Are you a woman and have frequent vaginal pain that prevents you from having sexual intercourse?
Can you not evacuate completely, and often stool 'gets stuck' in the rectum and sometimes you have to facilitate its exit manually?
Rectocele is one of the most disabling conditions for a woman, and it is also a disease that is still guiltily underestimated, often even by Doctors, about which there is still so much misinformation.
Read this page to find out what rectocele is: what it originates from, how it is diagnosed, and how it can be treated.
Pain during the penetrative sexual act and obstructed defecation are the main symptoms of a high-grade rectocele, which has become problematic.
Often, such a condition puts a woman in awe and embarrassment who, for reasons of shame, avoids seeking the Physician's attention.
This is the wrong attitude, as well as counterproductive: in fact, the first step in resolving or alleviating the symptoms of rectocele is precisely to proceed to a specialized proctological examination.
What is rectocele?

In Medicine, rectocele refers to the herniation (sliding) of the rectum into the vaginal cavity.
Due to obvious anatomical limitations, this condition affects only women and, not infrequently, is also associated with other pelvic floor prolapses, such as cystocele (bladder prolapse) and prolapse of the uterus.
Although often little or not at all known, rectocele is a condition (not necessarily symptomatic) that is estimated to involve most postpartum, i.e., already giving birth, women over the age of 50.
What was the cause of the rectocele?
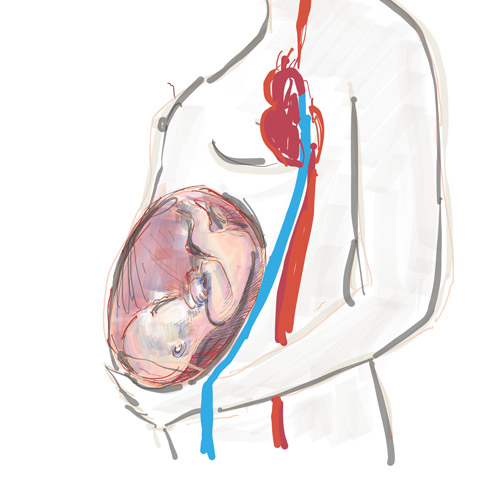
Rectocele, or rather the herniation that causes it, is dependent on the failure or exhaustion of the muscular and ligamentous tissues of the recto-vaginal part, that is, that anatomical structure that physically separates, in women, the rectum from the vagina.
This structural failure is, in large part, caused by an abnormal increase in intra-abdominal pressure, which in turn is generated by a variety of triggers, such as:
- The labor and the delivery;
- Chronic constipation never treated;
- Some strenuous work or sports;
- Obesity
In addition to these known factors, given that recto-vaginal wall unraveling always has purely mechanical origins, any state or stress that worsens the pressure to the pelvises is, potentially, triggering rectocele.
Rectocele tends to occur with greater incidence in older women because, due to natural physiological aging and slowing of metabolism, pelvic floor tissues in them are naturally less loaded with collagen, and therefore less adherent to supporting structures.
What are the symptoms of rectocele?
Rectocele is a chronic and, tendentially, degenerative condition: prolapse of the recto-vaginal wall and its herniation do not recede without the right therapies; in the best cases, they stabilize (by how much, one cannot predict).
Thus, the symptomatology of rectocele is directly proportional to its stage of severity.
At present, three stages of rectocele have been defined, divided into ascending order:
Grade I rectocele (mild rectocele)
Herniation of the rectum into the vagina is mild, and symptomatology is almost always absent, at least in young women;
Grade II rectocele (moderate rectocele)
Herniation of the rectum into the vagina is substantial, often reaching the vaginal opening.
Pain during sexual acts, difficulty expelling stool, and difficulty during urination appear;
Grade III rectocele (severe rectocele)
The rectum has completely invaded the vagina, and the recto-vaginal wall is totally collapsed and, often, torn.
Sexual intercourse becomes almost impossible, fecal and urinary incontinence appears, 'foreign body' sensation in the vagina, heaviness and pain in the pelvises, both anus and vagina.
Is rectocele common in women?
Yes, definitely.
It is estimated that the majority of postpartum women, that is, women who have already given birth, develop at least a grade I rectocele.
The exact estimation of the percentage of women with rectocele is complicated, since mild stages, which are considered physiological in the woman giving birth, do not give any symptoms, and therefore are not perceived by the patient, who in turn does not report them to the Physician.
How is a rectocele diagnosed?
The diagnosis of rectocele is performed by the physician (either Proctologist or Gynecologist) by pelvic and proctological examination.
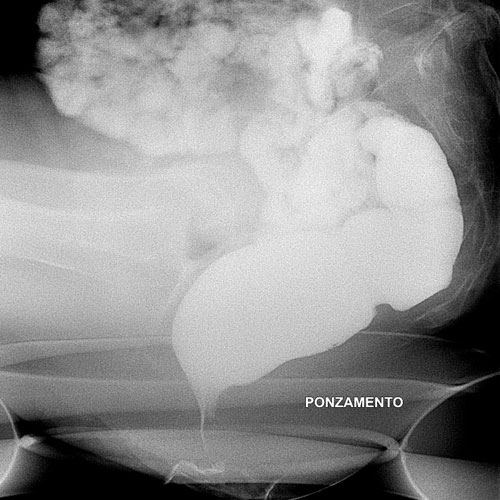
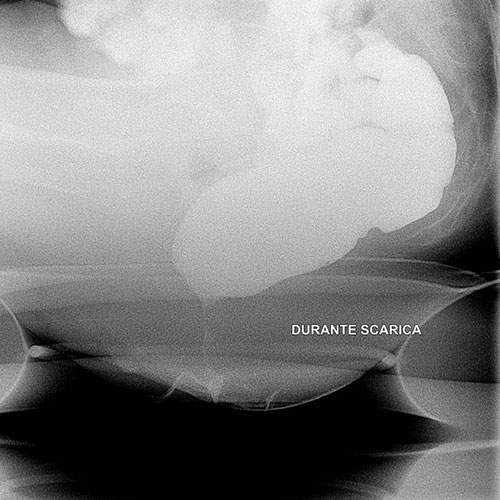
Digital inspection of the anus and vagina is accompanied by various supportive examinations, including proctoscopy, anorectal manometry (useful for establishing sphincter muscle tone), vaginal or transanal ultrasound, and defecography.
These examinations are useful to the Physician not so much to assess the presence of rectocele (the experienced Physician is, usually, satisfied with proctological inspection to establish it), but rather to ascertain the severity of it and the state of the supporting structures of the recto-vaginal wall.
This information is essential for the physician to the prescribe the right therapy, whether rehabilitative or surgical.
What is the treatment for rectocele?
Rectocele requires medical and rehabilitative intervention exclusively when it is symptomatic, that is, when it presents disabling symptoms for the patient.
Mild rectoceles are considered physiological, and therefore almost always not even perceived by the woman, who often does not even know of their pathological existence.
Only symptomatic rectocele should be treated, with pelvic floor rehabilitation and, in very severe cases, surgical access.
That being said, it is imperative to emphasize that, as moreover in other cases of prolapse of human anatomies, prevention is the best cure for rectocele.
This means that a woman, especially during her young and fertile life, should avoid abdominal hyper-pressure, or at least avoid situations in which it is possible, or certain, to occur.
In this sense, the greatest danger to a fertile woman is from pregnancy and natural delivery.
During the labor and the delivery, the recto-vaginal wall undergoes abnormal pressures, often deforming it irreparably (although, fortunately, in most cases slightly).
This harm is greater the longer and more complicated the labor, and therefore the patient should be properly followed by an OB/GYN throughout the pregnancy, possibly planning (if the physician deems it appropriate) a cesarean delivery.
More strenuous sports with excessive loads should also be limited, such as weightlifting, horseback riding and body building in general.
Constipated women should be properly cared for, as situations of chronic constipation always lead to excessive exhaustion of the pelvic floor, including the recto-vaginal wall.
These preventive rules are considered the 'gold standard' for rectocele and, if well implemented, although they cannot completely eliminate its occurrence, they can still limit its degree of severity.
However, when the rectocele is now symptomatic, there is no alternative to rehabilitation and, in some cases, surgery.
What is rehabilitation therapy for rectocele?
Rehabilitation therapy for rectocele is required when prolapse of the rectum into the vagina has become symptomatic, that is, causing pain and discomfort for the patient.
It is based on a series of specific pelvic exercises (the Kegel exercises), combined with electrostimulation and biofeedback.
This is a conservative therapy aimed not at resolving the rectocele, but at decreasing intraabdominal pressure and re-tuning the supporting muscles and structures of the pelvic floor.
Rehabilitation therapy for rectocele is performed with flexible protocols usually tailored to the patient's need, usually involving an initial tranche of intensive sessions, followed by another maintenance session that is more spread out over time.
Although it cannot cure rectocele herniation upstream, rehabilitation therapy, if well performed, can significantly reduce the symptoms of rectocele, sometimes eliminating them altogether.
When is surgical treatment for rectocele performed?
Surgery for rectocele is reserved only for severe cases where rehabilitation does not provide detectable and concrete benefits.
Surgery is usually resorted to when there is a total prolapse of the recto-vaginal wall, with laceration of the same and, as a result, with the constant presence of stool in the vagina.
The most common procedure to surgically repair this damage is colporrhaphy, which often also involves the insertion of a biocompatible mesh to reinforce the reconstructed wall.
Where significant descent of the perineum is also present, the Surgeon may also opt for simultaneous perineorrhaphy, which involves the shortening of the prolapsed perineum itself.
When should one seek medical attention in case one suspects rectocele?

In general, it is advisable for women, especially those who are puerperous and over 50, to see a Proctologist (or alternately, a Gynecologist) when they begin to experience problems with:
- Fecal or urinary incontinence;
- Pain during the act of penetration;
- Presence of fecal debris in the vagina;
- Difficulty evacuating regularly, with mandatory recourse to manual removal of feces from the rectum;
- Sensation of 'foreign body' in the vagina;
- Anal or vaginal bleeding after defecation
These symptoms, even if shared with other conditions, should alert the woman and prompt her to have a specialist, proctological or gynecological examination as soon as possible.
Which physician should be consulted if a rectocele is suspected?

The Physician who specializes in rectocele and all disorders of the rectum and anus is the Proctologist Physician.
The Proctologist Physician, who is usually also a Surgeon, has all the necessary skills to diagnose and treat rectocele, with both rehabilitative and surgical therapy.
In fact, not infrequently, the Proctologist Physician has in his team nurses, physical therapists, massage therapists, and technical personnel capable of delivering advanced rehabilitative therapies, both with physical exercises and with the use of electro-medical devices.
Alternatively, the Gynecologic Physician is also a qualified professional to diagnose and treat rectocele, as this pathology, playfully, necessarily affects the patient's gynecological anatomical parts as well.
Do you think you are suffering from rectocele in Dubai? Rely on Dr. Luisella Troyer's 30 years of experience.

Dr. Luisella Troyer is a Proctologist Vascular Surgeon, who assists and receives patients with rectocele and pelvic floor prolapse problems every day at her clinic in Dubai.
The modernly organized practice has state-of-the-art electro-medical equipment for pelvic floor rehabilitation, as well as an excellent team of nurses, massage therapists, physical therapists and health technicians who can give high-quality support for women in need of pelvic rehabilitation against rectocele.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- RECTOCELE IS THE HERNIATION OF THE RECTUM INTO THE VAGINA;
- IT IS ESTIMATED THAT VIRTUALLY ALL PURPURE WOMEN OVER 50 YEARS OF AGE HAVE AGRADE 1 RECTOCELE, WHICH IS ALMOST ALWAYS ASYMPTOMATIC;
- FOR PREGNANCY AND CHILDBIRTH, A MILD RECTOCELE IS CONSIDERED PHYSIOLOGIC IN WOMEN, AND USUALLY DOES NOT REQUIRE MEDICAL TREATMENT;
- ONLY SYMPTOMATIC RECTOCELE REQUIRES REHABILITATIVE AND MEDICAL TREATMENTS;
- RECTOCELE, IF SYMPTOMATIC, CAN GIVE SEVERAL DISABLING SYMPTOMS FOR THE WOMAN: FROM INABILITY TO EVACUATE PROPERLY TO INABILITY TO HAVE PENETRATIVE INTERCOURSE;
- MEDIUM GRADE RECTOCELES CAN BE WELL CONTAINED WITH PROPER PELVIC FLOOR REHABILITATION, THROUGH PHYSIOTHERAPY AND ELECTROSTIMULATION;
- SEVERE RECTOCELES, IN WHICH THERE IS ALSO LACERATION OF THE RECTO-VAGINAL WALL, USUALLY REQUIRE PHYSIOTHERAPY AND CORRECTIVE SURGERY

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.

















