Have you suffered for years now from pathological hemorrhoids, which give you pain, burning and bleeding every time you have to go to the bathroom?
Would you like to cure them permanently but are scared of surgery, which you would like to avoid?
Modern Medicine has, for the past few years, developed a new treatment that is totally painless, quick and safe and can permanently resolve hemorrhoids without resorting to Surgery.
This is stabilized scleromousse: a completely noninvasive treatment, suitable for many hemorrhoidal stages, which can be performed without preparation and without any pain.
Read this page to find out what it is, and then schedule a proctology visit to see if you can do it.
Hemorrhoidal prolapse should not trigger embarrassment or shame, and therefore should not be delayed in diagnosisand treatment out of fear or shyness.
The sooner pathological hemorrhoids are diagnosed, the sooner action can be taken, with less discomfort and faster treatment, as well as a fair amount of financial savings (which never hurts).
What are hemorrhoids?
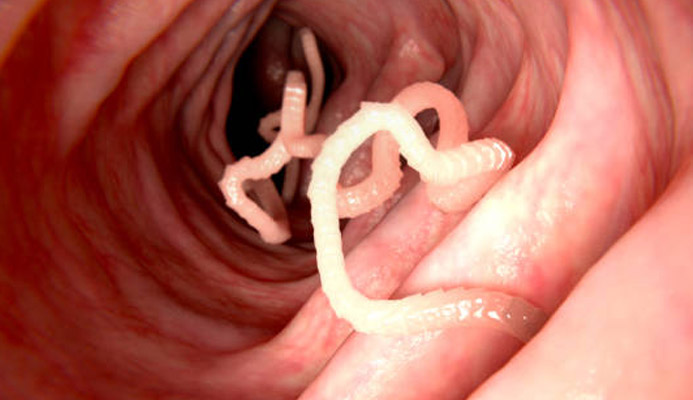
Hemorrhoids are athero-venous plexuses, basically resembling blood-laden pads, located within the anal canal.
To simplify, they are formations in which veins and arteries merge, and their main purpose is to sufficiently vascularize the anal canal and the anal orifice.
There are three main hemorrhoidal pads: right anterior, right posterior, and left lateral, to which are added two other secondary, smaller pads.
In normal situations, hemorrhoids do not cause any problems or discomfort, and their presence is not even felt, like that of any venous formation.
Given their peculiar position, however, in some cases, due to genetic predisposition or triggering factors, hemorrhoids extrude from their original position, bulging abnormally and descending into the anal canal, giving rise to what is called hemorrhoidal pathology (or hemorrhoidal disease).
Why do hemorrhoids bulge and prolapse?
There are many theories as to why hemorrhoidal disease begins, but so far Medicine has not established a universally valid cause.
At present, it is assumed that hemorrhoidal prolapse is mainly due to two causes:
- Genetic inheritance, which determines the quality of venous tissues (and their propensity or otherwise to fray);
- Hemodynamic pressure, which, combined with intra-abdominal pressure, causes continuous hemorrhoidal wall wear and tear
Associated with these two main causes may be a number of triggers, that is, conditions that, when encountered, can initiate hemorrhoidal pathology:
- Chronic constipation;
- Chronic diarrhea;
- The overweight;
- Pregnancy and childbirth;
- Natural aging;
- Smoking and alcohol abuse;
- Some sports or particular jobs
Obviously, multiple concurrences can come together, thus increasing the risk of hemorrhoidal prolapse starting or, if it has already happened, making it worse.
What are the symptoms of prolapsed hemorrhoids?

The symptomatology of pathological hemorrhoids is broad and varies greatly, especially in intensity from patient to patient, and is also related to the degree of prolapse severity.
That being said, there are symptoms that are very obvious, and common to roughly all stages:
Bleeding during defecation
Anal bleeding during defecation (hematochezia) is the most common symptom of pathological hemorrhoids.
It happens because stools, especially if they are particularly hard (typical of constipated bowel) tear the delicate hemorrhoidal wall bulging with blood, thus causing micro-abrasions, which in turn generate hematochezia.
Finding traces of bright red blood on the toilet paper, in the form of streaks on the stool itself or, in more prominent cases, in an even dripping form is a typical symptom of hemorrhoids.
In most non-serious cases, bleeding is minimal anyway, and does not cause health hazards.
In cases of severe prolapse that has never been treated, however, bleeding can also be profuse, even going so far as to bring anemia to the patient;
Burning and pain during defecation
Tearing of hemorrhoids as stool passes causes obvious bleeding and, like all wounds, also burning.
If the external hemorrhoids are prolapsed, this those can close to the anal orifice, the burning is often accompanied by pain as well.
Pain that becomes unbearable in case of hemorrhoid thrombization, that is, the formation of a thrombus (a blood clot) inside one of the external hemorrhoids;
Rectal tenesmus
Prolapsed hemorrhoids, especially if they are now very bulging, can give the sensation of incomplete emptying during defecation, with a symptom called tenesmus in medical jargon.
This particularly uncomfortable sensation can persist even after defecation, creating continuous abdominal tension;
Mucosal prolapse
By extruding outward, hemorrhoids drag part of the anorectal mucosa, thus also giving rise to prolapse of the same.
In mild cases, this prolapse is temporary, and resolves as the hemorrhoids recede, but in severe cases, of now completely prolapsed hemorrhoids, it can be permanent;
Dermatitis, proctitis and anitis
Extruded and bulging hemorrhoids are an unnatural situation, from which the anorectal mucosa attempts to protect itself by producing a large amount of mucus.
This overproduction of defense, however, causes a side effect called 'wet anus': the skin of the peri-anal area always remains moist with mucus and not well dried, soon coming to maceration and thus triggering anal area-specific dermatitis, called anitis.
Sometimes, this inflammation also extends into the rectum, resulting in proctitis.
Anitis and proctitis bring inflammation, burning, tingling and, almost always, anal itching;
Fecal incontinence
High-grade hemorrhoids, irreversibly prolapsed externally, worsen the natural hermetic closure of the anus at rest, causing it to close not completely and giving rise to a condition called, in Proctology, 'open anus'.
This partial opening of the anus at rest leads to leakage of fecal and gaseous material, thus giving rise to fecal incontinence.
It should be emphasized that all these symptoms are only a trace: they may not all occur (or all together), and they may also indicate pathological conditions other than hemorrhoids.
That is why the diagnosis of hemorrhoidal prolapse must mandatorily be confirmed by a Proctology Physician.
How are pathological hemorrhoids diagnosed?

Diagnosis of pathological hemorrhoids is relatively simple for an experienced Proctology Physician, but is often complicated by patient noncompliance.
In fact, often out of insulting and unsympathetic social qualms, shame, or fear of feeling pain, the patient delays a specialized proctological examination for years, thus making the situation worse and turning to the physician only when it is now severely compromised.
Diagnosis of hemorrhoids, on the other hand, is absolutely painless, requiring an equally painless proctological examination.
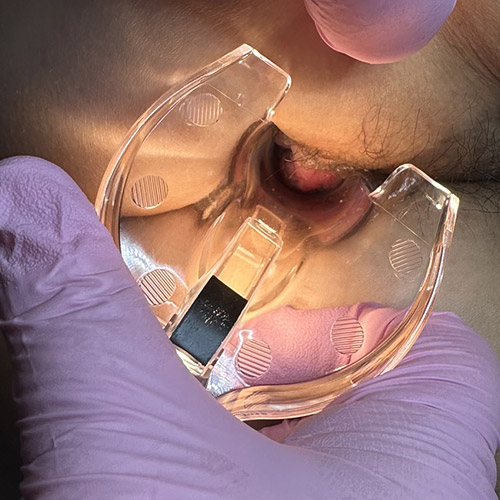
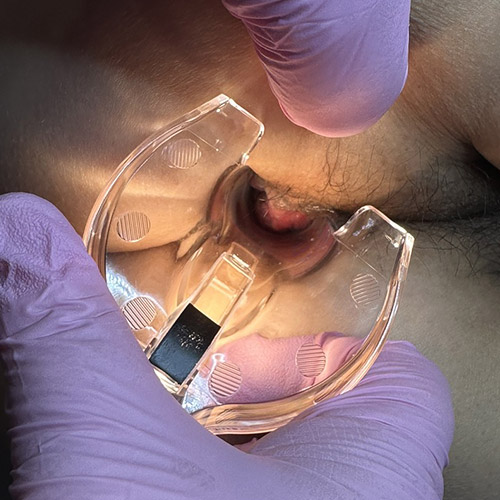
The proctology examination is divided into four distinct acts:
- The medical history, with the collection of the patient's entire medical history;
- Abdominal examination, with bowel palpation and assessment of peristalsis activity;
- Digital exploration of the anus, absolutely painless, in which the physician assesses the condition of the anal orifice and anal canal, looking for prolapses, lesions or polyps;
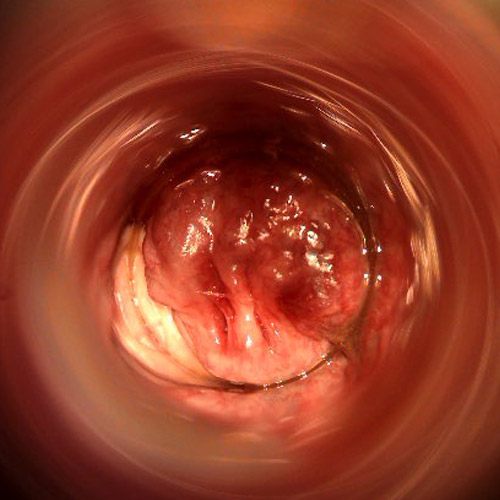
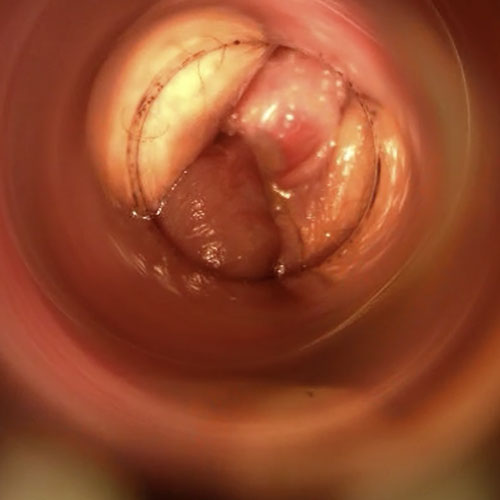
- Electronic Endoscopic Videoproscopy, a totally painless examination in which the physician, with the help of a high-resolution video camera, explores the entire anorectal canal, recording the examination on electronic media
These four unified medical acts make up the proctological examination for hemorrhoids, and are necessary and sufficient to establish the diagnosis with certainty.
Only in case of complications such as anal fistulas, anal abscesses, or other diagnostic suspicion on the upper part of the colon, the Proctologist may prescribe other specialized examinations, such as colonoscopy, endoanal ultrasound, and anorectal manometry.
Is there a severity scale for hemorrhoids?
Yes, a severity scale for hemorrhoidal prolapse was drawn up in the 1980s, which is mainly based on the descent and swelling of hemorrhoids.
The more they swell and descend the anal canal toward the orifice, the more severe the prolapse is judged to be.
At present, the classification thus has four degrees of severity:
Grade I hemorrhoids
The hemorrhoidal plexuses are only slightly extruded, and remain within the anal canal, with no obvious external symptoms.
They hardly bleed, they do not ache or burn, and so it is a situation that, presumably, many individuals have without even realizing it.
This grade of hemorrhoids can only be diagnosed by Electronic Endoscopic Videoproscopy examination;
Grade II hemorrhoids
Hemorrhoids only come out of the anal canal during defecation, or under sports (or work) exertion, but then re-enter immediately without manual repositioning.
The patient may experience anal bleeding and burning, due to the rubbing and tearing of feces on the delicate hemorrhoidal walls.
It is the degree of prolapse that, if caught early, can also be effectively resolved with proper diet and drug treatment;
Grade III hemorrhoids
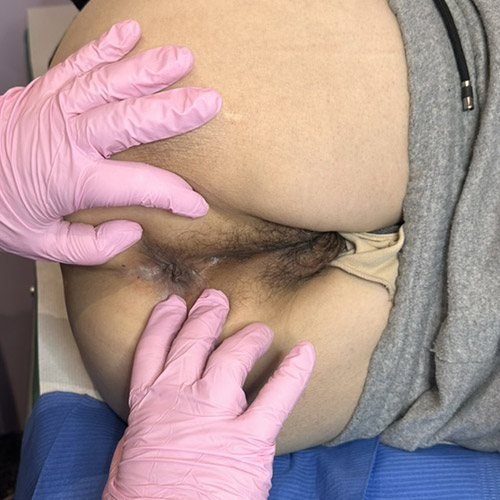
Hemorrhoidal prolapse is consistent and often abnormal, with plexuses extruding from the anal orifice after straining and defecation but not spontaneously re-entering.
They can go back in, however, if repositioned manually.
This hemorrhoidal stage also presents as symptoms anal bleeding, burning and, given that the prolapsed plexuses are already of considerable size, frequent episodes of anal tenesmus and itching;
Grade IV hemorrhoids
The hemorrhoidal prolapse is now abnormal, and is permanently extruded from the anal canal, not re-entering even with manual repositioning.
Bleeding even unrelated to evacuation is possible, and there is often a condition of a open anus, resulting in a wet anus and maceration of the peri-anal skin, leading to frequent anitis with anal itching.
Of course, these four degrees should not be seen as watertight compartments, well defined from each other under any conditions.
Pathological situations straddling one grade are always possible, with sometimes shared symptomatology.
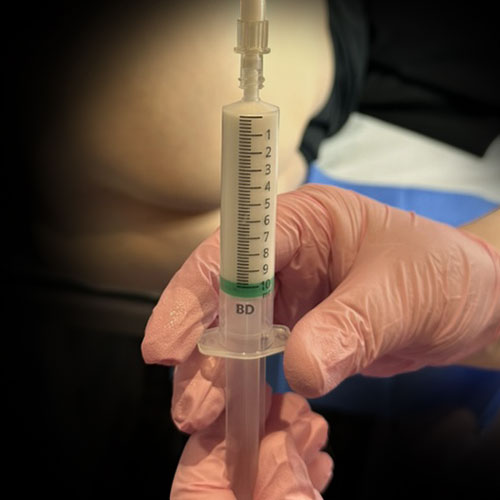
What is sterilized air-stabilized scleromousse?

Sterilized air-stabilized scleromousse is a medical-surgical treatment originally developed for the treatment of large venous varices, an alternative to actual surgery.
It is a mousse composed of polidocanol (a special type of alcohol) mixed with air previously sterilized using a special medical pump.
Usually, two parts polidocanol and six parts sterilized air are used to prepare the mousse, but these percentages may vary at the discretion of the Physician, and in relation to the patient's clinical status.
The chemical/physical premise is the same as in sclerosing therapy: polidocanol causes an irritation of the endothelium (the inner membrane of the veins), causing it to actually sclerose and thus cause it to shrink and close, effectively eliminating blood flow.
The vein thus closed becomes inert, and slowly reabsorbed by the tissues.
In scleromousse, the principle is the same, but polidocanol is mixed into a stable mousse that, unlike normal sclerosing fluid (unable to cling to veins of large lumen), is able to cling tenaciously to the endothelium of even large vessels, closing them off.
Sterilized air makes bacterial infections unlikely, thus preventing septic complications.
Today's sterilized air scleromousse, in contrast to early attempts in the past, is exceptionally stable: modern pumps can produce a nanobubble mousse that can remain tenacious for many minutes (even more than 20 minutes after preparation), thus providing excellent action on large vessels.
Because of this long-lasting stability, it was therefore possible to develop an exclusive treatment protocol for pathological hemorrhoids.
Hemorrhoids are essentially large vessels (veins and arteries joined together) in which blood stagnates when prolapsed.
Modern scleromousse is thus able to cling tightly to the inner walls of even large hemorrhoids, thereby causing them to sclerotize and shrink.
This approach guarantees, if well executed, similar results to surgical ones, but spares the patient the often uncomfortable operation of hemorrhoidectomy.
How long has scleromousse been used for hemorrhoid reduction?

The scleromousse protocol for hemorrhoid reduction has been developed on an experimental basis since 2018, which is when sterilizing pumps capable of producing a stable and suitable mousse for large hemorrhoid plexuses have been on the market.
Currently, after three years of trials and collected data, it has been concluded that the treatment is effective in more than 95% of treated cases, thus making it a serious alternative to surgery or minimally invasive therapies (often, relapsing and never resolving anyway).
Is scleromousse for hemorrhoids a definitive treatment?

Yes, sterilized air-stabilized scleromouse is a definitive treatment for the resolution of hemorrhoidal prolapse.
During the therapy, delivered in single sessions (about three, but the number may vary depending on the clinical case and the prescription of the Proctology Physician), polidocanol progressively sclerotizes the hemorrhoidal extrusion, effectively atrophying them and causing them to regress.
Along with the hemorrhoidal plexuses, mucosal tissue is also resorbed, so any mucosal prolapse is also treated.
Statistics and treatment trials tell us that the resolution rate of hemorrhoidal prolapse is more than 95%, making stabilized scleromousse comparable in results to surgery.
Is scleromousse for hemorrhoids painful?

No, the treatment is absolutely painless.
Polidocanol mousse injection is given beyond the combed line, that is, the line separating the anal and rectal canals, at a point where pain receptors are absent or at least very low in number.
This provides peace of mind to the patient, who experiences no pain except, at times, only a slight initial sting (however, totally bearable, and of very short duration).
Inoculation of the mousse into the hemorrhoidal gavage is absolutely painless, and is not felt by the patient in any way.
Polidocanol is a type of alcohol, which when in contact with the endothelium, i.e., the inner wall of veins, causes a curious effect: it causes the lumen to shrink, effectively closing it.
In Medicine, this effect is called sclerosis, and it is exploited by Vascular Surgery as a weapon to close, without resorting to scalpel or hooks, veins that have become diseased and incontinent.
The same principle is also used for hemorrhoidal plexuses (which have the same endothelium as veins), but exploiting an emulsion of polidocanol and air, prepared in mousse form.
Are there any pains or complications after scleromousse treatment for hemorrhoids?

Slight bleeding, however of very short duration, is normal immediately after treatment.
The therapy does not involve post-session pain, but slight swelling of the treated area, especially of the mousse-targeted gavage, is completely normal and physiological.
In the days following the session, the treated hemorrhoid may swell and change color, but this should not frighten the patient-it is normal and part of the healing process.
How long does the treated area take to heal completely?

Scleromousse for hemorrhoids is a treatment that is performed in sessions, usually three or more, delivered about 10 to 15 days apart.
The goal is to sclerotize and thus reduce hemorrhoids slowly, giving time for the tissues to heal spontaneously, without trauma.
Usually, the anal mucosa takes about 90 days to heal completely after injury or various surgical treatments.
So, full recovery is expected about three months after the last session.
However, this period of time should not frighten the patient: healing is painless, and the hemorrhoid situation improves with each passing day until complete resolution.
Can stage III or IV hemorrhoids also be treated with scleromousse?
Of course: sterilized air sclermousse treatment was indeed developed primarily for high-grade hemorrhoids, with the goal of avoiding surgical access for the patient.
Thus, scleromousse can be performed even on grade III or IV hemorrhoids, indeed: in many cases, these severe grades are the ones that respond best to treatment, yielding the best results.
Are all patients potentially indicated for scleromousse treatment of hemorrhoids?
Scleromousse treatment is designed to have the highest possible patient pool, with the goal of saving the cost (and discomfort) of classic hemorrhoidectomy surgery.
That being said, the indication for treatment is always decided by the physician after the appropriate proctological examination and videoscopic examination.
Do you suffer from prolapsed, bleeding and painful hemorrhoids in Dubai? Ask Dr. Luisella Troyer for help

Dr. Luisella Troyer is a Proctologic Vascular Surgeon who has specialized in the care and treatment of hemorrhoidal prolapses for many years.
After her long surgical experience, particularly with the Milligan-Morgan hemorrhoidectomy, Dr. was among the first Proctology Physicians to pioneer the new sterilized air-stabilized scleromousse.
A modern, innovative, effective and painless treatment that can bring immediate benefit without forcing the patient into Milligan-Morgan surgical access.
In her clinic in Dubai, Dr. Troyer can therefore help you diagnose your hemorrhoids accurately, thanks to the use of Electronic Endoscopic Videoproctoscopy, and establish the right course of treatment with the help of the new scleromousse.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- HEMORRHOIDS ARE ARTERIOVENOUS PLEXUSES, MUCH LIKE PADS, THAT ARE NORMALLY FOUND IN OUR ANAL CANAL;
- THE FUNCTION OF HEMORRHOIDS IS TO PROPERLY VASCULARIZE THE ENTIRE ANUS AND, SECONDARILY, TO HELP THE SPHINCTER MUSCLES IN FECAL CONTINENCE;
- IN NORMAL SITUATIONS, THE HEMORRHOID PLEXUSES DO NOT GIVE PROBLEMS OR DISCOMFORT;
- WITH AGE, WITH A CERTAIN GENETIC PREDISPOSITION, WITH PARTICULAR LIFESTYLES, JOBS, SPORTS, OR DUE TO PROCTOLOGIC DISEASES THAT INCREASE INTRA-ABDOMINAL PRESSURE, HEMORRHOIDS MAY EXTRUDE AND PROLAPSE FROM THEIR ORIGINAL POSITION;
- PROLAPSED AND BULGING HEMORRHOIDS ARE TERMED PATHOLOGICAL, AND GIVE RISE TO HEMORRHOIDAL PATHOLOGY;
- THERE ARE VARIOUS LEVELS OF SEVERITY OF HEMORRHOIDAL PROLAPSE, FROM STAGE ONETO STAGE FOUR;
- BULGING AND PROLAPSED HEMORRHOIDS TEND TO WORSEN OVER TIME, INCREASING DISCOMFORT FOR THE PATIENT;
- TYPICAL SYMPTOMS OF PROLAPSED HEMORRHOIDS ARE BLEEDINGDURINGEVACUATION, INTENSE BURNING, FOREIGN BODY SENSATION IN THE ANUS, AND, IN THE CASE OF THROMBIZATION, VERY SEVERE ANAL PAIN;
- IN THE LONG RUN, HEMORRHOID PATHOLOGY DEEPLY UNDERMINES THE PATIENT'S QUALITY OF LIFE;
- LOW-GRADE HEMORRHOIDS CAN RECEDE WITH THE RIGHT DIET AND DRUG THERAPY; HIGH-GRADE HEMORRHOIDS ALWAYS REQUIRE SPECIALIZED CARE;
- HEMORRHOIDECTOMY IS THE SURGICAL REMOVAL OF THE HEMORRHOID PLEXUSES, FOLLOWING A PROTOCOL KNOWN AS MILLIGAN-MORGAN;
- ALTERNATIVELY TO HEMORRHOIDECTOMY, A MODERN NONSURGICAL PROCOTOL CAN BE PRACTICED, BASED ON SCLEROTIZATION OF THE PROLAPSED PLEXUSES;
- SCLEROTHERAPY WITH SCLEROMOUSSE CAN SCLEROTIZE AND CLOSE THE HEMORRHOID PLEXUSES, WITHOUT PAIN AND WITHOUT THE USE OF SURGERY

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.