Do you notice strange growths around the anus that look like little papillae?
Do you have itching, redness, burning in the anal area, or do you produce an excessive amount of mucus, which also soils your underwear?
There is a viral infection that can afflict any part of the body's skin, including the delicate anal and peri-anal area, called condylomatosis.
Read this page to find out what anal condylomas are, what they originate from, how they occur, and what you can do to get rid of them.
Simple infection with the HPV virus does not mean the automatic development of anal or genital condylomata.
To form, condylomatous lesions need a great deal of viral activity, which is not effectively counteracted by the immune system.
This occurs only in cases of immunodepression, temporary or chronic, of the immune defenses.
In a healthy, nonsmoking, non-immunodepressed individual, the human papilloma virus is contained and, over time, eliminated, thus not giving rise to symptomatology.
What are anal WARTS?
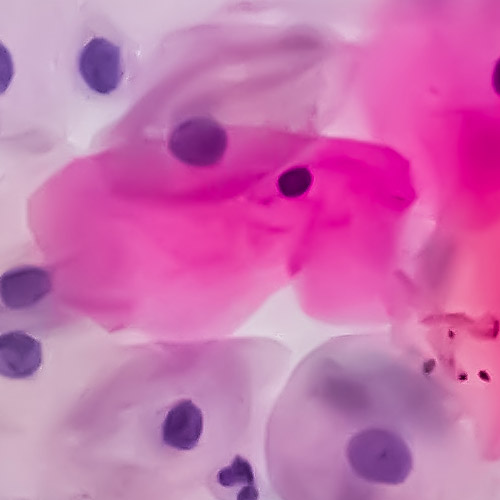
Anal warts, or anal condylomata, are fleshy, flat or acuminate growths caused by the immune response to a viral infection of the Human Papilloma Virus (HPV).
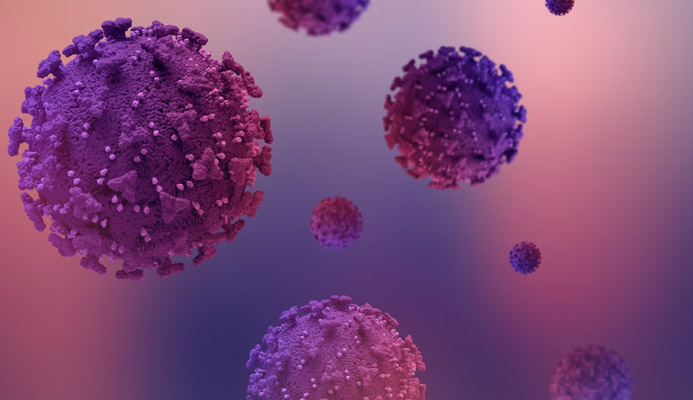
Human Papilloma virus is a naked virus, without a pericapsis, capable of infecting any part of the skin surface, including the anorectal mucosa.
This virus, known in 16 groups and as many as 120 different types, is a classic opportunistic virus: in fact, it prefers to attack the immune system when the latter is particularly weak, such as after heavy antibiotic treatment, a mild period of stress, or in conjunction with another infection, bacterial or viral.
Condylomas are a desperate response by our immune system, which, overwhelmed by the HPV virus, tries to contain it by 'pushing' it out of the body, thus into the epidermis.
This act generates the condylomatous lesions, which are nothing more than true ano-genital warts (and so, in fact, they are alternately called).
What is HPV virus, and why is it often asymptomatic?
Human Papillomavirus is an extremely common and widespread virus among the world's population, as its transmission occurs by simple direct contact.
Such contact may be with another infected person, or with a surface that has not been well washed or disinfected and has a high viral load.
Because of this characteristic, the HPV virus is perfect for transmission during sexual intercourse, effectively making it join the long list of sexually transmitted diseases.
The World Health Organization estimates that the vast majority of the adult human population, about 75%, at some point in their lives have contracted or will contract HPV infection, and this gives an idea of the numbers of infections each year.
In a healthy, nonsmoking individual who is regularly fed a varied diet, the HPV virus does not generate any symptoms, as it is usually confronted and defeated by the immune system before it can replicate uncontrollably.
Virus symptoms, i.e., condylomatous lesions, appear exclusively when the host is immunocompromised, either temporarily or chronically.
When designing the right therapy for anal condylomas, it is important to respect the patient's anorectal tissues, avoiding unnecessary scarring or postoperative pain.
Injuries of the anal canal, but not only
Warts caused by uncontrolled replication of the HPV virus can affect not only the anus and anal canal, but also the rectum, perianal area, genitals, and, in a more extensive form, any other mucous membrane in the body.
Also the oral cavity, throat, or lips, although in the latter cases the occurrence of warts in those areas is mainly confined to long-term immunocompromised patients, such as HIV-infected individuals not adequately treated with appropriate anti-viral therapy.
Clinically, there is no difference between anal or genital condylomatous lesions, or even of the oral mucosa: they are always caused by the Human Papilloma virus, their shape and coloration may change slightly but they are always an extreme response of the host immune system.
Are condylomata pre-cancerous lesions?
Yes, condylomata are considered pre-cancerous lesions, and for this reason their treatment is always recommended.
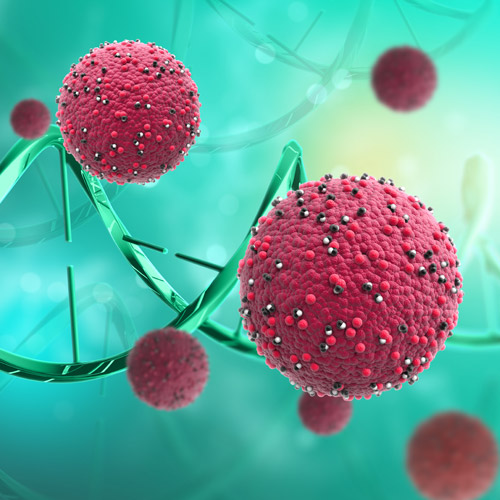
In fact, although in a small number of cases and almost always only for certain types of PHV (strains 16 and 18 especially), condylomata can degenerate into a malignant form, thus giving rise to cancerous lesions.
This is because, in the long run, the PHV virus can cause mutation in the DNA of epithelial cells, thus originating the cancer pathology, for example, with cancer of the anus or rectum.
However, it should be remembered and well emphasized that the transformation of anal condylomata into rectal and anus cancers is a statistically rare event, although still possible.
What are anal warts caused by?
Anal condylomata are essentially the latest weapon of the immune system, which, debilitated (temporarily or chronically), attempts to contain the Human Papilloma virus, confining it as much as possible to outside of the body.
Thus, the real cause of warts is not so much the HPV virus itself (actually, in most cases harmless), but its hyper-proliferation caused by a decided lowering of immune defenses.
For these reasons, the most symptomatic individuals are immunocompromised patients, for example, HIV-infected individuals who have not been properly treated with anti-viral therapy, or individuals who are recovering from a course of radiation or chemotherapy, or who otherwise, for whatever reason, have (even temporarily) lowered immune defenses.
The HPV virus is an opportunistic virus, and this bears repeating: in a healthy individual it is effectively contained and defeated by our natural defenses, and thus needs to find a flaw in our immune system to proliferate and propagate.
Obviously, it is not being homosexual per se that increases the risk of condyloma eruption, but the anal penetrative activitythatsuch sexual preference often entails.
In fact, the anal mucosa, being devoid of epidermis, is particularly sensitive and delicate, and more exposed to attack by microorganisms, such as the HPV virus.
This risk worsens with sexual activity at the anal level, since during penetration, even if well lubricated, micro-trauma and micro-injuries are still created, which, although insignificant from a clinical point of view, are real chasms for viruses, which can thus better penetrate the body.
Using a condom during intercourse mitigates the risk but does not reduce it entirely.
Are there individuals in greater danger of contracting warts?
HPV is transmitted by direct contact, predominantly (but not exclusively) through sexual contact.
This means that PHV infection is an STD, and thus follows the general rules of any other Sexually Transmitted Disease.
Thus, the most exposed individuals are all sexually active and particularly promiscuous adults without a steady partner and monogamous sexual relationship.
Again, given that any anal intercourse (even if well lubricated) always generates micro-injuries to the anal canal, homosexual individuals are particularly at risk of acquiring HPV infection.
Individuals with chronic debilitating pathological conditions, such as tuberculosis or HIV-positive patients not adequately treated by anti-viral therapy are 70% to 80% more likely than a healthy individual to become infected with the HPV virus and then develop condylomata.
Even the use of condoms during intercourse, although it helps to reduce viral load, never protects 100% from possible human papillomavirus infection.
Sexual activity aside, PHV, as mentioned just above, is a virus that is transmitted by physical contact, either direct skin-to-skin or mucosa-to-mucosa or with infected, not well disinfected surfaces.
Like any virus, its ideal proliferation site outside the host is a warm and humid environment, and therefore it is possible to contract Papillomavirus even in environments such as swimming pools, saunas, and gyms.
Self-contagiousness, that is, contagion of a healthy part of the same patient's body from an infected part instead, cannot be ruled out.
For example, some cases of anal condylomatosis is the result of self-contagiousness: the individual, by shaving his genital private parts or touching himself during daily ablutions, may transfer the virus to the anal and perianal area, giving rise to anal condylomata.
How are anal warts diagnosed?

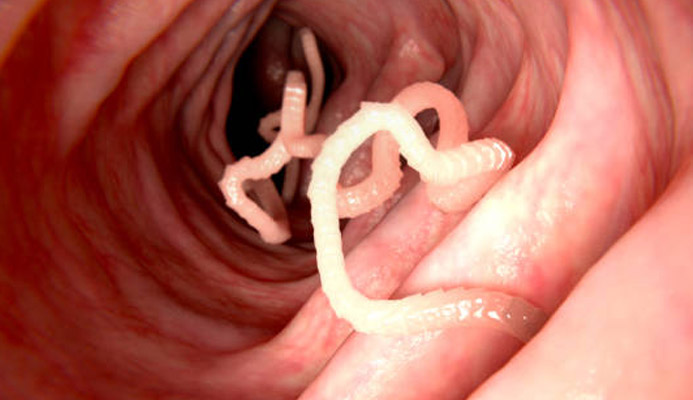
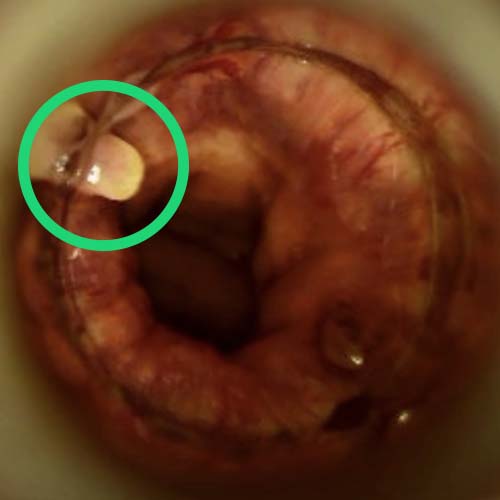
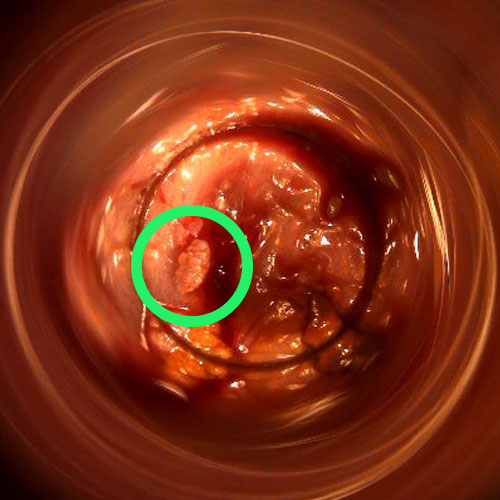
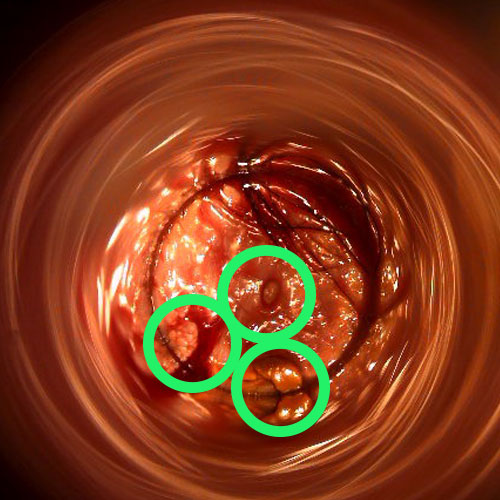
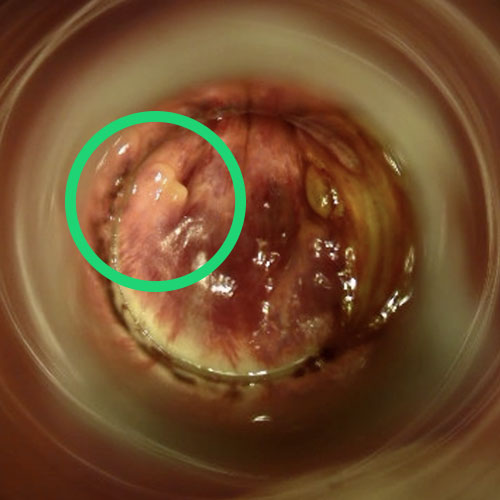
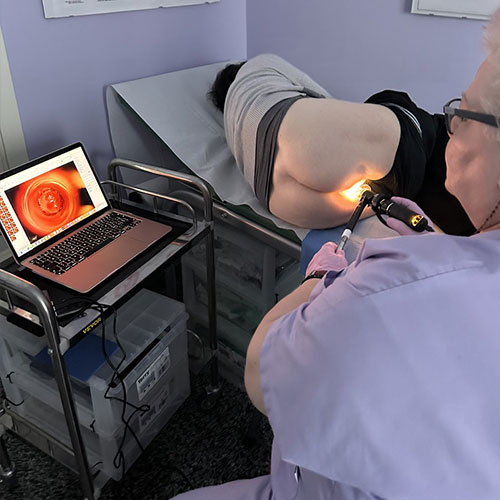
Diagnosis of anal condylomata is fairly easy for an experienced Physician, requiring a proctological examination with related proctoscopy.
Warts external to the anal canal and peri-anal warts can be diagnosed clinically, while any internal ones, which can expand all the way into the rectal canal, necessarily require proctoscopy.
Particularly useful for the correct identification of condylomata and their mapping is the Electronic Endoscopic Videoproscopy examination: an advanced examination that allows the Proctology Physician the precise identification of each lesion, perfectly magnified on a monitor and recorded on a digital medium, which can be consulted at any time.
What are the symptoms of anal warts?

Warts appear as jagged lesions of varying size, with an irregular edge and varying coloring: from whitish to pinkish, even reaching brown.
These formations can appear flat or sharp, giving rise to the typical 'cockscomb' shape.
They generally give no other symptoms, and if they are present inside the anal canal they are often not even perceived by the subject, who is therefore an unaware carrier of Papillomavirus.
Only in some cases do these lesions bother, and they generate dermatitis, increased mucus production, and subsequent anitis (more or less severe), which in turn causes itching and anal burning for the patient.
This rather rare symptomatology is dependent on the immune system itself, which, in order to protect the mucosa from the virus, produces more mucus than normal, causing the wet anus phenomenon, which gives rise to dermatitis.
Anal condylomata can affect any part of the perianal area, anus, anal canal, and rectal canal, but they do not expand beyond the rectum.
Of course, it bears repeating, the occurrence of warts is only possible when the HPV virus finds good play at uncontrolled hyper-replication, due to a temporarily or chronically depressed immune system.
Vaccination against HPV should be done beforethe onset of sexual activity, thus roughly before adolescence.
Any vaccination in adulthood when one has already contracted the virus is statistically less effective (although always recommended).
How do you treat anal warts?

In the current state of Medicine, there is still no specific treatment available for HPV infection, but several treatments are available for condyloma removal.
Removal of anal condylomata is always recommended, for three main reasons:
- Warts are highly infectious lesions: their viral load is high, and therefore they can expand viral infection to other areas of the body;
- The longer the lesion remains, the greater the statistical risk of it degenerating into a cancerous form;
- There is no certainty that the lesion will recede on its own, and this is regardless of the immune system's 'victory' over the HPV virus
Currently, treatments for condyloma removal are both medical and surgical: the use of either method depends on various factors, decided by the Proctology Physician during the specialist visit.
Medical therapies fight the virus on two fronts: they stimulate natural immune defenses on the one hand (immune-stimulating therapies), while attempted to destroy condyloma cells through anti-cancer drugs.
The first-line weapon for warts, given its low cost and easy availability, is podophyllin: an anti-cancer agent with a now well-proven efficacy that can be used with topical ointment directly on lesions.
If condyloma placement allows, liquid nitrogen cryotherapy, which can burn off infected cells and leave no obvious scarring, can also be used.
Where medical therapies fail, or there is a different clinical indication, a more radical approach is used instead, through Surgery.
Condyloma eradication surgery must meet three main characteristics:
- Must ensure total remediation of the infected area;
- It should prevent the patient from unnecessary postoperative pain;
- Must respect the patient's healthy tissues
Eradication by surgery can be done in any way: by high-powered operative laser, by electrocoagulation, or by cold blade, depending on the preference and judgment of the Proctologist Surgeon.
Can anal warts recur?

Yes, condylomata can recur.
Like any other HPV lesion (even common warts), condylomata can recur, thus giving rise to a recurrence of symptoms.
Recurrence of warts is a fairly common adverse event, and it is unrelated to the skill of the Surgeon or Proctology Physician during lesion eradication (either by pharmacological or surgical method).
Recurrence occurs because, during eradication, some infected cells (invisible to the Physician) can remain, and thus infected the surrounding healthy tissue, giving rise to new lesions.
This happens quite often: recurrences of warts range from 30% to more than 60%, precisely because the high viral load of the virus allows it, with little tissue, to easily affect other healthy mucosa.
However, this should not discourage the patient or make him or her desist from the therapies agreed upon with the Physician: in the long run, with perseverance, the HPV virus is always eradicated from the body, and thus the infection is defeated.
However, this may require time, various therapies (or mix of therapies) and particular and precise medical follow-up.
Of this, the patient must be properly informed.
Human Papilloma virus is very infectious, but it lives very little outside the host: about 20 minutes, under optimal conditions (right temperature and right humidity), exclusively 'attached' to cell fragments.
In fact, the virus is not able to survive outside the cell, but indirect contagion can always occurconfragments of epithelium, mucus or mucosa, left on objects or places of frequentation.
That's why, to avoid nonsexual contagion, such as in public places like swimming pools or gyms, just follow these simple precautions:
- Never exchange your towel or bathrobe with others;
- Avoid walking barefoot in showers and locker rooms;
- Never use the same towel you used to dry your feet to also dry your genitals and anus;
- Always wash your hands thoroughly before touching or washing your genitals and anus;
- Avoid leaning on the toilet when you need to defecate or urinate;
- Do not sit without underwear or a towel on benches, chairs, armchairs, etc. in locker rooms, saunas or showers
Who is the Physician who can diagnose and treat anal warts?
The specialist physician with great experience in anal condylomatosis is the Proctology Physician.
The Proctologist is the medical professional who studies and treats all diseases of the anus and rectum, that is, the last parts of the intestines.
Therefore, the Proctologist is able to accurately diagnose anal warts, both external and internal, using proctoscopy examination.
Currently, state-of-the-art proctology physicians use, rather than the traditional optical proctoscope, the new Electronic Videoproctoscope.
Given that, the Proctologist is often required to intervene surgically to remove warts, it is not uncommon for them to come from purely surgical specialty schools, such as General Surgery or Vascular Surgery.
Do you suffer from warts in Dubai, or think you may be affected? Ask Dr. Luisella Troyer for help

Dr. Luisella Troyer is a Proctologic Vascular Surgeon with extensive clinical experience in the diagnosis and treatment of anal warts.
In her clinic in Dubai, Dr. Troyer can accurately diagnose all lesions of the rectum and anus, making use of the already modern and sophisticated electromedical investigation machines, such as the Electronic Videoproctoscope.
A noninvasive, totally digital examination, that can map with extreme precision any condylomata present in the anus and rectum, thus helping the Dr. Troyer to propose to the patient the best possible therapy to eradicate them.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- ANAL CONDYLOMATA ARE THE OUTCOME OF HUMAN PAPILLOMA VIRUS (HPV) INFECTION THAT IS NOT WELL CONTROLLED BY THE IMMUNE SYSTEM;
- HPV IS A DERMATOLOGICAL VIRUS, WHICH IS SPREAD THROUGH DIRECT CONTACT, ESPECIALLY THROUGH SEXUAL CONTACT;
- CONDYLOMATOSIS FALLS UNDERSEXUALLY TRANSMITTED DISEASES;
- ANAL CONDYLOMATA PRESENT AS WARTS, FLAT OR SHARP, THAT CAN OCCUR ANYWHERE ON THE PERI-ANAL SKIN OR WITHIN THE ANORECTAL MUCOSA;
- ANAL CONDYLOMATA ARE LESIONS CONSIDERED PRE-CANCEROUS;
- SOME TYPES OF HPV VIRUSES ARE MORE LIKELY TO TRANSFORM INFECTED CELLS INTO TUMORS, WHILE OTHERS ARE AT LOW CANCER RISK;
- NO SPECIFIC CURE FOR HPV IS CURRENTLY AVAILABLE, BUT MANY TREATMENTS ARE AVAILABLE TO ERADICATE CONDYLOMATA;
- REMOVAL OF CONDYLOMAS IS ALWAYS RECOMMENDED BECAUSE THE LESIONS ARE HIGHLY INFECTIOUS AND, IN THE LONG TERM, THE DANGER OF MUTATION INTOCANCEROUS OUTCOMES IS NONZERO;
- CERTAIN CATEGORIES OF PEOPLE, SUCH AS IMMUNOCOMPROMISED INDIVIDUALS AND HOMOSEXUALS, ARE MORE PRONE TO HPV INFECTION AND THE DEVELOPMENT OF CONDYLOMAS;
- BOTHMEDICAL AND SURGICAL TREATMENTS ARE AVAILABLE TO SAFELY REMOVE CONDYLOMAS;
- RECURRENCE OF CONDYLOMAS IS A COMMON OCCURRENCE, BUT STILL SHOULD NOT DISCOURAGE THE PATIENT;
- PREVENTION FROM HPV VIRUS CAN BE DONE QUICKLY AND PAINLESSLY BY VACCINATION

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.