hemorrhage.
This can occur even without evacuation, and is usually a symptom of a serious bowel situation, requiring immediate medical or surgical treatment.
Bleeding due to anal fissure
An anal fissure is an injury (wound) of the anus or anal canal that heals very slowly, and sometimes healing is even totally absent.
It is always a vertical wound parallel to the sagittal plane, following the typical pleats of the perianal mucosa.
It can be outside the anal orifice or inside the anal canal, and has as symptoms pain and burning at the passage of stool, bleeding, and, in severe cases, pain even during normal daily activities.
The reason an anal wound ulcerates and becomes a fissure are always related to poor vascularization of the area, which does not allow platelets, oxygen, and blood in general to send all the necessary elements for healing.
This vascular deficit is often related to a hypertonus of the internal sphincter muscle, which, stimulated by the pain of the fissure, contracts too vigorously and frequently, resulting in spasms that do not allow regular arterial blood flow.
As the stool passes, the fissure burns and bleeds, as it is in effect an ulcer that is unable to heal.
Bleeding is similar to that of pathological hemorrhoids, and is usually bright red, either on the toilet paper or, in the form of streaks, on the stool.
Anal warts and their bleeding
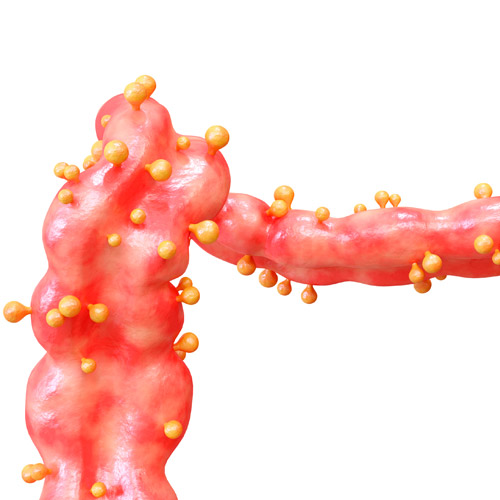
Anal warts, also known as anal condylomata, are fleshy, often sharp-shaped lesions (but flat ones also exist) that can invade the anus and anal canal, triggering what is called anal condylomatosis.
They are an extreme response of the immune system to an out-of-control viral infection, specifically that due to Human Papilloma Virus (HPV), from the same viral family that causes common warts.
Warts are an extreme and desperate response of the immune system, which, overwhelmed by the virus due to a variety of causes and predisposing factors, attempts to stem the infection by confining the virus outward, thus giving rise to condylomatous lesions.
Florid, acuminate anal warts have the characteristic of locating 'in clusters' over a given area of the anal mucosa and perianal skin, and like all protruding lesions they can be lacerated by the passage of feces, thus beginning to bleed.
Again, the bleeding is bright red, more or less copious depending on how many condylomata have been lacerated at the passage of stool.
In contrast to benign conditions, warts are a form considered pre-cancerous, highly infectious.
This means that the blood coming out of their lesions can, potentially, infect other areas of the body, essentially allowing the virus to expand.
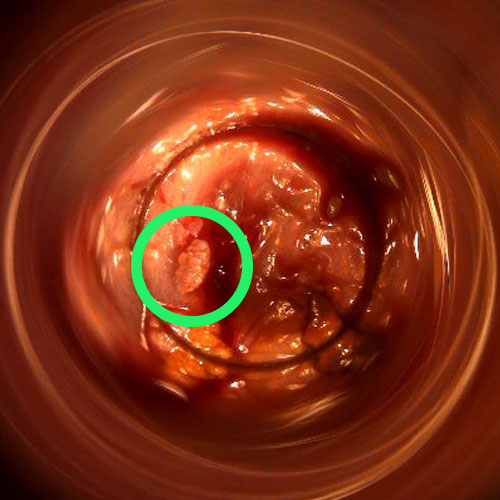
Bleeding from rectal polyposis
In medicine, a polyp is a lesion of the mucosa, in this case the intestinal mucosa, considering a pre-cancerous lesion.
It can develop anywhere along the gastrodigestive tract, and can therefore afflict any part of the intestine, even the rectum and anus.
There are polyps of various sizes, from very small ones visible only by magnifying cameras, to much larger lesions clearly visible to the naked eye.
Bleeding is one of their classic symptoms, again due to the stool rubbing against them as they pass but, in certain cases, they can also bleed spontaneously.
Diverticulitis and inflammation of diverticula
Diverticula are extroversions of the colon, resembling small sacs that can form all along the intestinal wall.
They are not a pathology, nor a malformation, but a physiological abnormality, which may be congenital in nature or may develop later in life.
They do not give symptoms or pain, and often the carrier is completely unaware of their existence, and are usually revealed accidentally during a colonoscopy.
The condition of the presence of diverticula is called diverticulosis and, as mentioned, is not a pathological condition, and therefore does not require care or treatment.
When these small sacs, however, become inflamed, thus initiating a process of inflammation, the actual diverticular pathology, called diverticulitis, sets in.
Diverticulitis is thus the inflammation or infection of one or more diverticula, almost always caused by chyle fragments (the food that has already been digested by the small intestine and is ready to become alvo, i.e., stool) that have gone to settle in the indentation of the small sacs.
Diverticulitis is a bad experience for sufferers, and it manifests as very intense abdominal pain, cramping, fever, altered alvus, and, in about 5% of cases, intestinal bleeding.
This intestinal bleeding may therefore be copious, resulting in anal bleeding.
Acute diarrhea
Diarrhea is unformed, liquid or semi-liquid stool, a consequence of failure to reabsorb fluids properly in the intestines.
It appears when there is an intestinal imbalance, with a disruption of the regular convivial mechanisms of the bacteria that naturally inhabit the colon, such as during an infection caused by a toxin or a virus.
Diarrheal stools are malformed stools with high acid content (acidified), which, especially during the continuous discharges of the acute phase of diarrhea, irritate and tear the anorectal mucosa, thus possibly giving rise to bleeding episodes.
Many causes, always a symptom

Anal bleeding is thus a symptom, and never a cause in itself.
As we have seen in this article, there are so many diseases or otherwise pathological conditions that can give rise to anal bleeding, and the only way to get to the bottom of the problem is a serious proctological investigation.
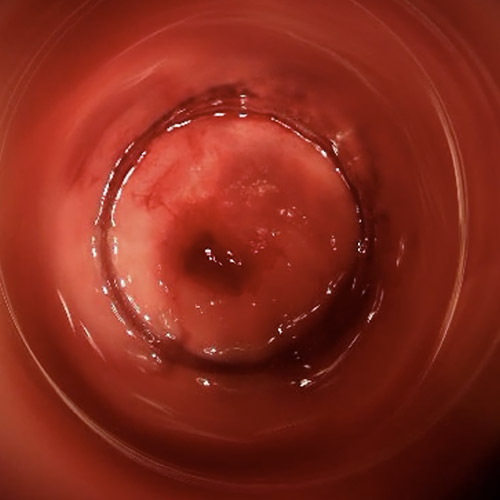
This investigation is carried out by means of the proctological examination, supplemented by a special examination called proctoscopy.
The Physician who specializes in all disorders of the anorectal canal, diagnosis of the cause of bleeding and its possible treatment is the Proctologist.
It is to him, therefore, that you should turn when you experience one or more episodes of anal bleeding, and you want to go and investigate the origin of the problem.
Do you suffer from anal bleeding in Dubai?
Don't be scared, dr. troyer can help you

Anal bleeding is often a condition that puts real fear into the patient, who becomes distressed and alarmed, even resorting to accessing the emergency room.
However, there is no need to be frightened, but to act reasonably, that is, by resorting to proctological examination.
At her clinic in Dubai, Dr. Troyer can help you discover the origins of your anal bleeding with a noninvasive, painless, fast and immediate-reporting exam called Electronic Endoscopic Videoproctoscopy.
Together with the Doctor, we will find the cause of your problem, and set up the appropriate remedial therapy.
All without pain or agitation: so that you are well, peaceful and calm.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- ANAL BLEEDING IS A CONDITION CALLED HEMATOCHEZIA, WHICH IS PART OF AN INTESTINAL PATHOLOGICAL PICTURE;
- IT IS NOT NORMAL TO LEAK BLOOD FROM THE ANUS DURING DEFECATION, AND IT IS NOT NORMAL TO FIND EVIDENCE OF IT IN THE STOOL;
- ANAL BLEEDING INDICATES AN INTESTINAL INJURY OR IN THE LAST PART OF THE COLON, I.E., RECTUM OR ANUS;
- MANY PROCOTLOGIC CONDITIONS CAN LEAD TO ANAL BLEEDING, SUCH AS PROLAPSED HEMORRHOIDS OR ANAL FISSURE;
- INTESTINAL INFLAMMATORY CONDITIONS, SUCH AS DIVERTICULITIS, CAN LEAD TO EPISODES OF ANAL BLEEDING;
- SOME AUTOIMMUNE DISEASES CAUSING FREQUENT EPISODES OF DIARRHEA, WHICH IN TURN IRRITATES AND TEARS THE ANORECTAL WALL CAUSING BLEEDING;
- ANAL BLEEDING SHOULD NOT CAUSE FEAR, BUT SHOULD PROMPT A PROCTOLOGICAL EXAMINATION

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.