Pregnancy is a special and delicate time for every woman.
The mother-to-be's body changes significantly-some of these changes are temporary, others permanent.
The new life growing inside the woman's uterus lives in total symbiosis with it, in a relationship that will remain indelible, in the new mother, truly for her entire existence.
Among the joys that a new pregnancy can bring, however, can also hide some pitfalls, often dictated by purely mechanical problems caused by the weight of the fetus and the amniotic fluid in which it forms.
Among these problems, undoubtedly vascular problems, and especially those related to hemorrhoidal prolapse, are undoubtedly among the most felt for pregnant women.
Pathological hemorrhoids, and their prolapse, are often related to pregnancy and, especially, to the time of delivery.
They are a problem for many pregnant women and new mothers, and this article was written by Dr. Luisella Troyer, Proctologist Surgeon, specifically to shed light on what to do if you have hemorrhoidal prolapse during pregnancy or shortly after delivery.
If you are a woman who is pregnant or about to give birth, you should therefore read this information page on hemorrhoids and their prolapse.
The intra-abdominal hyper-pressure that the fetus and amniotic fluid exert on the large abdominal vessels is not avoidable, just as the development of pathological hemorrhoids during pregnancy or delivery is not totally preventable.
However, there are good behavioral norms that the mother-to-be should follow to minimize the risk of hemorrhoid prolapse.
Such norms include proper diet and daily hydration,abstaining from tobacco use and alcohol,and keeping weight down throughout pregnancy.
The anorectal mucosa, already stressed by the mechanical hyper-pressure of the 'belly,' which increases its blood pressure, must be especially protected, and the first aid is precisely provided by the right production of soft, well-formedstools.
What are hemorrhoids?
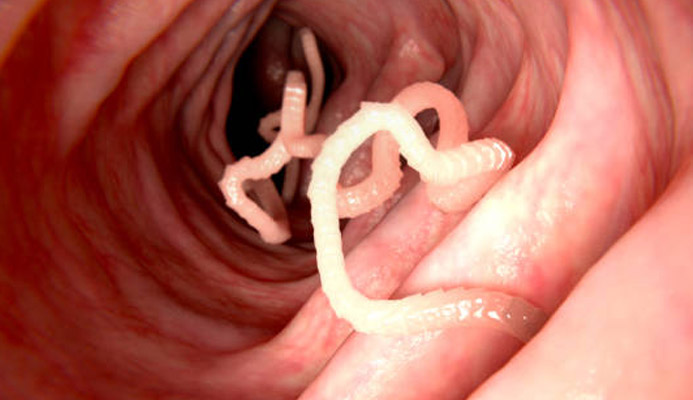
Hemorrhoids are small arteriovenous pads that occur naturally in our anal canal.
They are formed by both veins and arteries joined together, and their task is the proper vascularization of the entire anal canal.
Each of us has three main hemorrhoidal plexuses: right anterior, right posterior and left lateral, to which are added two smaller secondary plexuses.
Under normal conditions, the hemorrhoidal pads do not cause any discomfort, and they remain well within the anal canal, performing their function silently.
Only when hemorrhoids become inflamed, enlarged, lacerated, and prolapsed out of their original anatomical position can we speak of hemorrhoidal disease, or pathological hemorrhoids.
What is hemorrhoidal disease?

In Proctology, that is the specialized branch of Medicine that studies and treats all diseases of the anus and rectum, 'hemorrhoidal disease' means an unnatural condition of the hemorrhoids, which take on special and peculiar characteristics.
In hemorrhoidal disease, in fact, hemorrhoids are transformed and altered physiologically, and from silent pads become bulging, congestive, inflamed, often torn and prolapsing extrusions out of their original anatomical position.
As they become increasingly swollen with blood, the hemorrhoids increase in weight, and this worsens the exhaustion of the supporting structures that hold them anchored to the side of the anal canal, thus causing them to slowly slide downward (hemorrhoidal prolapse).
Hemorrhoidal prolapse can be of four stages of severity:
- Stage I, mild prolapse, where the hemorrhoids are all still inside the anal canal;
- Stage II, moderate prolapse, where the hemorrhoids extrude out of the anal canal only during pontication of defecation or only during some straining;
- Stage III, severe prolapse, where the hemorrhoids spontaneously extrude out of the anus but can still be repositioned inside the same by manual maneuvering;
- Stage IV, severe prolapse, where the hemorrhoids are permanently prolapsed outward
Pathological hemorrhoids are, along with dental caries, the most prevalent disease worldwide: this gives an idea of the phenomenon globally, even considering that, very often, the clinical condition of hemorrhoidal disease is under-diagnosed.
What is hemorrhoidal disease caused by?

There is still no unified explanation to describe the cause of hemorrhoidal prolapse.
Science has not yet arrived at a common answer, but two main macro-causes are suspected:
- A mechanical problem (mechanical theory), which wants the collagen-rich supporting tissues of hemorrhoids to naturally wear out due to physiological aging, and specific lifestyles or diseases, such as chronic constipation;
- A blood flow problem (hemodynamic theory), which wants the hemorrhoid plexuses to bulge and wear out due to hyper-increased blood flow, which in turn is caused by increased intra-abdominal pressure, lifestyles or particular periods (such as obesity, pregnancy, childbirth, some strenuous work, etc.).
It should necessarily be noted that these two theories are not at odds with each other, and that the general cause of the onset of hemorrhoidal pathology may be due to both conditions.
To these two main theories then, Medicine has for many years ascertained the presence of certain triggers of pathological hemorrhoids, which are often the 'initial spark' of hemorrhoid prolapse.
Such triggers are:
- Chronic constipation, never treated;
- A diet low in fiber and right hydration;
- Irritable bowel syndrome;
- The continued practice of anal sex;
- Familial predisposition to chronic venous insufficiency;
- The state of obesity;
- Smoking and excessive alcohol consumption;
- Pregnancy and childbirth;
- Some sports such as weightlifting;
- Some heavy-duty work, or work that requires long periods on your feet;
- The lack of physical activity, especially of daily walking;
- Physiological aging and the decline in collagen production
As can be seen from the list, almost all of these triggers include increased intra-abdominal pressure, which in turn can result in hyperblood supply to the hemorrhoid plexuses, which therefore become exhausted and over-swollen with blood.
Pregnancy and childbirth are, for women, the periods when this intra-abdominal pressure is considerable, and therefore the risk of developing hemorrhoidal disease is substantial.
The Physician who can help the future or new mother who has developed pathological hemorrhoids in pregnancy or after childbirth is the Proctologist Physician.
Such a health professional is usually a Vascular Surgeon, or at any rate a Physician from another surgical specialty, who is particularly experienced in treating conditions that may afflict the rectum or anus.
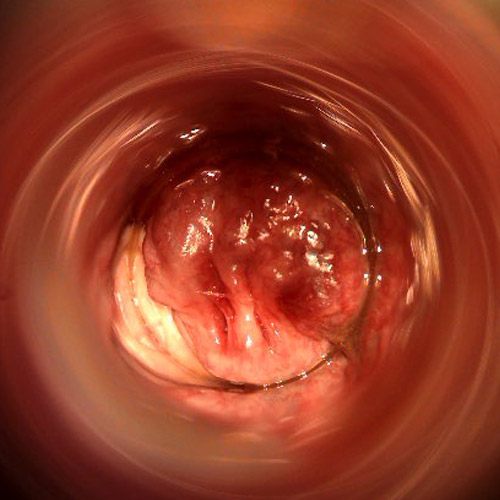
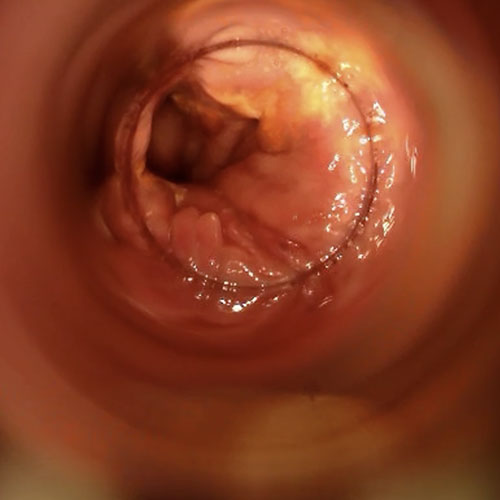
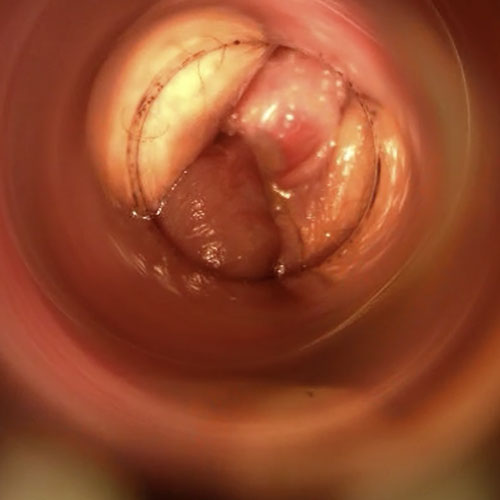
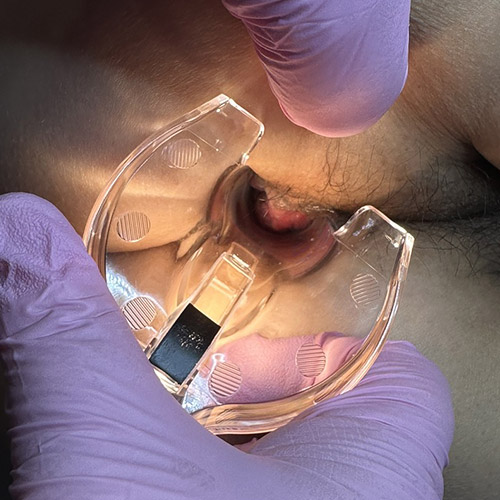
Pathological hemorrhoids are diagnosed by proctological examination, that is, the specialist examination that can analyze the condition of the rectum and anus.
This examination is always accompanied and complemented by the proctoscopy examination, in which the physician goes to investigate the patient's anorectal canal, looking for the origin of the symptoms reported in the history phase.
Pregnancy and increased pressure on the abdomen
As is well known, in mammals, of which Homo Sapiens is a part, the female of the species is the one in charge of gestating the offspring, after being fertilized by the male's seed.
Unlike other animals, mammals do not lay eggs, but the gametes, that is, the reproductive cells of the species, 'meet' and initiate life in the uterus of the female after sexual mating.
The uterus is, succinctly, a containing organ, capable of swelling and expanding in considerable size, and thus becoming the 'containing sac' of the forming embryo, which will later become a fetus and, at birth, a child.
Embryo formation is endogenous therefore in our species and in mammals in general, and takes place in the uterus, itself located roughly in the woman's lower abdomen.
To protect the fetus during gestation, as well as provide the new life with a safe and 'anti-shock' environment, the uterus fills with a special fluid called amniotic fluid.
This fluid increases in quantity over the course of gestation, following the growth of the fetus: from a few milliliters during the first few weeks of pregnancy, a pregnant woman will grow to contain about one liter of amniotic fluid toward the end of gestation.
To this fluid should be added the weight of the fetus, which varies from person to person, but averages close to 3 kg towards the last weeks.
It is therefore normal for the pregnant woman to gain weight in general, but here is a specific problem: the increase does not occur harmoniously throughout the body, but only at a specific point.
Such a point is, of course, the abdomen and lower abdomen.
This accumulation of many pounds hyper-concentrated on the abdomen often causes, to the mother-to-be, some problems during gestation, for a very simple reason: the load of the baby and the amniotic fluid is on a point of the body where many important vessels pass through, draining blood and lymph from the lower limbs.
These are the great abdominal vessels, which we all have and which pass right at the abdomen and pelvic area: the vena cava, the iliac veins, the abdominal lymphatic duct.
These vessels, important because they act as 'main highways' for venous and lymphatic flow, can be compressed and congested by the very uterus that has grown to enormous proportions, containing the fetus and its amniotic fluid inside.
This congestion in turn causes abdominal hyper-pressure, likely resulting in slower venous and lymphatic circulation.
This slowdown often causes pregnant women to experience problems with swelling and heaviness in the legs and, especially with a family predisposition, the appearance of telangiectasias, varicose veins and hemorrhoidal prolapse.
Congestion of the large abdominal vessels increases progressively as gestation increases, reaching delivery as the peak of intra-abdominal pressure.
It is precisely during the delivery, often in predisposed patients, that the 'outbreak' of hemorrhoid pathology therefore occurs: the supporting tissues of the hemorrhoids, already exhausted by nine months of pregnancy, finally give way, thus allowing for an overflow of blood and the onset of prolapse.
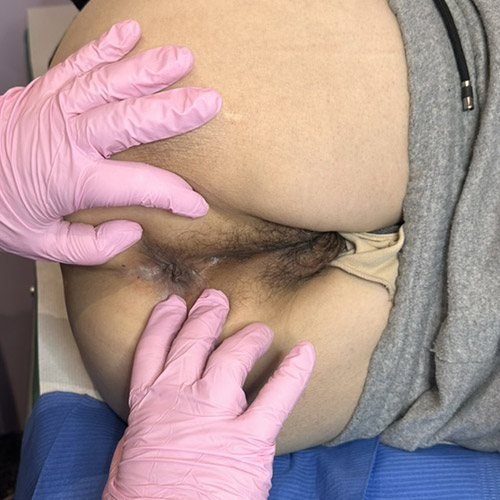
Sometimes, such onset of prolapse is particularly traumatic for the woman, who immediately after delivery experiences congestive, inflamed hemorrhoids almost completely outside the anal canal.
Many of these stages are fortunately reversible and transient; however, some are permanent, and are the source of future proctological problems for the new mother.
Could the onset of hemorrhoidal disease in pregnancy be due to genetic predisposition?
Yes, prolapse of hemorrhoids during pregnancy or childbirth may be caused by chronic venous insufficiency, that is the disease that slowly damages and deforms the veins and leads to the formation of varicose veins.
This condition is largely hereditary: of course, one does not inherit varicose veins, but the quality of the vessel endothelium tissues, which are much poorer in collagen and less elastic than average.
It takes relatively little for inelastic, collagen-poor inner venous walls to become deformed and permanently damaged, thus initiating the venous reflux that is the main cause of varicose vein extrusion.
Even in hemorrhoids, because they are arteriovenous tissues, although they do not have internal valves as in common veins, genetic predisposition can cause the tissues to become exhausted and damaged, thus initiating plexus prolapse.
During pregnancy, in patients predisposed to vascular problems, thus with mom and/or dad already having manifest varicose veins, the fetus's hyper-pressure on the large abdominal vessels can slow venous circulation, cause reflux and, thanks to the low quality of the internal tissues of the hemorrhoids, wear them down and thus give rise to hemorrhoidal disease.
Sometimes, the trigger of maximum danger, which triggers hemorrhoid discharge, is precisely the point of maximum possible intra-dominal pressure: the moment of delivery, and of the woman's necessary 'pushing' to get the baby out.
Can extruded and swollen hemorrhoids after childbirth return to their rightful place?

Hemorrhoidal prolapse is classified according to a four-grade scale, which in turn is directly related to the volume of hemorrhoids:
Grade I hemorrhoids
The prolapse is initial, and the hemorrhoids still result totally in the anal site;
Grade II hemorrhoids
The prolapse is contained, and the hemorrhoids come out of the anal canal are during defecation or some physical exertion, and then immediately return to their seat independently;
Grade III hemorrhoids
Prolapse is severe, and the hemorrhoids come out of the anal canal spontaneously, but can be repositioned with manual maneuvering;
Grade IV hemorrhoids
Prolapse is irreducible, and hemorrhoids are permanently prolapsed outside the anal canal
Knowing the severity of hemorrhoidal prolapse is essential in order to provide a diagnosis and, more importantly, a reliable prognosis for the new mother who has developed hemorrhoids in pregnancy or during delivery.
Indeed, the reduction in prolapse of hemorrhoids is dependent both on their severity status and, playfully, on the new mother's age, and her quality and quantity of collagen production (and ability to repair damaged tissue).
Mild stage prolapses, then grade I or II, can usually be cured with the right sphincter therapy and diet modification, adding the use of effective flavonoid supplements to the therapy.
Prolapses beyond Stage III often require more radical solutions, sometimes involving removal or total destruction of the now diseased plexuses.
Immediately after childbirth, even for women who are not predisposed, it is still judged normal to witness at least some inflammation and congestion of the hemorrhoid plexuses, even not in an already 'pathological' situation.
Straining during childbirth and a massive increase in intra-abdominal pressure can lead to temporary congestion of the plexuses, which, however, (always assuming good tissue elasticity) can spontaneously flare and shrink.
Other times, however, the damage is irreversible, and the hemorrhoidal disease becomes chronic.
Is there any way to prevent hemorrhoids during pregnancy?
The future mother's genetic predisposition to vascular problems, of course, is not preventable.
Healthy lifestyles during gestation and precise control of body weight are also certainly very useful and recommended acts, but by themselves they cannot totally prevent the occurrence of hemorrhoidal prolapse.
Often, mothers who have been flawless during pregnancy and have never had hemorrhoid problems throughout gestation suddenly develop a large prolapse during delivery, or soon after.
This was due to the intra-abdominal pressure just during labor and delivery, which can quickly defibrate and damage the supporting tissues of hemorrhoids, even without having experienced previously 'suspicious' conditions.
Certainly maintaining proper weight, the use of any phlebotonic supplements and, in women predisposed to venous insufficiency, prophylactic heparin therapy can reduce the risks of venous disease, but they still cannot eliminate them altogether.
The use of preventive and palliative elastic stockings, which is very effective in providing immediate relief to the legs of pregnant women, is of little or no benefit to the blood circulation of the hemorrhoid plexuses, so it cannot be considered a preventive attitude.
In the current state of Medicine, it should therefore be ascertained that the development of hemorrhoidal prolapse during pregnancy is yes facilitated by a genetic predisposition and the mother's behaviors, but it is a largely random element that can occur even in case of perfect patient compliance.
How can hemorrhoids be treated after pregnancy and childbirth?
The treatment of pathological hemorrhoids developed during pregnancy and childbirth is related to their severity status.
During pregnancy, treatment is exclusively palliative, as any medical or surgical intervention is impossible until the woman has completed gestation.
To provide relief for the mother-to-be, the Proctologist can prescribe systemic flavonoid supplements and topical soothing creams, not forgetting to remind the patient of the importance of adequate daily fluid supplementation and a diet rich in fiber.
Foods that are spicy or otherwise irritating to the intestinal mucosa are also avoided, and the goal is to bring the patient to the expulsion of soft, well-formed stools that are easy to expel and therefore do not further increase intra-abdominal pressure.
Ointments containing local anesthetic or cortisone should be avoided, in favor instead of soothing creams with inflammatory action and phytotherapeutic active ingredients (such as creams containing calendula or propolis).
Even immediately after childbirth, with hemorrhoids generally congested and inflamed (sometimes, even injured), it is imperative to provide for de-inflammation of the tissues, allowing them to regenerate and repair themselves, of course to the extent possible.
In many cases, inflammatory treatment of hemorrhoidal prolapse, if well prescribed, succeeds in completely resolving low-grade, and sometimes even higher-grade prolapses, especially if the patient is still young and with good collagen production.
The postpartum diet should also be prescribed by the proctologist and diligently implemented by the new mother, again to avoid episodes of constipation, which would worsen the clinical picture, and instead obtain soft, easy-to-evacuate stools.
Evaluation on medical or surgical interventions of the now irreparably prolapsed hemorrhoids is usually done at the end of puerperium, then at the end of breastfeeding.
There it is possible to take stock of the situation, and with the obligatory proctologic examination, the Proctologist Surgeon will be able to propose the most suitable treatment plan to the patient, considering that, in recent years, the treatment of hemorrhoids has been completely disrupted by the introduction of the new sterilized air-stabilized scleromousse.
A painless treatment with success rates equal to those of Surgery, but without requiring the patient to have surgical access.
Do you suffer from hemorrhoids developed in pregnancy or during childbirth? Dr. Troyer can help you

Dr. Luisella Troyer is a Proctologist Surgeon in Dubai, who has been perfected for many years in the treatment of hemorrhoidal pathology affecting pregnant women or women who have just given birth.
At her office in Dubai, Dr. Troyer can give you immediate relief from your hemorrhoids, as well as plan with you the right palliative therapy that will help you end your pregnancy without pain or discomfort.
If you have already given birth and are suffering from postpartum hemorrhoidal prolapse, Dr. Troyer can also help you get well, treating you and allowing you to return to your usual, pain-free life.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- HEMORRHOIDS ARE NORMAL VASCULAR PLEXUSES FOUND IN THE ANAL CANAL;
- THE PLEXUSES OF HEMORRHOIDS ARE COMPOSED OF BOTH VEINS AND ARTERIES, JOINED TOGETHER SEAMLESSLY;
- THE MAIN TASK OF HEMORRHOIDS IS TO PROPERLY VASCULARIZETHE ANAL CANAL;
- WE SPEAK OF HEMORRHOID PATHOLOGY ONLY WHEN HEMORRHOIDS BECOME INFLAMED, SWELL AND EXTRUDE FROM THEIR ORIGINAL POSITION;
- HEMORRHOIDS MAY PROLAPSE AND BECOME CONGESTED DUE TO MECHANICAL OR HEMO-DYNAMIC CAUSES , SUCH AS CHRONIC CONSTIPATION, PREGNANCY, CHILDBIRTH, OR NATURAL AGING;
- PREGNANCY AND GESTATION ARE PERIODS OF CHANGE IN A WOMAN'S BODY;
- DURING PREGNANCY THE WEIGHT OF THE FETUS AND ITS AMNIOTIC FLUIDOGRAVAON THE WOMAN'S LARGE ABDOMINAL VESSELS, CONGESTING THEM;
- CONGESTION OF THE LARGE ABDOMINAL VESSELS AND THE WEIGHT OF THE FETUS INCREASE THE INTRA-ABDOMINAL PRESSURE OF THE MOTHER-TO-BE'S BODY;
- INCREASED INTRA-ABDOMINAL PRESSURE MAY BE THE TRIGGER FOR THE ONSET OF HEMORRHOIDAL DISEASE;
- THE TIME OF DELIVERY IS WHEN INTRA-ABDOMINAL PRESSURE PEAKS, AND MAY THEREFORE BE THE TIME WHEN HEMORRHOIDAL PLEXUSES EXTRUDE;
- THERE IS A DEFINITE GENETIC COMPONENT THAT MAKES ONE PREDISPOSED TO THE ONSET OF DISEASES OF THE VENOUS SYSTEM AND ALSO HEMORRHOIDS;
- THE TREATMENT OF HEMORRHOIDS IN PREGNANCY IS EXCLUSIVELY PALLIATIVE, AIMING TO MAKE THE MOTHER FEEL BETTER;
- PERSISTENT HEMORRHOIDS EVEN AFTER DELIVERY CAN BE TREATED, IF CLINICALLY INDICATED, WITH STABILIZED SCLEROMOUSSE

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.