
Has blood come out of your anus, either spontaneously or during evacuation, and are you terrified of the symptom?
Have you noticed bright red blood stains on stool, undergarments, or toilet paper?
First of all, don't freak out: statistically, most anal bleeding episodes are due to benign causes.
Bleeding from the anus can put genuine terror in the patient, but the situation can and should still be managed, calmly and reasonably.
Read this informational page written by Dr. Luisella Troyer, Proctologist Surgeon, and then book a specialized proctologic examination, which is the only sensible act that can put your mind at ease and give an accurate answer to why the anal bleeding is occurring.
Le emorroidi patologiche, cioè il prolasso e l'estrusione dei plessi emorroidari, sono tra le prime due patologie in tutto il mondo (assieme alla carie dentale).
Questo può dare subito l'idea dell'estensione del fenomeno, che non conosce confini geografici per davvero, e di quante persone, ogni giorno, soffrano di episodi di sanguinamento anale.
A livello statistico, le emorroidi prolassate e lesionate dal passaggio delle feci sono la causa primaria di tutti gli episodi di sanguinamento anale.
What is rectoragia, and how does it differ from hematochezia?

In Medicine, rectorrhagia is defined as copious bleeding from the rectum, coming out of the anal orifice and sometimes taking on the contours of a true hemorrhage.
It differs from hematochezia, i.e., anal bleeding, in the intensity of the flow, which in hematochezia is much more restrained, sometimes manifesting only in sporadic spots or streaks of blood on stool or toilet paper.
The two terms are often confused with each other and, often, even health care professionals mix them up without much distinction, but in fact rectorrhagia is really copious bleeding, while hematochezia is extremely more restrained.
Regardless of the amount and intensity of blood coming out of the anus, however, it should be noted that both rectorrhagia and hematochezia have one common origin: a lesion of the anorectal canal or even the intestines.
What was the reason for the anal bleeding?

Bleeding from the anus, whether it is just 'spotting' or 'streaking' or a copious drip, is always given by a lesion (wound) of the anorectal canal or the colon, that is, the large intestine.
The origin of this lesion in the intestinal mucosa varies, and there are many diseases or at any rate pathological conditions that can cause the intestine or rectum to tear, and thus bleed.
The color of the blood coming out of the anus can help give an initial guess as to where, in fact, the lesion developed.
In fact, bright-red bleeding generally indicates lesions distal to the anal orifice, thus located at a point in the bowel not too far from the opening of the anus.
Usually, this spot is located in the rectum or right in the anal canal, and this is why the blood comes out 'bright red', not yet clotted.
Conversely, dark blood, or hematochezia presenting as small pieces of dark, clotted blood in the stool may be significant of a proximal lesion of the colon, located at the beginning of the intestine.
The 'blackness' of blood is thus given by digestion as it passes through the intestinal mucosa by bacteria.
Having clarified this, regardless of the color of bleeding, the intestinal mucosa can bleed from a long list of causes, for example:
- For anal fissure, then a lesion with slow or totally absent healing of the anal canal;
- For a 'fresh', i.e., not yet ulcerated, wound of the rectal or anal canal, due, for example, to the transit of stool that is too hard;
- For intense proctitis, which is inflammation of the anorectal canal;
- For diverticulitis, which is inflammation, infection, or ulceration of the diverticula in the colon;
- For an anal fistula;
- For a hemorrhoidal prolapse with tearing of the plexuses;
- For anal or rectal warts;
- For the presence of one or more rectal or intestinal polyps;
- For Crohn's disease, or ulcerative rectocolitis;
- For gastroenteritis;
- For severe irritation given by the infestation of Candida albicans fungus;
- For ischemic colitis;
- For salmonellosis intoxication;
- For a solitary ulcer of the rectum
- For the presence of carcinoma of the rectum, anus, or colon
The latter case, fortunately, is the rarest statistically, and most anal bleeding is due to benign conditions, such as severe proctitis, prolapsed hemorrhoids, or anal injury.
How is rectoragia or hematochezia diagnosed?

The clinical symptom of anal bleeding is characteristic, leaves no doubt of interpretation, and is obviously already detected by the patient, who often becomes excessively frightened and, not infrequently, runs to the emergency room.
However, hematochezia or rectoragia are only symptoms, the cause of which must be investigated with the mandatory proctologic specialist examination.
Good medical practice involves a scrupulous anamnesis, with the collection of the patient's clinical history, which often already directs the physician toward the diagnostic hypothesis.
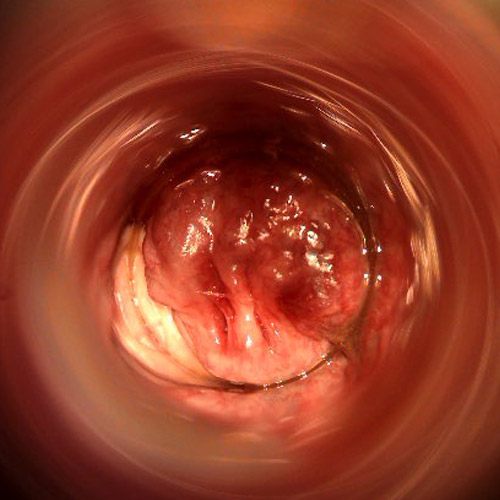
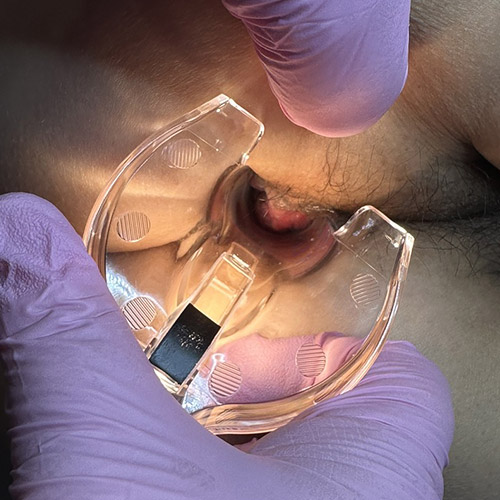
After the medical history, the proctological examination includes abdominal examination, digital inspection, and the obligatory Electronic Endoscopic Videoproscopy.
This technique allows the entire anorectal canal, from the ampulla to the anal orifice, to be visualized in high definition by means of a camera.
In the case of positivity of the examination, thus in the case of finding lesions in the rectum or anus, originating from the bleeding, the patient is directed to the right treatment, medical or surgical.
If the examination is negative, medical protocol involves deeper inspection of the entire colon by video colonoscopy.
If it, too, yields a negative result, the physician may prescribe the further examination of gastroscopy, with possible pelvic and abdominal CT scans.
In the case that the patient's age is over 50 years, it may be useful to always evaluate, regardless of whether the videoproctoscopy examination is positive or not, the whole bowel by videocolonoscopy as well.
What is the treatment for anal bleeding?
Obviously, the treatment of anal bleeding is the treatment of the intestinal injury that is generating it.
Statistically, most episodes of hematochezia and rectorrhagia are due to hemorrhoidal disease, that is, inflammation, congestion, swelling, and tearing of the hemorrhoidal plexuses extruded out of their original anatomical position in the anal canal.
Another percentage of bleeding causes, smaller but still not negligible, is also due to the presence of wounds, either fresh or ulcerated (fissures), of the anal canal.
Also not to be minimized is the rate of bleeding from intense proctitis, i.e., inflammation of the anorectal canal, often due to never resolved bowel problems (constipation or chronic diarrhea).
Typical autoimmune diseases of the colon, such as ulcerative rectocolitis and Crohn's disease, also cause intense episodes of rectorrhagia.
Diverticulitis, i.e., inflammation and tearing of diverticula, can lead to episodes of anal bleeding, which often result in intense rectoragia, always requiring urgent hospitalization.
Fortunately, only a small percentage of anal bleeding episodes are due to anorectal or colon cancer.
Treatment therefore can vary greatly depending on the cause of the bleeding, and can be arranged by the Proctologist only after the exact diagnosis has been made.
Why do hemorrhoids bleed?
Hemorrhoids are three small, pad-shaped vascular plexuses formed by veins and arteries joined together seamlessly.
They are placed in the anal canal just before the orifice, and have the function of vascularizing the entire area of the anus, while aiding the sphincters in stool containment.
Due to a long series of triggers, almost always related to problems of intra-abdominal hyper-pressure and alvus disorders (chronic constipation, for example), hemorrhoids can swell, become inflamed, and thus extrude from their original position, thus initiating what is called hemorrhoidal pathology.
Swelling with blood and extruding from the anal canal, hemorrhoids can easily tear as stool passes that is too hard, typical of constipation, or too acidic, typical instead of the condition of diarrhea.
Tearing, being filled with blood, the hemorrhoids begin to stain clothing, toilet paper, and stool, sometimes dripping, sometimes leaving spots of semi-coagulated blood, and sometimes instead giving rise to full-blown rectorrhagia that lasts, albeit spotty, for many days.
Although not as frequently, this rectoragia, in cases of patients with major hemorrhoidal prolapses, can even give anemia, and require emergency transfusion treatment.
Hematochezia due to hemorrhoids is, statistically, the most common cause of all anal bleeding.
What to do if you experience blood coming out of the anus?
If you notice bloodstains on toilet paper, underwear, or even red streaks on stool, first it is a good idea to remain calm and not be frightened.
Most of these bleeding episodes are due to benign diseases of the anorectal canal, thus hemorrhoids or small internal mucosal tears.
What needs to be done, in addition to not freaking out, is to book a specialized proctological examination with a Proctology Physician right away.
Specialist proctological examination the only really sensible thing to do, as well as the only medical act that can give an accurate answer about the origin of the anal bleeding.
Unless you are experiencing unstoppable rectorrhagia, with large and continuous bleeding that you just cannot stop, you should not clog up the already congested emergency rooms for an anal bleeding episode.
Are you bleeding from your anus, and are you worried? Ask Dr. Luisella Troyer for help

Dr. Luisella Troyer is a Proctologist Surgeon specializing in Vascular Surgery, and perfected for many years in Proctology.
At his clinic in Dubai, Dr. Troyer can give you immediate support for your anal bleeding, also helping you to understand its origin with the use of advanced Electronic Endoscopic Videoproscopy.
A diagnostic tool of excellence, which allows the entire anorectal canal to be viewed, without preparation or pain, to discover the origin of the lesion that is causing the hematochezia.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- UNDER NORMAL CONDITIONS, NO BLOOD SHOULD COME OUT DURING DEFECATION, AND NO DISCOMFORT OR BURNING SHOULD BE EXPERIENCED;
- WHEN ONE EXPERIENCES AN EPISODE OF ANAL BLEEDING IT IS ALWAYS BECAUSE OF AN INJURY SOMEWHERE IN THE BOWEL;
- ONE SPEAKS OF HEMATOCHEZIA WHEN THE BLEEDING IS MODEST, WHILE ONE SPEAKS OF RECTORRHAGIA WHEN THE ANAL BLEEDING IS CONSTANT;
- SEVERE EPISODES OF RECTORRHAGIA CAN LEAD TO ANEMIA, AND SUBSEQUENT LIFE-THREATENING;
- BRIGHT RED BLOOD FROM THE ANUS INDICATES A LESION CLOSE TO THE ORIFICE; DARK BLOOD, ON THE OTHER HAND, SUGGESTS A LESION FAR FROM IT, AT THE BEGINNING OF THE COLON;
- MOST ANAL BLEEDING EPISODES ARE DUE NOT TO MALIGNANT DISEASE BUT TO HEMORRHOIDAL DISEASE;
- ANAL FISSURE, ANORECTAL CONDYLOMATA, INTENSE PROCTITIS, DIVERTICULITIS, AND A SOLITARY ULCER OF THE RECTUM CAN ALSO LEAD TO ANAL BLEEDING;
- TO TREAT ANAL BLEEDING, IT IS NECESSARY TO TREAT THE LESION THAT ORIGINATES IT;
- PROCTOLOGICAL EXAMINATION IS NECESSARY TO HYPOTHESIZE ANY DIAGNOSIS OF ANAL BLEEDING

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.

















