While doing your daily intimate hygiene, do you feel strange growths around your anus?
The presence of lesions of the peri-anal area should never be underestimated because, in addition to benign situations (such as small marisades or dermatofibromas), pre-cancerous infections, called anal warts, can still lurk.
Read this page written by Dr. Luisella Troyer, Proctologist Surgeon, to learn more about the peri-anal lesions that go by the name of condylomatosis.
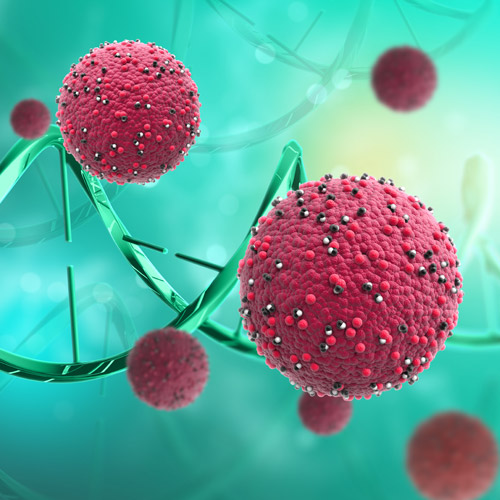
Having contracted HPV infection is not sufficient for the development of anal warts.
In fact, condylomatous growths form exclusively when the virus finds a far more than fertile replication environmentthat is not adequately limited by the natural action of the immune system.
This usually occurs in cases of immunodepression, either temporary or chronic.
A particularly heavy and lengthy antibiotic treatment , a period of severe stress, chemotherapy or radiation treatment, or chronic infection with another virus (e.g.,HIV) that has not been adequately treated.
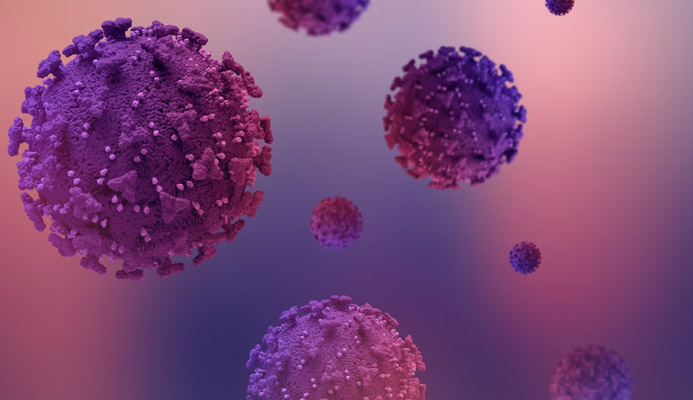
What is human papillomavirus infection?
Human Papillomavirus, also called by the English acronym HPV (Human Papilloma Virus) is a naked capsule virus, currently known in 16 groups and as many as 120 types.
It is a fairly infectious virus that is very easily spread by direct contact with infected skin, mucous membrane, or surfaces.
The viral load required for the virus to propagate is relatively low, making it particularly virulent.
HPV infection is extremely common in the adult population: the ease of direct infection and the low viral load required to initiate infestation make it widespread in virtually every part of the planet, in virtually every hygienic and social condition.
Since HPV is a dermatological virus, which infects precisely by 'piercing' the natural defenses of our skin or mucosa, the antigen falls under the broader list of Sexually Transmitted Diseases, as its proliferation is majority (but not exclusive) through the venereal route.
Although highly contagious, the HPV virus is largely harmless to our bodies: a healthy immune system can easily overpower the virus, eradicating it before it multiplies uncontrollably.
Only in a small percentage of cases, when the virus finds a weakened immune system (temporarily or chronically), the symptomatic manifestation of the infection occur, which are the common warts or, in the case of some very specific types of the virus, ano-genital condylomata.
What are anal warts?
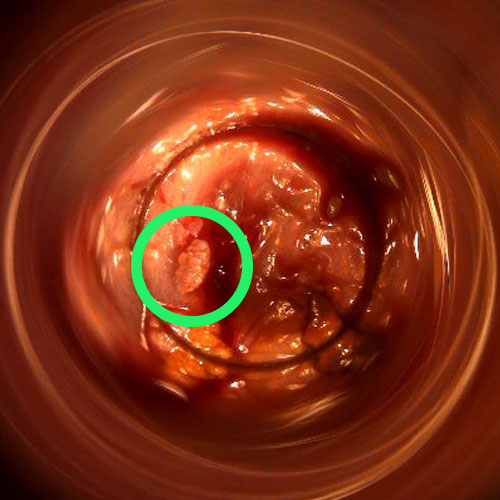
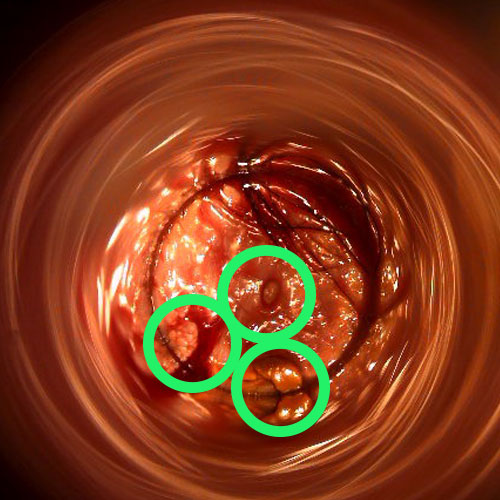
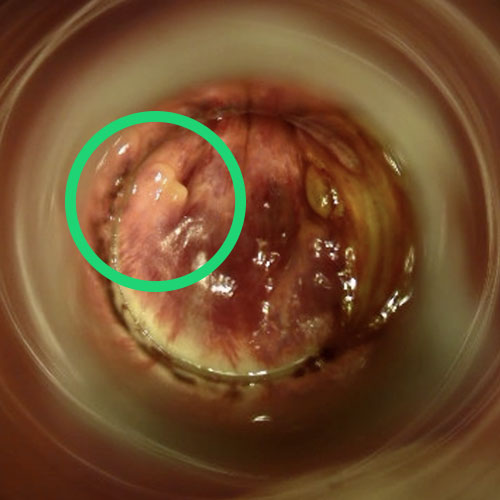
Anal condylomata, also called anal or ano-genital warts, are fleshy, flat or sharp growths, a visible symptom of HPV infection that the immune system has failed to control and confine.
They can occur anywhere on the ano-genital skin and also on the ano-rectal mucosa, and their shape and coloring can vary greatly, ranging from flat to sharp, and from pinkish to dark-brownish coloring.
In reality, these lesions are nothing more than the extreme response of our immune system, which, overwhelmed by the virus, attempts to isolate the threat by pushing it to the outside of the body, that is, to the skin, thus originating the lesions.
Given that these lesions are basically a large number of viruses 'confined' by the immune system in the form of superficial warts, their infectivity is extremely high.
Warts are considered oncologically to be pre-cancerous lesions: this is because in the long run the presence of the virus in infected skin cells can lead to malignant degeneration of the tissues, thus triggering carcinoma.
Some types of viruses are more likely than others to turn into cancerous lesions, and in fact typing of the infection is, usually, a histological test that is always suggested to the patient at diagnosis.
That is why, usually, removal of anal and genital warts is always suggested to the patient with condylomatosis (i.e., visible HPV infection).
What are the causes of anal warts?
The cause of the onset of condylomatous lesions is, as mentioned, an HPV infection that the immune system failed to contain and eradicate in time, before its uncontainable replication.
This usually occurs in cases of immunodeficiency, either temporary due to special situations (a high state of stress, particularly heavy antibiotic treatment, a concurrent debilitating viral or bacterial disease, chemotherapy, etc.), or due to chronic diseases that constantly impact the immune system (e.g., HIV infection not adequately treated).
Statistically speaking, the occurrence of warts is largely in the HIV-positive population: in fact, it is estimated that condylomatous symptomatology can be attributed, in the totality of known cases, in 60-80% to undiagnosed or untreated HIV-infected patients.
However, it should be specified that HPV is a typical opportunistic virus, which can affect even healthy individuals at any time, regardless of sex or age.
Anal warts are true pre-cancerous lesions, and should be considered and treated as such.
There is no guarantee that the lesions, in the future, will not develop into something more serious of a malignant nature, even if the viral strain that caused them is low risk.
That is why their removal is always recommended, and should never be put off for too long.
How common is the HPV virus in the human population?
HPV is very common in humans, and it does not make many distinctions of phenotype, sex, or age.
Statistically, WHO estimates that at least 75% of the entire human population comes into contact, at least once in their lifetime and during adulthood, with the virus.
However, most of these infections remain virtually ignored, as only a very small percentage then manifest visible symptoms, namely ano-genital condylomata.
Given that the Human Papilloma virus is spread through simple contact, one of the preferred routes of infection is precisely sexual intercourse, especially if unprotected.
The ano-genital mucosa, in fact, is particularly sensitive and delicate, and during intercourse (especially anal intercourse) it can easily micro-lacerate, thus becoming a preferential gateway for the virus.
Are there certain categories of people who are more predisposed to HPV infection?

Although the Human Papilloma virus can infect any part of the body, even not necessarily the ano-genital area, the sexual route is definitely the virus' preferred one, partly because of the large amount of organic material that, usually, partners exchange during the sexual act.
That being said, certain categories of people are therefore more prone to HPV infection.
These categories are:
- People without steady partners and with many promiscuous relationships, or sexually free couples with frequent promiscuous relationships;
- Homosexual people;
- People with HIV infection;
- People who are immunodepressed due to secondary causes (chemotherapy treatment, special emotional stress situations, trying antibiotic treatment, etc.);
- People who smoke
It should be remembered, however, that these categories of people, although statistically more prone to HPV infection, will not necessarily then manifest symptoms of condylomatosis.
As mentioned earlier, in order for the eruption of condylomatous lesions to occur, it is indeed necessary for the immune system to be overwhelmed by the virus, and for it therefore to replicate uncontrollably.
What are the symptoms of anal warts?

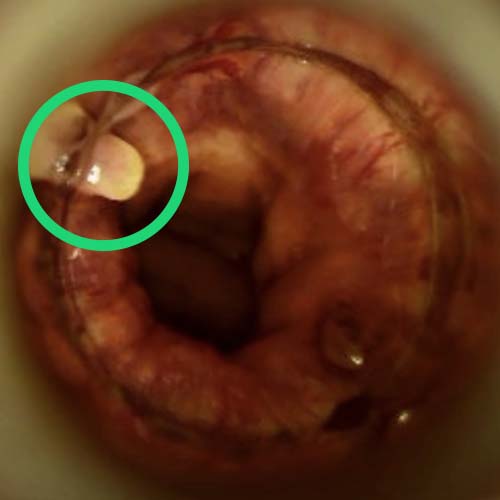
While HPV infection is, to a large extent, asymptomatic, condylomatous lesions, on the other hand, are well recognizable by the experienced Physician because they have distinctive features.
While their shape is always jagged, there are two types: flat or sharp.
Condylomata acuminata are also called 'cockscombs' because of their visual resemblance to the crest of the male chicken.
Their extent can vary: from a few millimeters to a few centimeters, as can their color, which can range from pinkish-white to dark-brownish.
Their presence is often asymptomatic, and they generally do not give any discomfort other than that of aesthetic unpleasantness.
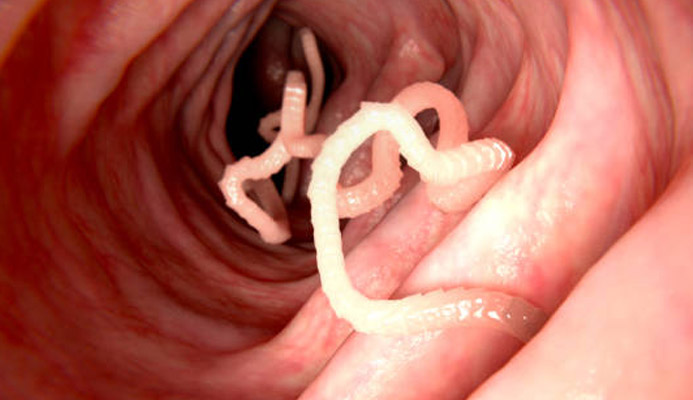
They can occur anywhere in the ano-genital area: on the genitals proper (including inside the vagina, or on the shaft of the penis), in the perineum area, in the peri-anal area (around the anus) or even inside the ano-rectal canal, reaching up to the end of the rectum (beyond that, in the upper intestine, they do not go).
Often the patient becomes aware of them only through tactile sensitivity: if the lesions are in fact external to the anal canal, around the peri-anal area, they can be felt during normal daily ablutions.
Warts internal to the anal canal, on the other hand, are neither noticeable nor visible, and are often diagnosed incidentally, following other proctologic investigations.
Only a very small proportion of condylomatous lesions give rise to inflammatory symptoms (anitis or proctitis), given by the excessive mucus production that the mucosa, in defense against the virus, can sometimes initiate.
This hyper-production of mucus, in some individuals, gives rise to the so-called 'wet anus', which leads to maceration of the peri-anal skin with the onset of dermatitis, specifically called anitis.
The possible recurrence of anal warts (always a likely event) should not, however, discourage the patient or make him or her desist from continuing treatments.
Relapses may occur but, in the long run, all therapies succeed in eradicating condylomata, also relying on the indispensable contribution of the immune system, the only and true cure for HPV infection.
Over time, the immune system always succeeds in defeating the virus, and therapies always succeed in eradicating condylomatous lesions once and for all, as long as the patient performshyperiodic checkups and the follow-up planned by the physician.
How are anal warts diagnosed?
Diagnosis of anal condylomata is clinical, and is relatively simple for an experienced Proctologist Physician.
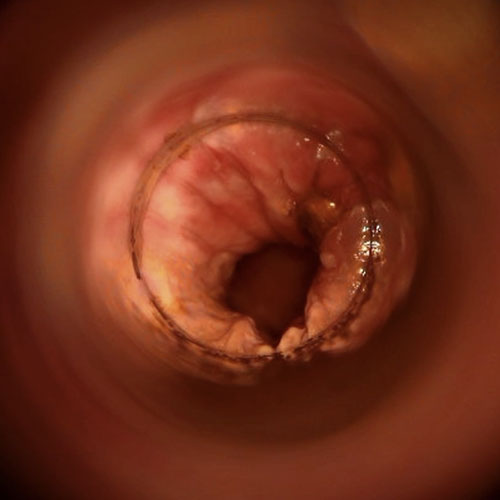
External lesions are easily framed during the proctologic examination, while any internal ones are visualized with a noninvasive video-based examination called Electronic Endoscopic Videoproctoscopy.
A whole colonoscopy for internal investigation of the anorectal canal is often proposed by unskilled Physicians, but such an examination should be avoided for this condition because condylomatosis does not develop beyond the junction of the rectum with the sigma.
This length (about 12-13cm) is easily reached by the Videoproctoscopy examination, thus sparing the patient the tedious preparation for colonoscopy.
What is the treatment for anal warts?

Although no HPV-specific antiviral treatment is yet available, a large number of treatments for the removal of anal condylomata are available instead.
Removal of condylomatous lesions is always suggested to the patient, since these pre-tumor neoformations, in addition to being an oncological risk (generally low anyway, statistically speaking), are also a danger to the patient himself, since there is always a risk of self-inoculation, from the diseased part to other healthy parts of the body.
This self-inoculation can occur at any time, and thus condyloma removal also (and especially) aims to lower the viral load of the infection.
Treatments for anal warts can be essentially of two types: medical or surgical.
Among medical treatments, the topical use of podophylline (an anti-cancer agent) is usually prescribed as a quick and low-cost application.
For external warts only, a very effective and low-cost treatment is the use of liquid nitrogen cryotherapy, which also has the advantage of leaving no obvious scarring.
The use of an electrosurgical scalpel or plasma lance is also a very effective treatment for removing condylomata in the peri-anal area, without significantly impacting the aesthetics of the area.
For warts inside the anal canal, surgical access is usually the preferred access.
This is performed according to various techniques, at the Surgeon's discretion: with the cold blade (i.e., scalpel excision), or by combining it with cautery using an electrosurgical scalpel.
Whichever technique is chosen, it is the Surgeon's job to provide for the total removal of all visible lesions, while at the same time respecting healthy mucosal tissues.
Is it true that anal warts can recur?
Yes, it is true.
Recurrences after lesion excision, even if it has been performed with excellent techniques, are extremely frequent.
This, for a simple reason: the Surgeon provides removal of diseased tissue visible to the eye (even with special magnifiers), but cannot notice individual infected cells.
It therefore takes only a short time for the virus, especially if the host is still immunocompromised, to relapse, starting the infestation again.
It should be noted, however, that although recurrences are frequent, in the long run, medical and surgical treatments always get the better of the infection, thanks in part to possible immune-stimulating therapies (which, often, are offered to the patient during eradication therapy).
No matter how long, therefore, the battle against anal condylomata should not be considered a waste of time or a factor of disturbance and emotional stress: in the long run, it always brings eradication to a conclusion, provided, of course, that the patient is punctual and diligent with the mandatory follow-ups and checks.
Who to contact if you suspect you have anal condylomatosis?

The qualified Physician for diagnosis and treatment against anal warts is the Proctologist Surgeon, that is, the health care specialist with great experience in the study and treatment of all diseases of the anorectal canal, including warts.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- HUMAN PAPILLOMA VIRUS(HPV) IS AN OPPORTUNISTIC DERMATOLOGICAL VIRUS, TRANSMISSIBLE BY DIRECT CONTACT OF INFECTED SURFACES;
- IN A HEALTHY, NONSMOKING ADULT SUBJECT, HPV REMAINS ASYMPTOMATIC, EFFECTIVELY CONTROLLED AND ERADICATED BY THE IMMUNE SYSTEM;
- ONLY WHEN THE IMMUNE SYSTEM IS WEAKENED CAN THE HPV VIRUS REPLICATE UNCHECKED, GIVING RISE TO CONDYLOMATOSIS;
- CONDYLOMATA ARE FLESHY GROWTH-LIKE LESIONS THAT CAN AFFECT ANY PART OF THE SKIN AND MUCOSA, ANAL, RECTAL, AND EVEN ORAL;
- CONDYLOMATOUS LESIONS ARE VERY INFECTIOUS, AS THERE IS A LOT OF VIRAL LOAD WITHIN THEM;
- MEDICALLY, CONDYLOMA LESIONS ARE CLASSIFIED AS PRE-CANCEROUS LESIONS;
- WHEN THEY AFFECT THE PERI-ANAL AREA AND ANAL CANAL, CONDYLOMATA ARE CALLED ANAL CONDYLOMATA;
- ANAL CONDYLOMAS DEVELOP PREDOMINANTLY IN IMMUNOCOMPROMISED INDIVIDUALS, EITHER TEMPORARILY OR CHRONICALLY;
- NO CURE IS YET AVAILABLE FOR HPV INFECTION, BUT SPECIFIC TREATMENTS FOR ANAL CONDYLOMAS ARE AVAILABLE;
- ANAL CONDYLOMAS CAN DEGENERATE, ALBEIT RARELY, INTO NEOPLASMSOF THE ANUS AND RECTUM;
- FOR SAFETY REASONS, REMOVAL OF ANAL CONDYLOMAS IS ALWAYS PROPOSED TO THE PATIENT

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.