There is a particular form of neoplasm that, after the age of 50, is shown to be the second most common form of cancer (after prostate cancer in men and breast cancer in women(, with higher incidence in the male sex.
It accounts for 11.5% of all known malignancies, and in European Union countries, colorectal cancer accounted for 12.7% of all new cancer diagnoses and 12.4% of all deaths due to cancer.
It is the colorectal cancer, a killer that is almost always silent and invisible, and one that should cause proper apprehension precisely because of its absence of symptoms except in the final stages of its evolution.
Read this page to find out what rectal cancer is, how it originates, and what treatments can eradicate it.
Very often, bleeding from the anus during or shortly after defecation (hematochezia) puts the patient in total distress, who immediately thinks he has rectal cancer.
However, most episodes of anal bleeding are attributable to completely benign conditions, such as hemorrhoidal prolapse and anal fissure.
In fact (and this is not good news for diagnosis), usually cases of carcinoma of the anus or rectum give bleeding episodes only at advanced staging, that is, when by then the tumor mass has acquired considerable volume, and adhesions are now widespread.
What is rectal cancer?
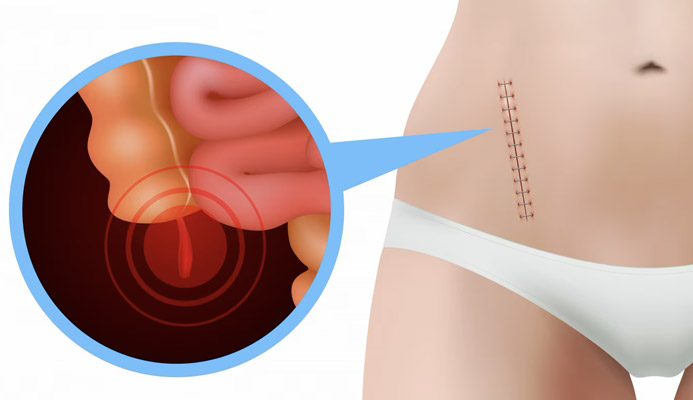
Tumor, or carcinoma of the rectum, is a neoplastic form that originates from the mucosa of the last part of the intestine, i.e., the short tube of the rectum, also including the anal canal and anal orifice area.
Cancer of the rectum is but one form of the more extensive colorectal cancer, that is, that form of cancer that can affect the entire large intestine.
To be precise, rectal cancer composes, percentage-wise, 30% of all intestinal cancers.
What is the origin of rectal cancer?

The origin of rectal cancer is not unlike that of other forms of cancer: it is an uncontrolled, malignant cell degeneration that, in this case, has in the rectal or anal mucosa the starting point.
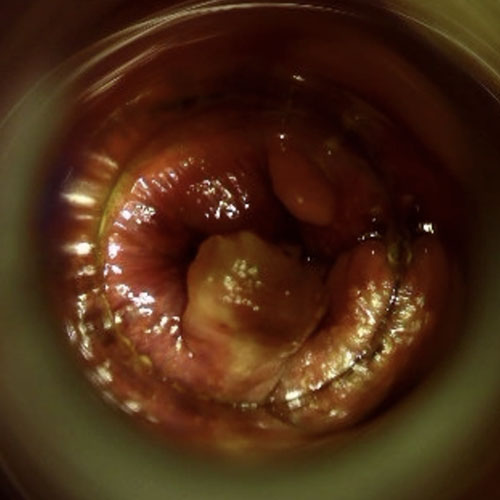
Most malignant tumor formations arise from lesions considered pre-cancerous, such as polyps of the rectum and anus and, not secondarily, anal condylomata that have not been properly removed.
In addition to these pre-cancerous lesions, there are also established risk factors:
- Age over 50;
- Alcohol abuse and tobacco use;
- Obesity and overweight;
- Diet low in fiber and high in fat;
- Familiarity with episodes of colon or rectal cancer;
- Crohn's disease and ulcerative rectocolitis
What are the symptoms of rectal cancer?
Rectal cancer, not unlike other forms of cancer, is asymptomatic in its early stages.
The first symptoms begin to present are at advanced staging, and are not always felt early by the patient.
The first of the typical symptoms, often underestimated because it is also shared with benign hemorrhoidal disease, is anal bleeding during or immediately shortly after defecation (hematochezia).
In advanced stages, depending also on the total volume of the tumor mass and its possible penetration into the sphincters and the peri-rectal panniculus adiposus, hematochezia may also transmute into rectorrhagia, that is, actual anal bleeding even not associated with defecation.
In addition to anal bleeding, several other associated symptoms may also appear, such as:
- Tenesmus, that is, feeling of not having completely evacuated;
- Chronic alteration of alvus, which is often perennially malformed;
- Impellency of defecation, which solvent results in pain;
- Pain in the perineum or pelvis
It must necessarily be reiterated that these symptoms may or may not be present, as well as hematochezia.
One of the greatest dangers of rectal cancer is, in fact, that it can be totally asymptomatic until the final stage, when it has now advanced deep into the tissues and treatment is therefore complicated.
No wonder, then, that the preponderant medical advice is for early diagnosis, using the modern screening protocols currently available at low cost and quick to perform.
How is rectal cancer diagnosed?
The diagnosis of carcinoma of the rectum is made during the proctological examination.
Already, the patient's history, which must be scrupulous and rigorous, should aim to ascertain whether or not suspicious family situations or predisposing conditions (e.g., condylomatous infections that have never been treated in the past) are present.
Possible hematochezia is also a symptom shared with pathological hemorrhoids, and this should be appropriately considered in the clinical history.
The medical history was then followed by the proctotological examination with digital exploration, which is useful for the Proctology Physician to highlight any cancerous lesions of particular significance.
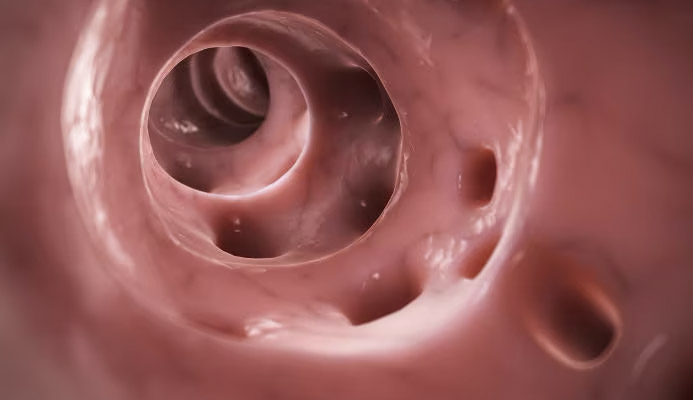
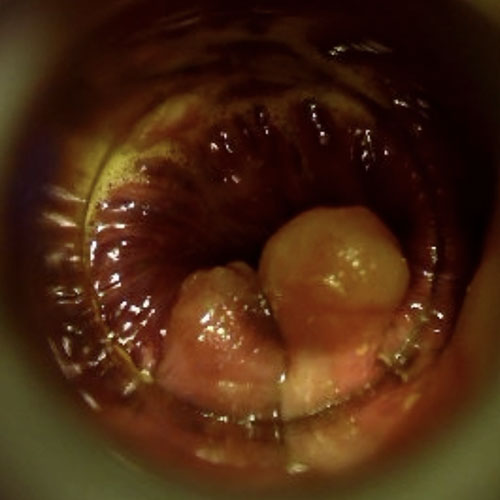
The proctological examination is then obligatorily followed by proctoscopy, performed by means of modern Electronic Endoscopic Videoproctoscopy.
With this examination, the Proctologist is able to inspect the entire rectum and anal canal by means of a special inspection tube and a high-definition video camera capable of capturing even the smallest details.
Videoproctoscopy is a complete visual examination of the entire anal and rectal canal: if there is a cancerous neoformation in the latter part of the intestine, it is definitely detected.
If positive, the Proctology Physician may prescribe complementary diagnostic tests, to assess the staging of the tumor, such as endoanal ultrasound (to detect and evaluate tumor adhesions in the deep layers of the rectal wall and peri-rectal fat) or even a multilayer total body CT scan.
Not infrequently, to get the full picture of the entire intestine and avert or ascertain injury to other areas of it as well, a traditional colonoscopy is also prescribed by the Proctologist.
What is the treatment for rectal cancer?
Treatment for cancer of the rectum or anus is essentially surgical.
Radiotherapy and chemotherapy are supportive therapies, often prescribed to reduce the size of the tumor mass and facilitate its surgical removal, but individually they fail to eradicate tumor degeneration.
The surgical approach, as always, is given by the staging of the tumor as well as its placement in the anorectal canal.
Small carcinomas without deep adhesions can be removed easily with mini-surgery, preserving almost all anorectal function intact.
The lower the lesion gets, that is, the closer it gets to the anal orifice, the more chance there is that the Surgeon will have to provide total removal of the rectum, effectively lowering the colon and joining it directly to the anus, in a procedure called colon-anal anastomosis.
The surgery usually gives excellent results, allowing pain-free healing for the patient and without too much discomfort, with only a temporary deviation of the anus (reducible in a few months) to prevent sagging of unhealed tissues.
In a minority percentage of cases (10% to 20%) the tumor mass infiltrates the sphincter muscles, and this situation leaves no alternative to definitive colostomy, with permanent detour of the anus.
There is, however, a need to specify that modern surgical techniques, combined with early and constant screening, as well as undoubted advances in supportive chemical therapies, are able to treat virtually any type of cancer of the rectum and anus, increasingly with micro-operations that are low-invasive for the patient.
Whatever therapy is proposed for the specific clinical case, therefore, should not be frightening: the absence of pain is almost always guaranteed, so too is the least invasiveness possible.
How often should screening for rectal cancer be done?
Screening for rectal cancer pairs with screening for colon cancer, and is recommended for everyone over the age of 50.
Everyone, no one excluded, even completely asymptomatic individuals.
Screening is performed by colonoscopy examination, which can be either traditional or virtual.
Colonoscopy is an examination that often frightens patients, who often have misinformation and, not infrequently, exaggerated or otherwise vitiated by subjective opinions.
In fact, the examination itself is completely painless, and the patient does not even remember having it done, as it is delivered under deep sedation.
Moreover, the colonoscope instrument is not merely a passive investigative tool, but can operate directly and remove polyps and small lesions, thus avoiding additional surgeries for the patient.
Should one be alarmed when one sees traces of blood on toilet paper or feces?
There's no reason to be worried, but there's for sure reason to further investigate.
And to do so, a specialized proctological examination must first be performed.
Hematochezia, that is, leakage of blood from the anus during defecation, in most cases results from benign conditions such as pathological hemorrhoids or an anal fissure, but it could also be a symptom of colorectal cancer.
That is why there is no need to be frightened, but to seek a specialist's attention right away.
Which Physician should be consulted if rectal cancer is suspected?
The health specialist whose particular expertise is the last tract of the intestines is the Proctologist Physician.
The Proctologist Physician is the white coat who has deep experience in diseases of the rectum and anal canal, and who uses all useful diagnostic tools to investigate without pain and discomfort, such as Electronic Endoscopic Videoproscopy.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- RECTAL CANCER IS A TYPE OF CRANCRO THAT GENERATES FROM THE ANORECTAL MUCOSA;
- STATISTICALLY, RECTAL CANCER COMPOSES ABOUT 30% OF ALL INTESTINAL CANCERS;
- UNFORTUNATELY, LIKE MANY OTHER TYPES OF CARCINOMA, RECTAL CANCER DOES NOT GIVE PARTICULAR SYMPTOMS IN THE EARLY STAGES;
- SYMPTOMS OF RECTAL CANCER ALMOST ALWAYS OCCUR IN THE ADVANCED STAGES OF THE DISEASE, AND ARE OFTEN FUSED WITH THOSE OF OTHER DISEASES, SUCH AS HEMORRHOIDS;
- COLON SCREENING IS A MANDATORY EXAM FOR EVERY PERSON OVER 50, EVEN IF THEY ARE PERFECTLY HEALTHY;
- MODERN SURGERY CAN CURE RECTAL CANCER IF CAUGHT EARLY;
- ONE SHOULD NEVER PROCRASTINATE PROCTOLOGIC CHECKUP AND SCREENING COLONOSCOPY: THESE ARE LIFE-SAVING MEDICAL ACTS, AS RECTAL CANCER IS OFTEN TOTALLY ASYMPTOMATIC;
- ONE SHOULD NOT BE FRIGHTENED IF ONE NOTICES TRACES OF BLOOD IN THE STOOL OR ON THE TOILET PAPER, AS THIS COULD ALSO BE A BENIGN CONDITION, AND NOT NECESSARILY RECTAL CANCER;
- IF YOU NOTICE ANAL BLEEDING AFTER DEFECATION, WHAT YOU NEED TO DO IS TO REMAIN CALM AND BOOK A PROCTOLOGICAL EXAMINATION

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.