As has been known to science for some time now, our body is not a closed organism in relation to its surroundings.
In fact, in addition to the common daily interactions of feeding, in which we essentially take energy that has already been chemically processed by other biological beings, our organism in turn harbors a large number of very small life forms that in return exploit the biological waste or residues produced by our metabolism.
Candida albicans, a yeast belonging to the large family of Saccharomycetes fungi, is precisely one of these microorganisms that live on and in our bodies, which results in a very comfortable environment for them to find abundant nourishment.
Normally Candida albicans is a fungus that is harmless to us: it feeds on the waste products of our metabolism and indeed, by its presence keeps out other far more malevolent microorganisms that might colonize and infect our tissues.
In certain situations, however, this useful yeast can grow and proliferate uncontrollably, initiating what is called candidiasis.
When candidiasis afflicts the mucous membranes of the anus and perianal skin, it is more properly called anal candidiasis.
Read this page to find out what anal candidiasis is, how it is diagnosed, and how you can prevent it.
Statistically, anal candidiasis is a more common pathological condition in women than in men.
The cause of this statistical preference is due to a woman's hormonal cycle , which in turn is the frequent cause of lowered immune defenses and the danger of developing candidiasis.
Again, taking the birth control pill greatly increases the risk of developing vaginal candidiasis, which is common in more than 60 percent of women on hormone therapy.
Given that the vagina and anus, in women, are very close together, the risk of self-inoculation of the fungus spores into the anal mucosa is very high, hence the higher percentage of possibility of anal candidiasis.
What is Candida albicans?

Candida albicans is a fungus, more precisely a yeast, belonging to the large family Saccharomycetes.
Like all fungi, its life cycle is based on parasitism, specifically the digestion of sugars produced by other biological organisms in a well-known process called fermentation.
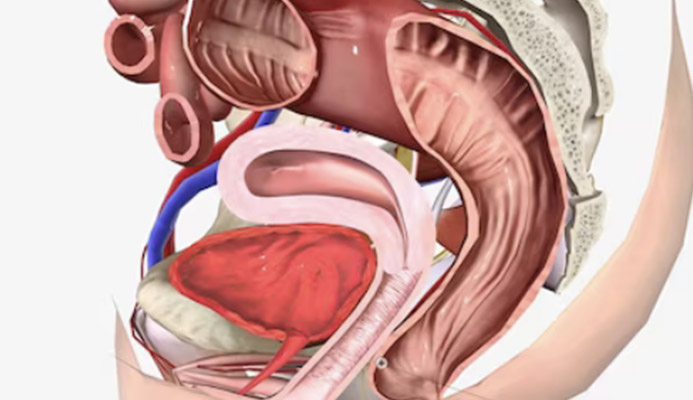
Candida is present in large numbers in our oral cavity, in our gastrodigestive tract (intestines and colon), and on our ano-genital skin, thus anal orifice, penis, testicles, and vagina.
Under normal conditions, candida is a fungus that lives by feeding on the organic wastes it finds in our oral cavity, intestines or superficial skin, and is not a pathological microorganism.
On the contrary, its presence is beneficial to our immune system, as it keeps out other potentially pathogenic bacteria or fungi that could take Candida's place if it were not already present.
Only under exceptional conditions, in which there is hyper-proliferation of the yeast, is one already properly speaking of candidiasis.
What is candidiasis?
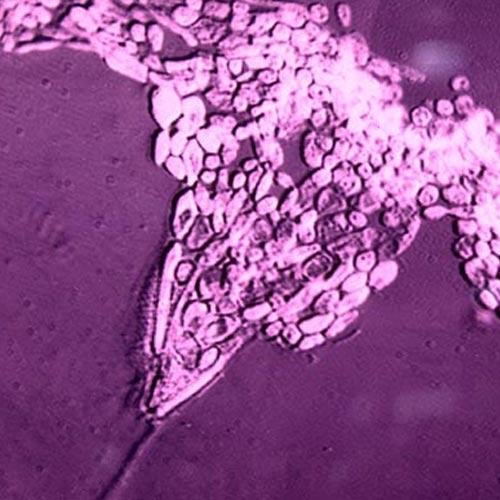
Candidiasis is a pathological condition, caused by the excessive and uncontrolled proliferation of the fungus Candida albicans.
Normally, the immune system is able to keep the candida fungus at bay, preventing it from proliferating excessively, and thus confining it to precise areas of the gastrointestinal tract or skin, where it stays and lives as a saprophyte (digesting the waste products of our metabolism).
When this does not happen, and the candida fungus replicates abnormally and uncontrollably, it is called candidiasis, which is a real disease with specific symptoms.
Why does candidiasis occur?
Candidiasis, as mentioned a little above, is an unbalanced condition of the Candida albicans fungus, normally found in our mouth, in our intestines, and on our genitals.
The reasons for its uncontrolled replication are always attributable to a decided lowering of immune defenses, which allow the fungus to hyper-proliferate beyond physiological limits of equilibrium.
This lowering of immune defenses is in turn related to external causes or over-infections, viral or bacterial, such as:
- A long antibiotic treatment, which seriously lowered the quantity and quality of the intestinal microbiota (natural antagonist of Candida albicans);
- A severe bacterial infection, such as pneumonia, or another infectious disease that is particularly trying for the body;
- Alcoholism and smoking;
- Diabetes mellitus;
- A situation of malnutrition or incorrect and deficient nutrition;
- HIV infection not treated with the right antiviral therapy;
- A prolonged period of stress, both physical and psychological;
- A chemotherapy or radiation therapy;
- The presence of an aggressive tumor attack;
- About hormonal surges;
- Taking the birth control pill;
- Sexual intercourse with a partner with urogenital or anal candidiasis
Whatever the primary cause of the lowered immune defenses, it should be intercepted and diagnosed by the physician at the time of history taking, as therein lies the root of candidiasis overinfection.
Steroid molecules, thus containing cortisone, are a particularly welcome 'food' for fungal parasites, and candida fungus is no exception to the rule.
Anal and peri-anal candidiasis caused by the immoderate use of topical cortisone creams is in fact a common problem in patients with hemorrhoidal disease, who often refuse to visit the Proctologist and, as a substitute, turn to the pharmacist who, often, does not skimp on selling them cortisone creams.
The result is a sensitization of the anal and peri-anal area that, over time, not only causes violent dermatitis, but also induces candida fungi to hyper-proliferate, content with the fact that there is much more nutrition suitable for them (the cortisone molecules).
Anal candidiasis due to inordinate use of topical cortisone creams and preparations is a frequent problem in patients with pathological hemorrhoids, and is often a secondary symptom related to hemorrhoidal prolapse.
Can candidiasis be transmitted?

No, Intestinal candidiasis is not a communicable disease.
Urogenital candidiasis, or even anal candidiasis, on the other hand, is transmissible through sexual intercourse, and therefore falls under the list of Sexually Transmitted Diseases.
What are the symptoms of candidiasis?
The symptoms of candidiasis vary greatly depending on its location and, no less, also depending on the patient's sex and age.
In young children, it often occurs in the oral cavity, where it is called thrush, with typical yellowish-white, plaque-like lesions.
On the skin, in both adults and children, candidiasis takes the form of whitish, often crumbly scaling that may or may not be itchy.
In the intestinal mucosa, the fungus can reach the bloodstream and release its toxins, which give a wide range of symptoms, such as:
- Diarrhea or constipation;
- Poor digestion;
- Perennial fatigue or drowsiness;
- Irritability and depression;
- Abdominal bloating;
- Insomnia and recurrent headaches
These symptoms, as you can see are very varied, are often compounded by poor absorption of intestinal villi, invaded by the candida fungus, which in the long run can cause malnutrition.
In the female genital site, urogenital candidiasis most often involves burning, itching, a feeling of perpetual and impending need to urinate, and, last but not least, pain during the penetrative sexual act.
These symptoms are part of the more general picture of vaginitis, a condition that frequently afflicts many young women on birth control therapy.
In men, urogenital candidiasis is often asymptomatic, but when it becomes symptomatic, scaly lesions of the penis, especially the glans, can be appreciated, often itchy.
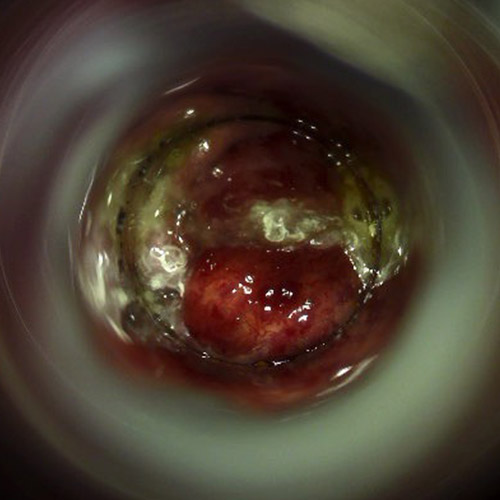
Anal candidiasis, on the other hand, is manifested as violent proctitis (inflammation of the anus and rectum), which makes the anal mucosa and perianal skin reddened, painful to the touch, and itchy.
Such anal itching is often reported as unbearable, and it also adds to anal burning during evacuation.
What is anal candidiasis?
Anal candidiasis is the localization in the anal and perianal site of candidiasis.
It can occur in both men and women, and is always dependent on a hyper-proliferation of the Candida albeicans fungus, which in turn is caused by lowered immune defenses but, unlike intestinal candida, sometimes by unprotected sexual intercourse.
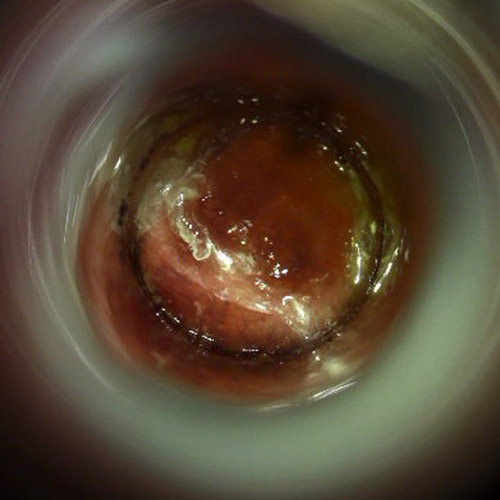
Its symptoms are those of proctitis, i.e., inflammation of the perianal area, anal orifice, and rectum, making the mucosa reddened, easily lacerated, often bleeding, sometimes with the presence of whitish-yellowish lesions that, easily removed, recur shortly thereafter.
Proctitis caused by candidiasis irritates all anorectal tissues, and this causes continuous burning and tingling, especially during evacuation, which is association with intense anal itching.
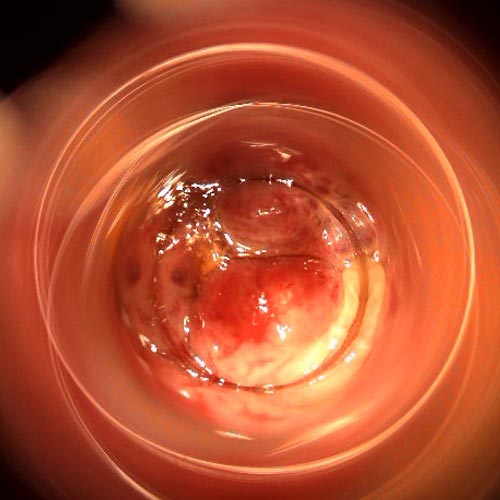
Before the development of Electronic Endoscopic Videoproscopy, the only reference and highly reliable examination for the diagnosis of anal candidiasis was the videocolonoscopy.
This is a fairly invasive examination, which moreover requires troublesome preparation, and is in any case exaggerated to investigate only the anus and rectum.
Videoproscopy has solved this problem: it is a fast, no-preparation, noninvasive examination that can immediately visualize all candidiasis lesions in high resolution.
How is anal candidiasis transmitted?

In women, almost all cases of anal candidiasis are by self-inoculation, that is, by transmission of the fungus spores from the nearby vagina, which thus results in the focus of infection.
In turn, vaginal candidiasis is often caused by a hormonal change, often dictated by the birth control pill (about 60 percent of women on birth control therapy experience this symptom).
However, infection from sexual intercourse with a (often, asymptomatic) partner with a high fungal load cannot be ruled out.
In men, anal candidiasis is rarely dependent on sexual intercourse or a hormonal surge, but rather on a drastic lowering of immune defenses, such as after prolonged antibiotic treatment over time.
How is anal candidiasis diagnosed?

Diagnosis of anal candidiasis is not easy, as the symptomatology of the infection may be confused with that of other proctological diseases (e.g., chemical or bacterial dermatitis, or even hemorrhoidal prolapse).
In addition to proctologic inspection, it is imperative that the Proctology Physician perform a rigorous medical history, which must take into account any collateral symptoms of the patient, his or her lifestyle and sexual preferences and habits.
The examination is completed with the required Electronic Endoscopic Videoproscopy, where the Proctologist Physician, using a proctologic inspection tube and high-definition video camera, scans the entire anorectal tract, looking for the presence of the typical whitish, friable lesions of Candida albicans.
Coproculture, i.e., the fecal culture test used to investigate the presence or absence of the fungus in fecal waste may be recommended, but in itself is not indicative for diagnosis, as remnants of Candida yeast are normally present in our alvus.
Biopsy of the anorectal canal allows a more precise diagnosis, but since it is an invasive test, the physician tries to avoid it if possible, resorting to it only when first-line therapy for candidiasis fails.
What is the treatment of anal candidiasis?
The treatment of anal candida is not dissimilar to that for intestinal or urogenital candida, and is essentially based on the administration of antifungal drugs, both systemic and topical.
The dosage of therapy is modulated by the proctologist depending on the extent and severity of candidiasis, the patient's immune response, the presence or absence of parallel overinfections, and, of course, the patient's overall health status.
Generally, the antifungal drugs of first use are fluconazole, itraconazole and voriconazole, with the latter active ingredient (very strong) used as a last resort only in the case of persistent infections.
These drugs can be administered either orally or topically, in the form of creams to be applied to the anal and perianal area, or a combination of the two modalities.
It must necessarily be emphasized that along with the reduction of the fungal load of Candida albicans, it is imperative for the Proctologist Physician to also investigate and resolve any pathologies or disease states that originate from the patient's lowered immune system.
Systemic administration of probiotics (milk enzymes) is also often necessary, to rebalance any intestinal flora disrupted by Candida albicans hyper-proliferation.
In addition to these medical treatments, the Proctologist almost always combines a control of the patient's diet, which is used as a true adjuvant therapy to the pharmacological one.
What diet should be had during the treatment of anal candidiasis?
Dietary therapy is very important during the treatment of candidiasis, as the Candida albicans fungus, in addition to residing physiologically in the gastric and intestinal mucosa, derives its source of sustenance from leavening sugars.
When the Candida albicans fungus increases its population in an uncontrolled manner, in the gut the natural microbiota living in our symbiosis (i.e., the friendly bacteria that complete our digestive process by forming stool) is affected, and weakened.
A weak microbiota causes a variety of alvus problems: from chronic diarrhea to stubborn constipation, which alter stools and thus worsen anorectal inflammation.
With that understood, the diet that the Proctologist usually prescribes for the candidiasis patient aims to avoid refined and pure sugars (such as white sugar), limit carbohydrate intake in general, and prefer fish, vegetables, eggs, white meat, and olive oil as dressing.
Proper dietary therapy supports and reinforces antifungal therapy, accelerating healing time and improving the patient's intestinal symptoms (which, often, are altered precisely by Candida infection).
Which physician should be consulted if anal candidiasis is suspected?
The Proctologist Surgeon is the referral health specialist in cases of suspected anal candidiasis.
In fact, it is that medical figure who is perfected in the study and treatment of all anorectal diseases, including Candida albicans hyperinfection.
In addition, advanced proctology practices, such as Dr. Luisella Troyer's, have state-of-the-art diagnostic equipment such as Electronic Endoscopic Videoproctoscopy, which are indispensable in assessing, without pain or preparation, the actual state of the anorectal mucosa and confirming or not the presence of anal candidiasis lesions.
Anal itching that won't go away? Maybe it's anal candidiasis, get help from Dr. troyer

If you experience symptomatology that makes you think you have anal candidiasis, such as intense itching that does not go away, you should not initiate self-prescribed therapies, but you should seek the advice of a Proctologist Physician experienced in the field.
If you are in Dubai, Dr. Luisella Troyer's clinic can help you diagnose anal candidiasis, including using modern Electronic Endoscopic Videoproctoscopy.
Dr. Troyer is a Proctologic Vascular Surgeon with decades of experience in proctology and anal candidiasis infections, and can therefore help you diagnose and treat Candida, with a personalized treatment plan that, in addition to medical care, also combines scrupulous dietary control.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- CANDIDA ALBICANS FUNGUS IS A SAPROPHYTIC PARASITE THAT NORMALLY LIVES IN OUR ORAL CAVITY, GASTRODIGESTIVE TRACT, ANAL AND GENITAL SKIN;
- UNDER NORMAL CONDITIONS, CANDIDA IS NOT DANGEROUS TO OUR HEALTH;
- CANDIDIASIS IS THE HYPER-PROLIFERATION OF THE CANDIDA FUNGUS DUE TO A MARKED LOWERING OF IMMUNE DEFENSES;
- THERE ARE MANY CAUSES THAT LEAD TO THE HYPER-PROLIFERATION OF THE CANDIDA FUNGUS: FROM AGGRESSIVE ANTIBIOTIC TREATMENT TO SITUATIONS OF CHRONIC IMMUNODEFICIENCY OR HORMONAL SURGES;
- IN WOMEN, UROGENITAL CANDIDIASIS IS VERY COMMON, ESPECIALLY IF THEY ARE ON CONTRACEPTIVE THERAPY;
- EVEN SEXUAL INTERCOURSE WITH AN ASYMPTOMATIC PARTNER WITH CANDIDIASIS CAN LEAD TO INFECTION;
- ANAL CANDIDIASIS IS WHEN THE LOCALIZATION OF HYPER-PROLIFERATION OF THE FUNGUS AFFLICTS THE ANORECTAL MUCOSA;
- SYMPTOMS OF ANAL CANDIDIASIS ARE OFTEN ITCHING, REDNESS OF THEANAL AREA AND ANAL MUCOSA, PRESENCE OF MALODOROUS WH ITISH LESIONSON THE ANUS AND PERIANAL AREA;
- ANAL CANDIDIASIS IS DIAGNOSED CLINICALLY,BY MEANS OF ELECTRONIC ENDOSCOPIC VIDEOPROCTOSCOPY EXAMINATION;
- THERAPY FOR CANDIDIASIS IS BASED ON THE PRESCRIPTION OF ANTIFUNGALS, PROBIOTICS, AND THE APPROPRIATE DIETARY DIET

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.