Pathological hemorrhoids, that is, hemorrhoids now prolapsed and extruded outside the anal canal, are a problem for millions and millions of people worldwide.
Statistically, hemorrhoidal disease is estimated to be, along with dental caries, the second most common disease in the entire human population, which gives a good idea of the numbers of potential 'hemorrhoid' patients.
In the early 1900s, two British Surgeons, Dr. Milligan and Dr. Morgan revolutionized colonproctology by devising a radical surgical protocol for the tout-court removal of diseased hemorrhoid plexuses.
This protocol, albeit with slight modifications and variations, is still used in the present day, and is called hemorrhoidectomy according to Milligan-Morgan.
Read this page to find out what hemorrhoidectomy according to Milligan-Morgan is: when it needs to be performed, who it can be performed on, and how the postoperative develops.
Modern surgical protocols have perfected the Milligan-Morgan hemorrhoidectomy, which is much less invasive and painful than in the past.
Although the underlying goal is the same, as is the necessary surgical excision of the diseased hemorrhoid plexuses , expedients such as high ligation of the arterial pedicle and mucosal'bridges' left between incisions ensure a much less painful postoperative course for the patient in most cases.
Prophylactic antibiotic therapy, prescribed diet, and the use ofspecific laxatives (only temporary in the days following surgery) also help the patient to evacuate soft stools that are easy to expel, which benefits pain control.
What is hemorrhoidectomy according to Milligan-Morgan?

Hemorrhoidectomy according to Milligan-Morgan is a colonproctology surgical procedure, the purpose of which is the total removal of diseased hemorrhoidal tissues due to hemorrhoidal pathology.
The surgical protocol was originally devised by two British Surgeons, Dr. Milligan and Dr. Morgan, and essentially has remained virtually unchanged to the present day.
This surgery is considered radical: diseased hemorrhoid plexuses are physically removed, through appropriate incisions that, at the end of the operation, are not sutured, but left to heal by second intention.
Until shortly before the introduction of the outpatient stabilized scleromousse technique, hemorrhoidectomy according to Milligan-Morgan was the only radical and resolving therapy for major hemorrhoidal prolapses beyond grade III.
What are hemorrhoids, and why do they get prolapsed?
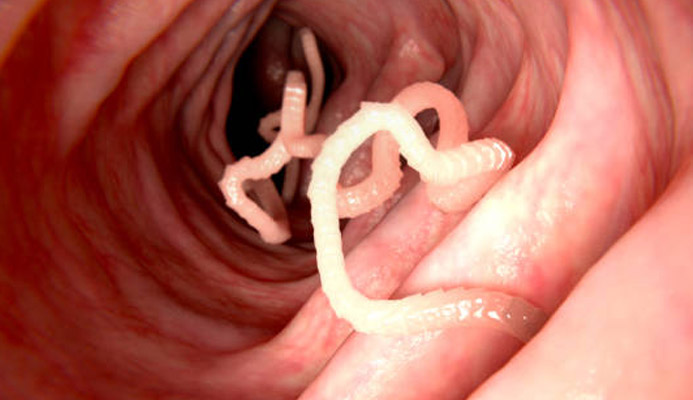
Hemorrhoids are of natural athero-venous plexuses, normally found in our anal canal.
There are three main ones (left side, right front, and right rear), plus two other smaller secondary ones.
The purpose of these plexuses, which resemble soft pads swollen with blood, is to effectively vascularize the entire anal canal and, secondarily, to aid the sphincter muscles in fecal containment.
Under normal conditions, hemorrhoids do not cause any problems, but in certain situations, such as in the case of inflammation, tearing of the anal mucosa, congestion, or exhaustion of the supporting tissues that anchor them in the anal canal, hemorrhoids may extrude and swell excessively, giving rise to hemorrhoidal disease.
Medicine has not yet established a certain and common cause that explains the onset of hemorrhoidal prolapse, but underlying the disease are both mechanical (tissue exhaustion from excessive intraabdominal strains, aging, and collagen decline) and hemodynamic theories.
A certain and almost always present triggering situation for hemorrhoidal prolapse is chronic constipation, which wears down the tissues anchoring the hemorrhoids to the anal canal due to the chronic increase in intraabdominal pressure.
The 'strain' in the constipated person's pouching, the passage of stool that is hardened and difficult to expel because it is dehydrated, in the long run wears down the hemorrhoid tissue, which dilates and prolapses downward, thus giving rise to the condition.
Natural aging, natural pregnancy and childbirth, as well as frequent episodes of diarrhea that tend to become chronic (perhaps the result of irritable bowel syndrome), or even certain strenuous jobs and particular sports can also be considered triggers of hemorrhoid prolapse.
What symptoms do prolapsed hemorrhoids give?

Hemorrhoid prolapse brings a wide variety of symptoms for the patient experiencing it, the most common of which is definitely anal bleeding (rectorrhagia).
This bleeding, which can be copious or spotty (hematochezia), usually occurs during or shortly after defecation due to the passage of stool, which, playfully, rubs the already inflamed and congested outer wall of the hemorrhoids.
The friction therefore creates tissue tearing, hence the bleeding.
In addition to bleeding, which worsens in severity in cases of stubborn constipation, the patient with pathological hemorrhoids also experiences anal burning and itching, often accompanied by a sensation of a foreign body in the anus and, no less frequently, a feeling of never being able to 'empty' completely after evacuation (tenesmus).
To these typical symptoms of hemorrhoid prolapse can be added the complication of the formation of a thrombus (a blood clot) inside the hemorrhoids themselves, which takes the standard of hemorrhoid thrombosis.
This condition, which is extremely painful and capable of completely prostrating the patient, generates what is called a 'hemorrhoidal crisis'.
Milligan-Morgan hemorrhoidectomy, although one of the most successful surgical techniques in the history of proctology, is slowly being replaced by the new sterilized air-stabilized scleromousse.
This medical protocol, developed during the Covid-19 pandemic, has countless advantages for the patient: no surgery in the room, complete absence of postoperative pain, immediate return to sports and work activities, and extremely low cost.
Scleromousse for hemorrhoids is able to resolve, in 95 percent of cases, even severe situations of hemorrhoidal prolapse that once could only be addressed by Milligan-Morgan hemorrhoidectomy.
Is there a degree of severity of hemorrhoids?

Hemorrhoids are conventionally graded according to their extrusion from their original anatomical position on a four-grade scale:
- Grade I hemorrhoids, hemorrhoids that are not yet congestive, of mild prolapse, and still remain totally located in the anal canal;
- Grade II hemorrhoids, with moderate prolapse, extruding from the anal canal only during defecation or during some straining;
- Grade III hemorrhoids, with severe prolapse, which extrude completely from the anal canal but can re-enter it with manual repositioning;
- Grade IV hemorrhoids, with severe prolapse that are permanently prolapsed outside the anal canal and are no longer reducible even with manual maneuvering
Current Medicine is able to achieve excellent results for decongestion of low-grade hemorrhoids, while hemorrhoidectomy is a surgical procedure designed exclusively to solve the problems of high-grade hemorrhoids, grade III and above.
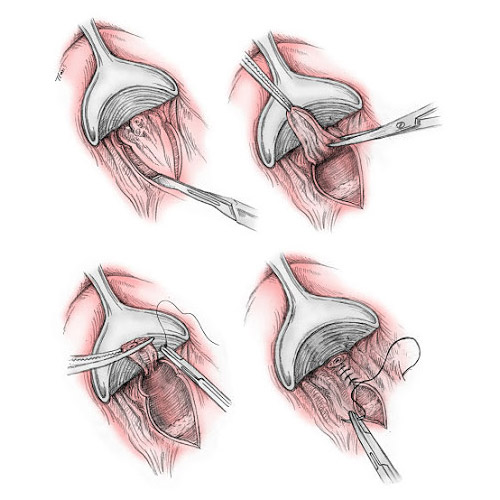
How is Milligan-Morgan hemorrhoidectomy surgery performed?

Hemorrhoidectomy surgery according to Milligan-Morgan is performed under general anesthesia.
After ligating the arterial pedicle that feeds the hemorrhoids, the plexuses are surgically removed, with the Surgeon's preferred instrument: with the cold-blade scalpel, with the electrosurgical scalpel, with the radiofrequency scalpel, with the laser scalpel, etc.
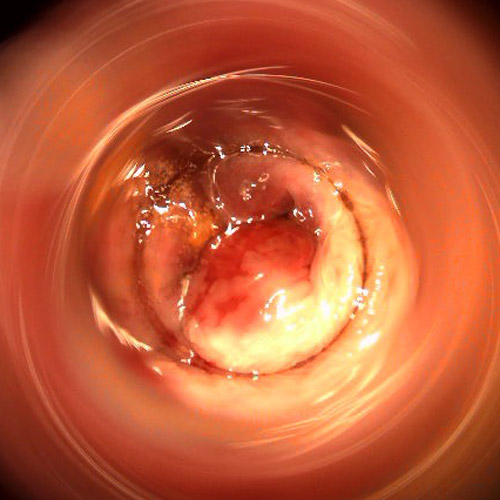
The artery that feeds the hemorrhoids is then cauterized, and the incisions of the surgery, as there are three major hemorrhoid plexuses, leave at the end of the execution the well-mooted 'clover' image.
Incisions are not sutured, only medicated: healing will occur by second intention, in about 90 days after surgery.
The high ligation of the arterial pedicle and the surgeon's ability to leave mucosal bridges, which are essential for wound drainage and to minimize the risk of scar stenosis, allow for a much smoother postoperative for the patient.
Is there pain after Milligan-Morgan hemorrhoidectomy surgery?
Milligan-Morgan hemorrhoidectomy surgery that is performed modernly is much smoother in the postoperative course than the same surgery that was performed decades ago.
The modern surgical technique allows much more respect for the healthy tissues of the anal canal and, therefore, gives much more peace of mind to the patient in the postoperative period.
Modern post-surgical protocols, fortunately different from past protocols in which intestinal blockage was even caused, allow the patient to discharge safely after surgery without excessive pain.
It goes without saying that, being an 'open' technique, i.e., without suture, Milligan-Morgan hemorrhoidectomy cannot provide for an entirely discomfort-free post-surgery, and of this the patient must be mandatorily informed.
The passage of feces over open, healing wounds can cause burning and irritation, which are especially pronounced in the first few weeks after surgery.
Bleeding and overproduction of mucus, usually copious in the first two to three weeks after surgery, are also normal conditions that should not, however, frighten the patient.
The discomfort, burning, or pain of the first few days after hemorrhoidectomy can be contained, however, with a good dietary protocol, which is essential to always obtain soft, well-formed stools that are easy to expel, and the use of common pain relievers.
Not all cases of hemorrhoidal prolapse necessarily require surgery: some degrees of pathological hemorrhoids, such as grade I or II, can be cured very effectively by appropriate medical decongestant therapy, which is usually combined with an adequate diet.
Conventionally, the decision is made to resort to Milligan-Morgan hemorrhoidectomy surgery only when the hemorrhoid prolapse is now irreducible and chronic, seriously affecting the patient's quality of life.
However, since the Covid-19 pandemic, the advent of the new stabilized scleromousse sclerotherapy has profoundly changed the curative approach to hemorrhoids, greatly scaling back the use of hemorrhoidectomy.
After how long does one recover from Milligan-Morgan hemorrhoidectomy?
The tissues of the anorectal mucosa, barring complications, on average heal completely 90 days after surgery.
Sometimes, however, depending on the patient's own degree of healing, it takes longer to reach full healing.
Delays in the total resolution of the surgery are usually caused by postoperative infections, irritation of the area (proctitis), often given by less than excellent patient compliance during convalescence.
After how many days can one return to work once Milligan-Morgan hemorrhoidectomy surgery has been performed?
The patient is usually kept in the hospital for two to three days after surgery.
In the absence of complications, the physician prescribes an appropriate period of home rest, which is usually 15-20 days.
It is possible to return to desk work after that time, while for those who do strenuous work, or work that otherwise involves exertion and heavy lifting, the recovery time is longer, even up to a month (in some cases, longer).
Sports activity can be resumed after about 30 to 40 days, always after endorsement by the physician, and in any case avoiding activities that increase intra-abdominal pressure.
Is hemorrhoidectomy surgery according to Milligan-Morgan definitive?
When well performed, statistics show that Milligan-Morgan hemorrhoidectomy surgery is resolving more than 98% of treated cases.
Who is the surgeon who specializes in Milligan-Morgan hemorrhoidectomy surgery?
Pathologic hemorrhoids are a classic specialty of Vascular Surgery, so usually the Surgeon very well versed in hemorrhoidectomy according to Milligan-Morgan is the Vascular Surgeon (also commonly called Angiologist).
Is there an alternative to Milligan-Morgan hemorrhoidectomy?

Until a few years ago, hemorrhoidectomy according to Milligan-Morgan was the only effective and feasible solution for patients with now advanced and irreducible hemorrhoidal prolapse above grade III.
Minimally invasive outpatient treatments such as the HeLP technique or elastic ligation, for advanced stages of prolapse, were always found to be totally ineffective, so hemorrhoidectomy was the only suitable curative therapy to provide relief to patients with now unsustainable prolapse.
From 2020 onward, however, things have definitely changed.
The advent of modern scleromousse stabilized with sterilized air has completely revolutionized the treatment of hemorrhoids, both mild and advanced stages.
Initially started only as a palliative, pending hemorrhoidectomy surgery, polydocanol scleromousse instead proved to be curative in 95% of treated patients who, after therapy, no longer required surgery.
With this comforting trial, scleromousse has thus become a painless, fast, extremely low-cost alternative that can be administered on an outpatient basis, with all the obvious patient benefits (especially, post-surgical).
Do you suffer from pathological hemorrhoids and are considering performing a hemorrhoidectomy according to Milligan-Morgan? Get an opinion from Dr. troyer

Dr. Luisella Troyer is a Proctologic Surgeon who has been perfected in Milligan-Morgan hemorrhoidectomy for years, which she has helped to constantly improve with her clinical trials.
Dr. Troyer's goal is to give the least postoperative discomfort to her patients, respecting the anorectal tissues and thus ensuring a smoother postoperative course.
In the past few years, Dr. Troyer has begun to successfully use the new sterilized air-stabilized scleromousse, with a protocol that allows her to treat even the most severe cases of hemorrhoidal prolapse without, however, going through compulsory hemorrhoidectomy.
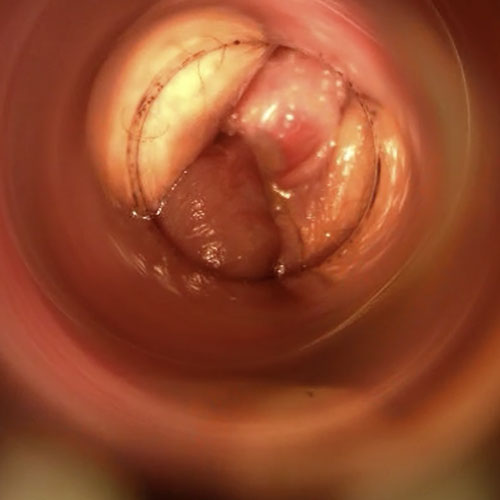
In her clinic in Dubai, Dr. Troyer can accurately diagnose your pathological hemorrhoids and degree of prolapse using an advanced endoscopic examination called Electronic Endoscopic Videoproscopy.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- HEMORRHOIDS ARE NATURAL PLEXUSES CONSISTING OF ARTERIES AND VEINS JOINED TOGETHER, FOUND IN THE ANAL CANAL;
- THE PRIMARY TASK OF HEMORRHOIDS IS TO ADEQUATELY VASCULARIZE THE ENTIRE ANUS AND ANAL ORIFICE, ALSO HAVING AS A SECONDARY TASK THAT OF FECAL CONTAINMENT;
- FOR A LONG SERIES OF TRIGGERING FACTORS, HEMORRHOIDS CAN PROLAPSE AND EXTRUDE OUT OF THE ANAL CANAL, GIVING RISE TOHEMORRHOIDALPATOLOGY;
- THERE ARE DIFFERENT STAGES OF SEVERITY OF PATHOLOGICAL HEMORRHOIDS, DIVIDED ACCORDING TO THE VOLUME OF PROLAPSE;
- PROLAPSE OF HEMORRHOIDS BRINGS CONGESTION OF THE PLEXUSES, INFLAMMATION AND, OFTEN, TEARING, DUE TO THE PASSAGE OF FECES;
- CONSTIPATED PATIENTS, PREGNANT WOMEN AND PARTURIENTS, AS WELL AS PATIENTS WITH PARTICULARLY STRENUOUS JOBS OR SPORTS, MAY BE PARTICULARLY AFFLICTED BY THE PROBLEM OF HEMORRHOIDS;
- PATHOLOGICAL HEMORRHOIDS ARE AN EXTREMELY COMMON DISEASE WORLDWIDE, SECOND ONLY TO DENTAL CARIES;
- MILLIGAN-MORGAN HEMORRHOIDECTOMY IS A SURGICAL TECHNIQUE DEVISED OVER A CENTURY AGO TO COMPLETELY REMOVE DISEASED HEMORRHOID PLEXUSES;
- THE MILLIGAN-MORGAN HEMORRHOIDECTOMY TECHNIQUE DOES NOT INVOLVE SUTURING OF INCISIONS, AND THEREFORE HEALING IS SLOWER FOR THE PATIENT;
- ALTHOUGH SURGICAL TECHNIQUE AND POST-SURGICAL PROTOCOLS HAVE BEEN REFINED OVER TIME, MILLIGAN-MORGAN HEMORRHOIDECTOMY REMAINS A SOMETIMES UNEVENTFUL OPERATION IN RECOVERY;
- CURRENTLY, MANY CASES ONCE ELIGIBLE ONLY FOR HEMORRHOIDECTOMY ARE TREATED WITH THE NEW SCLEROMOUSSE SCLEROTHERAPY

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.