Do you suffer from pathological hemorrhoids, and do you notice that the symptoms worsen during the summer or at any rate the hot season?
Summer and hot weather are difficult times for those suffering from hemorrhoidal disease, which often results in genuine hemorrhoidal crises, which are very painful and therefore feared by patients.
There is a definite correlation between increased temperature and worsening of pathological hemorrhoids: read this page to find out what this connection is, and what you can do to improve the situation and make the symptoms less painful.
Drinking the right amount of water every day is an unavoidable task for each of us, and it is a good healthy practice independent of age and season of the year.
However, in summer,due to our body's increased sweating, we are all obliged to replenish fluids more by drinking more.
There is no upper limit to the amount of water we can drink: water intoxication is a phenomenon that is almost impossible for a human being, as it would happen after dozens of liters ingested in a very short time.
Drinking a lot in hot weather is essential to keepthe stool softand hydrated, preventing it from becoming too hard, which could increase intra-abdominal pressure and thus inflame and tear the hemorrhoids, worsening the symptomatic condition.
WHAT ARE HEMORRHOIDS?
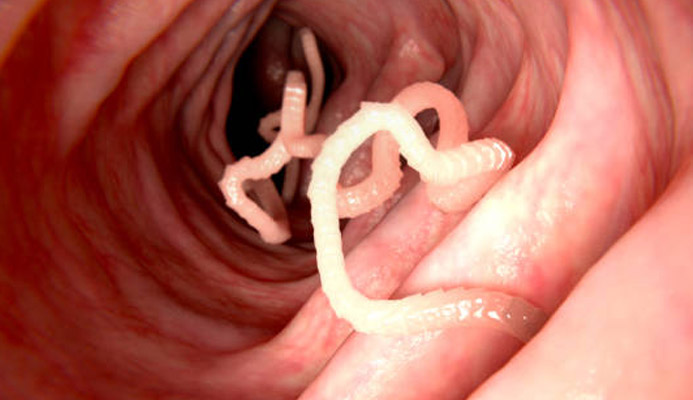
Hemorrhoids are physiological plexuses formed by veins and arteries joined together (anastomosed, in medical jargon), present anatomically in the anal canal.
They resemble soft, blood-laden pads, and each has three main plexuses: right anterior, right posterior, and left lateral.
These pads, under normal conditions, have the useful function of vascularizing the anal canal and, secondarily, of aiding the sphincters in restraining feces.
Only under certain conditions, that is, when the hemorrhoids become excessively swollen with blood, become inflamed, tear and extrude out of their original location, can we speak of 'hemorrhoidal disease,' or 'pathological hemorrhoids.
Drinking the right amount of water every day is an indispensable task for each of us, and is a good healthy practice independent of age and season of the year.
However, in summer, due to our body's increased sweating, we are all obliged to replenish fluids more by drinking more.
There is no upper limit to the amount of water we can drink: water intoxication is a phenomenon that is almost impossible for a human being, as it would happen after dozens of liters ingested in a very short time.
Drinking a lot in hot weather is essential to keep the stool soft and hydrated, preventing it from forming too hard, which could increase intra-abdominal pressure and thus inflame and tear the hemorrhoids, worsening the symptomatic condition.
WHAT IS HEMORRHOIDAL DISEASE?

Hemorrhoidal disease or pathological hemorrhoids refers to a pathological alteration of the normal hemorrhoidal plexuses, which becomeenlarged,inflamed, lacerated, and extruded out of their anatomical location in the anal canal, resulting in hemorrhoidal prolapse.
Hemorrhoidal disease is extremely common throughout the world: it is even thought to be, along with dental caries, the number one disease in humans, which should give a pretty good idea of how many people it affects and afflicts each year.
The main cause of hemorrhoid prolapse is not yet well known to science, but over time two main theories have been proposed :
- The mechanical theory, which sees a natural exhaustion of the supporting tissues of hemorrhoids due to advancing age, slowing collagen production, and triggers such as chronic constipation;
- The hemodynamic theory, which sees the onset of prolapse given by blood hyper-pressure on the plexuses, in turn due to intra-abdominal hyper-pressure
It should be noted that these two theories are not necessarily at odds with eachother, and that both can equally lead to hemorrhoidal prolapse.
In addition to these two theories that attempt to explain the origin of hemorrhoidal disease, over the years Medicine has ascertained the correlation between the onset of pathological hemorrhoids and the presence of certain triggers, such as:
- Chronic constipation;
- Aging and the natural loss of collagen;
- Chronic diarrhea and alvus problems given by the irritable colon;
- Pregnancy and childbirth;
- A diet low in fiber and proper daily hydration;
- A diet too rich in spicy and/or irritating foods for the intestinal mucosa;
- Some sports or strenuous work;
- Certain chronic diseases of the intestines, such as Crohn's disease or ulcerative rectocolitis.
All of these factors result in a degradation of the tightness of the supporting tissues to which the plexuses 'anchor' to the anal canal, as well as the exhaustion of the tissues of the hemorrhoids themselves, which become exhausted and initiate bulging and prolapse.
WHAT ARE THE SYMPTOMS OF PATHOLOGICAL HEMORRHOIDS?
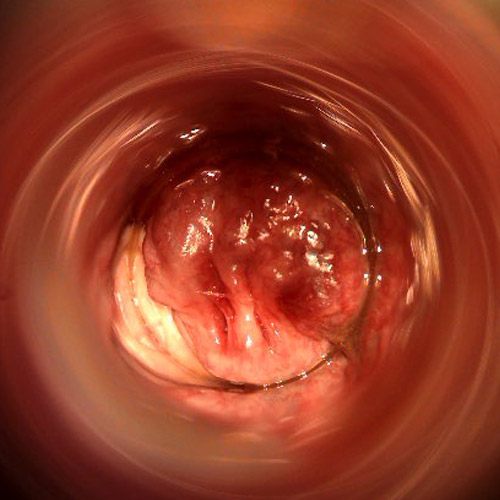
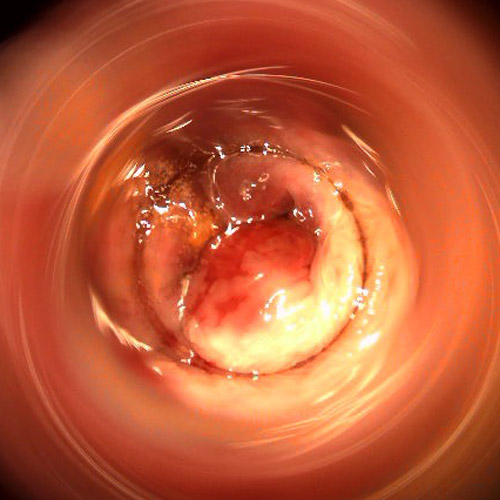
The typical symptoms of pathological hemorrhoids are prolapse of the plexuses, which tend to bulge out of the anal orifice, as well as anal bleeding (hematochezia), often coinciding with the act of defecation, due to the rubbing of feces on the prolapsed and inflamed hemorrhoids.
To these typical symptoms may be added other common related symptoms such as sensation of tenesmus, burning, and anal itching, and, as a complication of greater discomfort, a hemorrhoidal thrombus.
The clinical manifestation of all these symptoms varies both in relation to the extent of the prolapse, any palliative therapies the patient implements, and, last but not least, also the external temperature.
In fact, it is precisely the increase in temperature that causes a well-known physiological phenomenon underlying the increase in hemorrhoidal symptoms, which drives many patients to seek immediate treatment for prolapsed hemorrhoids in the hot season each year.
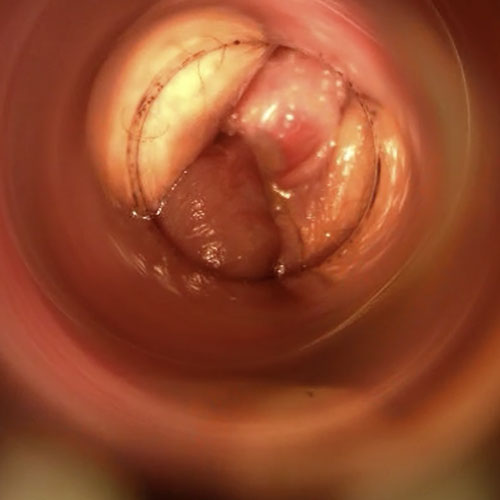
Treatment for hemorrhoids varies greatly according to their stage, as well as their inflammation and congestion.
Low-stage hemorrhoids can be effectively treated and resolved with the right diet, prescription of flavonoid supplements and local emollients, which can decongest the plexuses and, especially in young patients, help the body to regenerate the supporting tissues damaged by prolapse.
High prolapses, on the other hand, almost always require more vigorous, radical, hence destructive, therapy.
In recent times, hemorrhoidectomy according to Milligan-Morgansta being scaled back by the use of modern stabilized scleromousse, which can sclerose (close) the hemorrhoid plexuses permanently, without pain and without surgical access.
Therapy for hemorrhoids variesgreatly according to their stage as well as their inflammation and congestion.
Low-stage hemorrhoids can be effectively treated and resolved with the right diet, prescription of flavonoid supplements, and local emollients, which can decongest the plexuses and, especially in young patients, help the body to regenerate the supporting tissues damaged by prolapse.
High prolapses, on the other hand, almost always require more vigorous, radical, hence destructive, therapy.
In recent times, hemorrhoidectomy according to Milligan-Morganstabeing scaled down by the use of modern stabilized scleromousse, which can sclerose (close) the hemorrhoid plexuses permanently, without pain and without surgical access.
WHY DO HEMORRHOIDS GET WORSE IN THE HEAT?

Heat, in turn brought about by the increase in temperature related to atmospheric pressure, is a known vasodilator.
This means that the vessels of the human body (arteries, veins and lymphatic vessels) upon increasing temperature dilate and increase in diameter, thus causing more fluid to pass through them (whether blood or lymph).
Vasodilation due to increased external temperature is a natural phenomenon that affects all humans during the hot time of the year.
It is in fact common, for example, for the circumference of wrists and ankles to increase by even a few centimeters during the summer, precisely because the body's vessels increase in diameter.
Under normal conditions, vasodilation is not a worrisome phenomenon: veins and arteries are well elastic, and our body simply adapts to their increased diameter.
In pathological situations, however, where a vessel is already damaged and chronically dilated, as are precisely diseased hemorrhoidal plexuses, vasodilation can exacerbate problems.
Pathological hemorrhoids, already extruded and prolapsed well beyond normal size, increase their volume even more in the heat, thus worsening the symptomatic condition.
Greater dilatation of the hemorrhoid tissues, already exhausted and damaged by hemorrhoidal disease, swells the plexuses even more, which therefore prolapse more and more toward the outside of the anus, and become more likely to become congested, inflamed and injured.
In fact, it is no coincidence that, with the first warm weather, patients with pathological hemorrhoids complain of a systematic increase in symptoms such as burning, swelling, sensation of a foreign body in the anus, increased anal bleeding during or shortly after defecation (rectorrhagia) and intense itching, often caused by thehyper-production of mucus and sweat, typical of the anal area affected by hemorrhoidal prolapse.
These symptoms increased in intensity often last throughout the summer, tormenting the patient for months, and only subside with the arrival of the first cool autumn weather.
Ointments and over-the-counter products, sold in pharmacies for hemorrhoids and not requiring a prescription, are almost always ineffective for treating hemorrhoids.
In fact, these creams do not 'cure' anything, but at best are a palliative aid for symptoms, reducing the itching, burning, or sensation of discomfort typical of pathological hemorrhoids.
Many of these ointments, often prescribed by the pharmacist a little too hastily, contain local anesthetic in small amounts, as well as steroids (cortisone).
The beneficial effect of such preparations is thus provided by the local anesthetic and cortisone: when their effects, which usually last a few hours, are over, the patient begins to experience the symptoms of hemorrhoidal prolapse again.
WHAT CAN BE DONE TO RELIEVE THE DISCOMFORT OF HEMORRHOIDS IN SUMMER?

Hemorrhoidal disease, when initiated, is a chronic and progressive condition.
The severity of prolapse is graded according to its overall volume, and there are four degrees of severity:
- Grade I, internal hemorrhoids visible only by proctoscopy examination;
- Grade II, internal hemorrhoids that prolapse outward only during defecation or during some straining, but spontaneously re-enter the anal canal;
- Grade III, prolapsed hemorrhoids outside the anal canal but traceable by manual maneuvering
- Grade IV, externally prolapsed hemorrhoids no longer traceable within the anal canal
Low grade hemorrhoids, then grade I or II, can be treated and relieved with the right diet modification and medical decongestant therapy.
High-grade hemorrhoids, thus III and above, almost always require more vigorous, radical, destructive treatments.
Currently, traditional hemorrhoid surgery based on the Milligan-Morgan hemorrhoidectomy technique is being supplanted by the new stabilized sclerotherapy scleromousse.
Especially the latter treatment, which has the advantage of being non-surgical and can be easily administered on an outpatient basis, can treat even high-grade cases of hemorrhoid prolapse, sparing the patient access to Surgery.
Ointments and over-the-counter products, sold in pharmacies for hemorrhoids and not requiring a prescription, are almost always ineffective for treating hemorrhoids.
In fact, these creams do not 'cure' anything, but at best are a palliative aid for symptoms, reducing the itching, burning, or sensation of discomfort typical of pathological hemorrhoids.
Many of these ointments, often prescribed by the pharmacist a little too hastily, contain local anesthetic in small amounts, as well as steroids (cortisone).
Thus, the beneficial effect of such preparations is given by the local anesthetic and cortisone: when their effects, which usually last a few hours, are over, the patient begins to experience the symptoms of hemorrhoidal prolapse again.
DRINK A LOT, EAT RIGHT
There is a known correlation between the onset of hemorrhoidal prolapse and diet deficient in adequate hydration and fiber, which in turn causes chronic constipation condition.
In fact, a diet lacking proper daily hydration and the right amount of fiber is not beneficial to the intestines, whose natural peristalsis will be hindered by the formation of constipated stools, which are very hard and not easy to expel.
This condition in turn is considered a trigger for hemorrhoidal prolapse, as hard, difficult-to-evacuate stools always cause an increase in intra-abdominal pressure, which exhausts the supporting tissues of the hemorrhoids and, in the long run, initiates hemorrhoidal disease.
With hot weather, increased sweating, which in turn is a necessary tool for cooling the body, causes our natural hydration factor to dissipate, which we are therefore forced to keep constant by increasing the amount of fluids ingested.
Drinking a lot in summer and, in general, in hot weather, is imperative for our physique and also for our intestines, to avoid the formation of stools that are too hard and difficult then to evacuate.
A good amount of fiber in the diet then, with a preference for cooked leafy vegetables (such as spinach, cabbage, ribs, etc.) ensures the right consistency of stools and their proper volume, thus helping peristalsis to do its job.
Already drinking enough and eating well, preferring fiber-rich vegetables, is a good prevention for pathological hemorrhoids that we should all do all the time, especially in summer.
Patients with established hemorrhoid disease then absolutely must follow an appropriate dietary regimen to maintain soft and easy-to-evacuate stools at all times, avoiding dehydration and dangerous episodes of constipation.
IF HEMORRHOIDS WORSEN IN THE HEAT, VISIT A PROCTOLOGIST RIGHT AWAY

If you are suffering from hemorrhoid disease and notice that, in hot weather, it worsens, you should not search the Internet for remedies of dubious efficacy, which could also endanger your health.
Resorting to self-prescribed ointments, especially if they contain cortisone and a local anesthetic, is also never a good idea: they are useless in combating the cause of prolapsed hemorrhoids, and at best give only momentary and palliative relief.
What you should do instead is not to waste your time and contact a Proctology Physician, who will be able to perform a thorough proctological examination and give you, at last, an effective and decisive medical therapy.
Hemorrhoids must be fought by treating their cause, and to do so you must necessarily contact the Proctology Physician.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- HEMORRHOIDS ARE PHYSIOLOGICAL ARTERIOVENOUS PLEXUSES PRESENT IN OUR ANAL CANAL;
- UNDER NORMAL CONDITIONS, HEMORRHOIDS DO NOT CAUSE DISCOMFORT OR PAIN;
- THE MAIN TASK OF HEMORRHOIDS IS TO VASCULARIZE THE ANAL CANAL AS WELL AS SUPPORT THE SPHINCTER IN FECAL CONTINENCE;
- WE ALL HAVE THREE MAIN HEMORRHOID PLEXUSES: RIGHT ANTERIOR, RIGHT POSTERIOR AND LEFT LATERAL;
- WHEN THE HEMORRHOIDS SWELL, BECOME INFLAMED AND EXTRUDE OUTSIDE THE ANORECTAL CANAL, WE CAN TALK ABOUT HEMORRHOIDAL PATHOLOGY;
- HEMORRHOIDAL PATHOLOGY IS, ALONG WITH DENTAL CARIES, THE MOST COMMON PATHOLOGY IN THE WORLD;
- THE MAIN CAUSE OF THE ONSET OF HEMORRHOIDAL PROLAPSE IS NOT YET KNOWN, BUT TWO MAJOR THEORIES ARE SUSPECTED: MECHANICAL AND HEMODYNAMIC;
- MEDICINE HAS FOR MANY YEARS ASCERTAINED THE CORRELATION OF THE ONSET OF HEMORRHOIDAL PATHOLOGY WITH CERTAIN TRIGGERING FACTORS, SUCH ASCHRONIC LASTIPSIS, AN INCORRECT DIET LOW IN FIBER, CERTAIN SPORTS OR PARTICULARLY STRENUOUS JOBS, PREGNANCY AND CHILDBIRTH;
- HEMORRHOIDAL PROLAPSE, ONCE INITIATED AND UNTREATED, IS USUALLY CHRONIC AND WORSENING;
- THERE ARE FOUR DEGREES OF SEVERITY OF HEMORRHOIDS, RELATED TO THE VOLUME OF PROLAPSE;
- HEAT AND THE SUMMER SEASON ARE DELETERIOUS TO THE SYMPTOMS OF HEMORRHOIDS, WHICH WORSEN DUE TO THE WELL-KNOWN PHENOMENON OF VASODILATION;
- IN HOT WEATHER, THE VESSELS IN THE BODY INCREASE IN DIAMETER, THUS PASSING MORE BLOOD AND WORSENING THE EXTENT OF PROLAPSE;
- THERE ARE A VARIETY OF TREATMENTS FOR HEMORRHOIDS, BOTH MEDICAL AND SURGICAL, DEPENDING ON THE DEGREE OF PROLAPSE;
- A DIET RICH IN FIBER AND WATER KEEPS STOOLS SOFT, PREVENTS EXCESSIVE DEHYDRATION AND ALLOWS EASY DEFECATION, AVOIDING INJURY TO THE HEMORRHOID PLEXUSES;
- A PROCTOLOGIST AND PROCTOLOGICAL EXAMINATION SHOULD BE SOUGHT BEFORE THE ONSET OF THE HOT SEASON, THAT IS, BEFORE THE SYMPTOMS OF HEMORRHOIDS WORSEN

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.