Do you have unbearable pain in your anus or anal area that is excruciating and for which anti-inflammatories and antibiotics seem to have no effect?
Do you notice purulent material coming out of the anus, or perianal area, and don't know where to turn for medical help and support?
Perianal abscess is one of the most common proctologic emergencies, often considered nondeferrable: the pain and prostration it creates dictates immediate, surgical treatment.
Read this page to find out what perianal abscess is: what it is caused by, how to intervene, and who is the Physician who can provide the right health care support.
The thong is undergarment that is very fashionable among the young female population and have primitive origins.
Both provide essentially genital protection, leaving the buttocks exposed instead (partially in the thong, totally in the thong).
They are tribal-concept garments designed, at least originally,to provide minimal genital protection, leaving the buttocks uncovered (for practical reasons, e.g., convenience of movement and for rapid defecation).
Nowadays, the thong and thong are used almost exclusively for fashion, often to openly display the buttocks by way of sexual appeal (innate but extremely complex in our Sapiens species).
A considerable number of perianal abscesses, to which sebaceous cysts and anitis are added, arise precisely from the use of these garments, since the string that secures the undergarment to the waist excessively stimulates precisely the perianal skin, rubbing it continuously and, therefore, irritating it.
This can then be the beginning of the trauma that can lead to infection of a mucus gland, thus triggering perianal abscess.
This is why it is important to wear comfortable underwear, well-fitting but not excessively tight, preferably of non-dyed cotton.
Aesthetics perhaps lose out a bit, but you can on the other hand minimize the risk of painful problems.
What is perianal abscess?
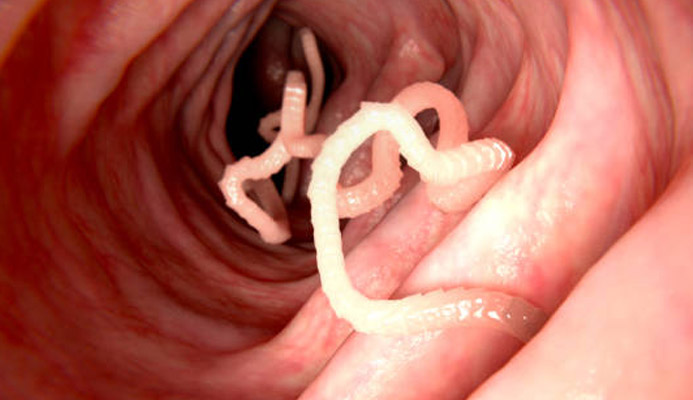
Perianal abscess is a process of acute infection of one of the glands of the perianal mucosa, exactly the glands of Hermann and Defosses, located a short distance from the anal orifice, or rather its outer margin.
These glands, located between the internal and external sphincters, are responsible for producing adequate amounts of mucus, which in turn is needed to lubricate and protect the delicate anal mucosa.
When, for reasons we will see later, one or more of these glands become infected, there is then the onset of what is called a perianal abscess.
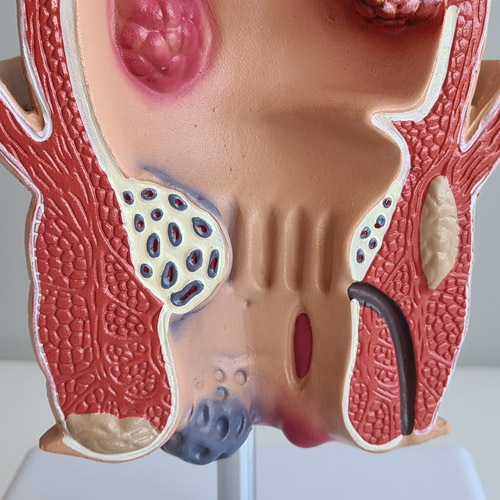
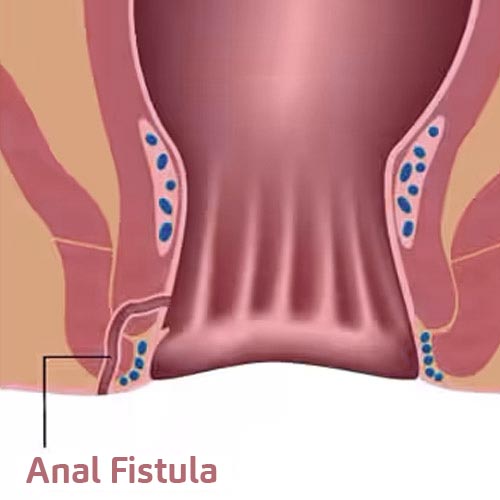
Perianal abscess is a condition that soon becomes extremely painful and, if neglected, can lead to the formation of a dangerous and equally painful anal fistula.
What are the causes of perianal abscess?
The perianal abscess depended on a bacterial infection to one of Hermann's and Defosses' glands, resulting in suppuration and formation of purulent material.
Given that these glands have no surface access outlets, but reside between the two sphincter muscles, the infection soon turns into an abscess, which is extremely painful and, if left untreated, in many cases leads to the formation of an artificial vent channel, called a fistula.
On the causes of this bacterial infection, Medicine has been debating for a long time.
At present, no single primary cause has been found, but a number of concurrent causes that may lead to a plausible explanation of the infectious phenomenon.
Among these triggers, we can mention:
- Repeated trauma of the anal and perianal area;
- Chronic constipation or chronic diarrhea;
- A hypertone of the internal anal sphincter;
- Poor hygiene of the anal and perianal area;
- Fecal incontinence and the resulting inability to keep the anus clean at all times
In general, therefore, it is clear to note that any situation in which the perianal mucosa is stressed and facilitated in the processes of inflammation is a clear invitation for bacteria, which can thus infect the mucus glands and give rise to infection.
What are the symptoms of a perianal abscess?
The main symptom of perianal abscess is the intense pain that develops in the anal area, which the patient often reports as unbearable.
The pain is visually associated with swelling from the perianal area origin of the abscess, with swelling and redness as well as intense heat of the skin.
To the touch, the area appears semi-fibrotic, extremely hot and sore, so much so that digital inspection of the anus is impossible.
If there has already been fistulization, there will be a small artificial orifice, either central or even located elsewhere than in the abscess edema, from which purulent, foul-smelling material will gush out.
Such suppuration, in addition to a fistula outside the anus, may also leak from the anal canal itself.
Accompanying this local symptomatology, perianal abscess is often associated with fever, exhaustion, difficulty evacuating (also due to severe pain in the anal area), sometimes even blood loss (hematochezia).
A perianal abscess can happen to anyone, but often lesions (even small ones) of the perianal mucosa are associated withrepeated traumatic eventsover time, such as those caused by constant use of a bicycle, motorcycle, orhorseback riding.
Diseases of the anal area, such as hemorrhoids, fissures, proctitis, or poorly treated anitis, can also promote the initiation of a perianal abscess.
How is a perianal abscess diagnosed?
Diagnosis of a perianal abscess is essentially clinical: an inspection of the perianal area is enough for the experienced proctologist to immediately identify the abscess.
Digital inspection and proctoscopy is not always possible at diagnosis because the extreme pain, even at the slightest contact, felt by the patient does not make the examination easy.
Endoanal ultrasound is the instrumental examination of excellence regarding perianal abscess, which time has defined as superior in diagnostic accuracy to MRI or CT scan.
What is the treatment for perianal abscess?
Perianal abscess is exclusively a surgical competence, and therefore must be resolved surgically.
The use of antibiotics or anti-inflammatories is not sufficient to resolve the abscess; in fact, it is often not recommended.
Surgical treatment, often performed as an emergency due to the prostration and unbearable pain the patient experiences, involves an incision of the swelling, wide enough to allow purging of the pus and subsequent dressings.
The primary purpose of surgery is to clean out the infected area, removing all traces of bacteria or pus.
This is done by washing with hydrogen peroxide and/or Betadine, and if fibrin is present within the abscess, it is removed by gentle curettage.
The wound is not sutured, but rather left open and blown open with gauze, to be changed daily.
Dressing is to be done daily until the wound is completely healed, per second intuition.
In uncomplicated abscesses, this is sufficient to allow the wound to heal, but in case of fistulization (present in about 20% of abscess cases), it is then necessary to provide appropriate specillation and insertion of a seton or, more modernly, laser cauterization of the fistula by VAAFT (Video Assisted Ana Fistula Treatment) technique.
In any case, even healed perianal access must be kept under control over time: in fact, in a not inconsiderable number of cases, posthealing fistulization is an unpreventable complication, thus necessitating a second specific surgical therapy (e.g., fistulectomy).
Is there anything that can be done to prevent the formation of perianal abscesses?
Scientific evidence has established that perianal abscesses are very common in cases where the area of the anus (and buttocks in general) often suffers continuous trauma, even minor trauma.
Again, chronic phlogosis of the anal mucosa and perianal skin, common in cases of chronic constipation or chronic diarrhea (a frequent symptom in patients with irritable bowel syndrome, for example) can lead to infection of the mucus glands, thus originating the abscess.
Prevention, therefore, is related to preventing these situations considered as triggers of perianal abscess.
Appropriate and adequate anal and perianal hygiene is also considered of paramount importance in preventing abscess of Hermann's and Defosses' glands.
In fact, the constant presence of feces in the anal orifice can inflame the mucosa, causing inflammation and, consequently, probable bacterial access and initiation of infection.
Are you suffering from a perianal abscess in Dubai? dr. troyer is an Emergency proctologist Surgeon, she can help you

If you experience symptoms of a perianal abscess, you can call Dr. Troyer for quick support, including surgical access.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- PERI-ANAL ABSCESS IS THE INFECTION OF A HERMANN AND DESFOSSES GLAND, I.E., A MUCUS GHINADOLA OF THE PERI-ANAL AREA;
- THE MUCUS GLAND USUALLY BECOMES INFECTED BY MINOR TRAUMA, OR SMALL BUT CHRONIC INFLAMMATION OF THE PERI-ANAL SKIN;
- PERIANAL ABSCESS CAN ALSO BE TRIGGERED BY WEARING INAPPROPRIATE UNDERWEAR, SUCH AS A THONG OR THONG;
- MUCUS GLAND INFECTION, HAVING NO EXTERNAL ACCESS, IS EXTREMELY PAINFUL, AND CAUSES EVEN HIGH FEVER, EXHAUSTION, AND PROSTRATION;
- THE ONLY POSSIBLE TREATMENT FOR THE PERI-ANAL ABSCESS IS SURGICAL, AND INVOLVES INCISION WITH THE PUS COMING OUT;
- IF CAUGHT LATE, THE PERI-ANAL ABSCESS CAN DEGENERATE INTO A PERI-ANAL FISTULA;
- PERI-ANAL FISTULA CAN OCCUR EVEN IF EARLY INTERVENTION IS TAKEN IN AN ABSCESS, AS A COMPLICATION OF HEALING;
- THE USE OF ANTIBIOTICS OR ANTI-INFLAMMATORIES IS ALMOST USELESS IN A PERI-ANAL ABSCESS, AS THEY ARE NOT VERY EFFECTIVE;
- PERI-ANAL ABSCESS IS ONE OF THE MOST COMMON PROCTOLOGIC EMERGENCIES

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.