Do you experience extensive and excruciating pain in the anal area, which is especially triggered when you go to the body?
After you defecate do you find that you are bleeding from the anus, and do you find bright red streaks of blood on the stool or on the toilet paper?
Anal fissure is an extremely painful condition that can afflict the anus and anal canal and which, if left untreated, tends to become chronic over time, becoming a real sore.
Read this page to find out what anal fissure is, what conditions cause it, how it is diagnosed, and how it can be treated.
Statistically, laceration of the anal mucosa caused by particularly hard stools, typical of constipated individuals, is one of the main causes of injuries that then, in a small percentage of cases, then chronicise an anal fissure.
Fortunately, only a small percentage of them then develop into a chronic ulcerative lesion requiring medical or surgical theapy.
What is an anal fissure?
Anal fissure is a lesion (wound) of the anal canal, characterized by its slow or completely absent healing.
Conventionally, all anal canal lesions that do not heal spontaneously in about four to six weeks are considered potential fissures, although this timeline should be taken as a generic guideline.
Anal fissure has many features similar to an ulcer and, in fact, it is, showing peculiarities of the sore in the strict sense: slow or very slow healing, bleeding on rubbing, formation of fibrotic tissue of the wound margins, tendency to formation of chronic granulation tissue, which does not allow healing.
Anal fissure can affect any district of the anal canal, but it usually afflicts the posterior part of it.
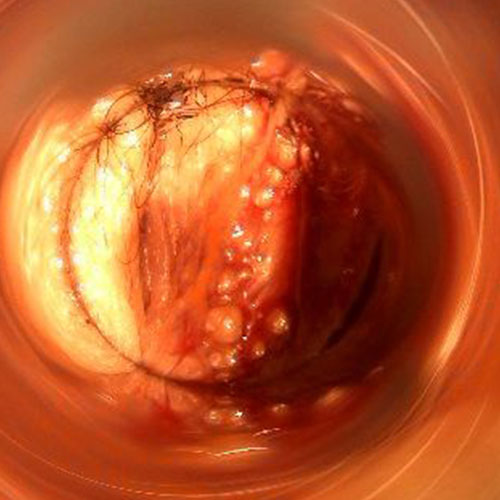
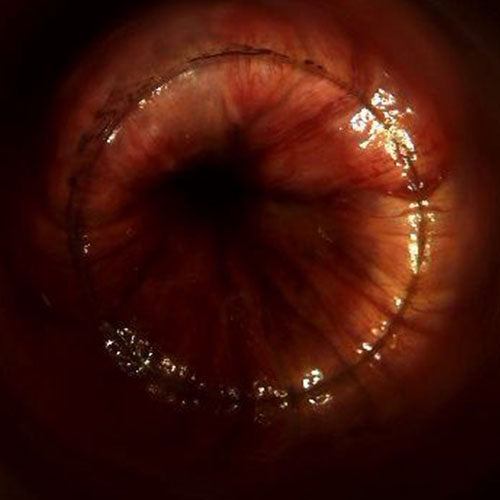
What does anal fissure look like?

The laceration of the fissure always occurs vertical to the anal canal, parallel to the natural pleating of the anal orifice.
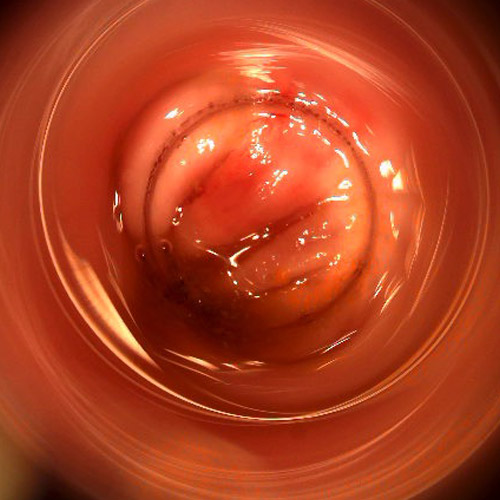
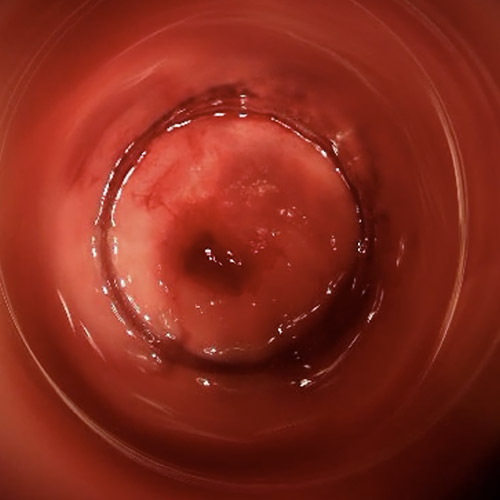
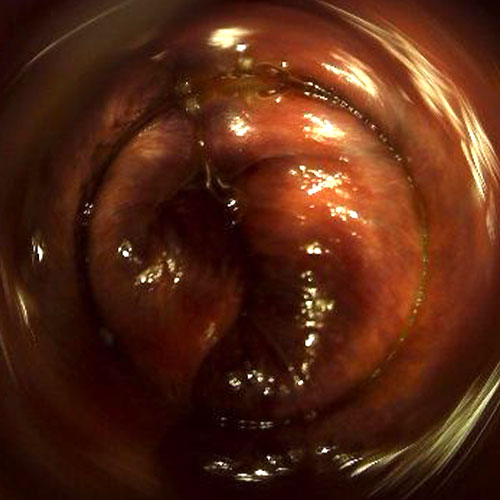
The lesion may be small or large, and appears on videoproctoscopy examination as a reddened wound, almost always bleeding as the proctoscope passes, with hard, fibrotic margins if already chronic over time.
Fresh, not yet chronic, fissures have reddish and bloody bottoms, as opposed to longstanding fissures with whitish bottoms (due to diseased granulation tissue) and, sometimes and in the case of deep lesions, the extent of the wound reaches as far as the sphincter muscle tunic.
Ragging well within the anal canal cannot be observed directly without endoscopic examination, and common proctoscopy, performed with the common optical proctoscope, often does not allow optimal observation of the lesion.
Therefore, for a more accurate and easier diagnosis for the proctologist, videoproctoscopy examination should be used, which can detect even small-sized fissures by perfectly visualizing their bottoms and edges.
What are the causes of anal fissure?
A fissure is a wound, and like any wound its origin is traumatic.
The most common cause of this trauma is the passage of particularly hard stools, typical of the constipated people, which are capable of tearing the delicate anal mucosa.
Frequent diarrheal episodes, with particularly acidified stools, are also capable of causing lesions that give rise to a fissure.
Then there is the statistically minor but present possibility that sexual intercourse that is not particularly lubricated can cause a wound that will later give rise to a fissure.
Regardless of the traumatic triggering event, the real cause of failure to heal anal fissure is, in most cases, a hypertonus of the internal sphincter muscle, which, stressed by the pain that causes the fissure, contracts with constant spasms, which in turn worsens the vascularization of the area and does not allow the fissure to heal.
In practice, the fissure itself urges the internal sphincter (which is an involuntary muscle) to contract, and this spasm, repeated constantly, does not allow the wound to heal.
A bit of a vicious cycle, which allows the ulcer to become self-sustaining and thus become a chronic plague.
What are the symptoms of anal fissure?
The most important symptom that alarms the patient and prompts him or her to urgently go to the doctor (often, even to the emergency room) is the stabbing pain that the fissure causes during and immediately after defecation.
Such pain, reported as excruciating, is often accompanied by anal burning and itching, and cases are not uncommon in which its duration goes well beyond the act of evacuation, extending even for hours afterward.
Coupled with the pain, the patient also experiences bleeding during defecation, with the presence of reddish streaks on toilet paper and stool (hematochezia), which usually puts a great deal of fear into the patient and makes urgent recourse to proctological examination.
This intense pain during and after defecation often and frequently depresses the patient, who voluntarily or involuntarily (in an unconscious reflex) delays evacuation more and more, developing full-blown constipation.
In turn, constipation worsens the quality of the stool, making it harder and, therefore, able to further tear the fissure, preventing or slowing its healing.
Almost always for very inflamed fissures, there is the concomitant formation of a hypertrophic papilla right at the apex of the fissure, resembling a polyp or hemorrhoidal prolapse, which is often mistaken by the patient for just that.
Such a papilla may extrude from the anus during evacuation, and is generally a complication of the fissure that worsens its healing.
If the fissure is near the edge of the anal orifice, a marisca, or particularly reddened and painful skin protuberance, may also appear.
In the (rare, but possible) event that the fissure becomes infected and initiates an anal abscess, the appearance of a fistula should also be budgeted for.
Like any other smooth muscle, the internal sphincter is an involuntary muscle.
This means that we cannot control it directly, as we do the external sphincter, but its contractures and decontracturesare automatically managed by the nerve ending.
A particular hypertone of the internal sphincter, that is, increased spasms and contractions compared to normal,are the main reason why anal fissures do not heal.
Sphincter spasms, in fact, worsen the blood and oxygen supply to the lesion, preventing it from healing.
The curious thing is that these spasms are caused by the very fissure itself, which automatically stimulates the internal sphincter muscle to contract.
Basically, a dog eating its own tail, feeding the fissure.
How is anal fissure diagnosed?
Diagnosis of anal fissure is made by proctological examination by clinical evaluation and proctoscopy.
Digital exploration conducted by the proctologist already directs the specialist to the diagnosis of a fissure, but it is still confirmed by proctoscopy examination.
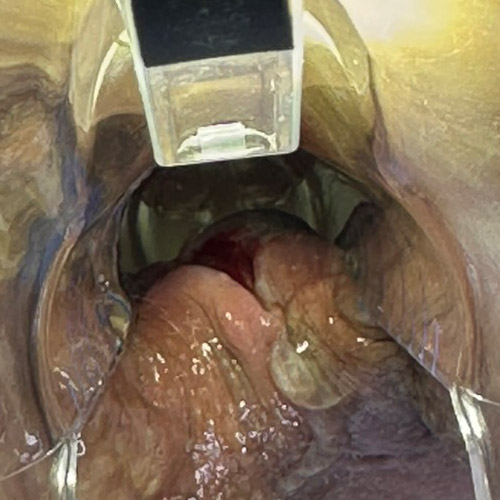
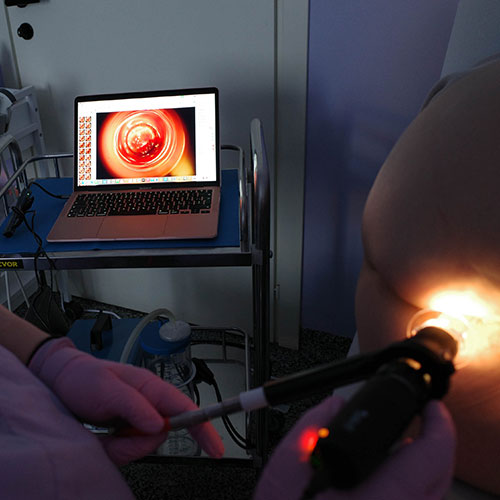
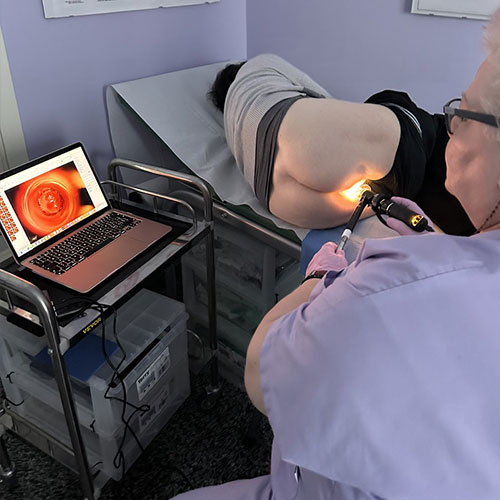
Traditional proctoscopy, performed with an optical proctoscope, has been superseded, in medical offices of excellence by Electronic Endoscopic Videoproscopy.
A painless examination, performed entirely digitally, which by means of a high-definition video camera is able to capture, in real time, even the smallest detail of the anal and rectal canal, allowing immediate identification of the fissure, its location and stage.
In case the Proctologist suspects sphincter hypertone, the patient may also be prescribed anorectal manometry examination.
Where there is the presence of pus or otherwise infected excretions, the proctologist may also prescribe an endoanal ultrasound to complete the proctologic evaluation.
What is the appropriate treatment for treating anal fissure?
Most anal fissures heal spontaneously over time, without requiring any medical or surgical treatment.
This healing time can, however, be facilitated by good behavioral and dietary rules, which are based on encouraging the expulsion of soft, well-formed stools that are not constipated or diarrheic, and good cleaning of the anal area.
In the acute phase of a fissure, soothing and healing creams can be prescribed, as well as gentle, emollient and healing-stimulating cleansers (e.g., excellent hyaluronic acid mousses).
The stool, again, should be kept as regular and soft as possible, with the intake of suitable amounts of fiber, fruits, vegetables, and, if required, also the support of probiotics.
In the case of established sphincter hypertone, it is necessary to relax the muscle with appropriate medical therapies, such as the use of thermal anal dilators (highly effective and easy to use) or special nitroglycerin ointments.
The use of botulinum toxin injections may also be considered, to help the internal sphincter relax and not contract excessively.
When should surgery be used to treat anal fissure?
Surgical therapy is reserved exclusively for those fissures that result refractory to adjuvant and medical treatments.
Fortunately, this type of fissure is statistically rare, affecting only a limited number of cases.
In cases of chronic sphincter hypertone and insensitive to drug treatment, generally the indicated intervention is sphincterotomy, that is, incision made with a certain protocol of the internal sphincter, which aims to reduce its tone.
This intervention is effective, but there is a chance (albeit small) of later developing some form of fecal incontinence.
Long-standing chronic rhagades with hard, fibrotic margins and whitish background are unable to heal spontaneously unless helped by a special procedure known as fissurectomy.
With fissurectomy, the Proctology Surgeon totally removes the lesion by incising a lozenge around the fissure, effectively turning diseased fibrotic tissue into healthy tissue, which will then tend to heal spontaneously in a few weeks.
Fissurectomy is the always preferable surgery, whenever possible, to sphincterotomy: the healing time of this surgery, in fact, is extremely short, and the original functionality of the sphincter is always preserved.
Which Physician can diagnose and treat anal fissure?

Anal fissure is a specialty of Proctology, which is that part of Medicine that studies and treats diseases of the rectum, anus, and anal orifice.
The Proctologist Surgeon is therefore the figure of reference for anal fissure, and is the health professional who can diagnose the lesion and treat it, both pharmacologically and, if necessary, surgically.
Do you suffer from a painful fissure and are you from Dubai? Dr. Luisella Troyer is here to help you

Dr. Luisella Troyer is a Vascular Surgeon specializing in Proctology, who has been studying and treating all diseases of the rectum and anus for over 30 years.
In her clinic in Dubai, Dr. Troyer can help you accurately diagnose your anal fissure by advancing the fully digitized examination of Electronic Endoscopic Videoproctoscopy.
A modern, painless examination of exceptional diagnostic ability that will allow the actual status of your fissure to be assessed and thus arrange for the right treatment.
Thirty years of Vascular Surgery and Proctology for your well-being, excellence care of anus lesions and great medical technology, to solve your fissure problem without pain.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- ANAL FISSURE IS A LESION OF THE ANAL CANAL THAT HAS THE CHARACTERISTIC OF HEALING SLOWLY, OR NOT HEALING AT ALL, BECOMING CHRONIC IN A FULL-BLOWN ULCER;
- NOT ALL ANAL FISSURES BECOME CHRONIC, INDEED: ONLY A SMALL PROPORTION OF ANAL LESIONS BECOME A FISSURE;
- FORTUNATELY, A VERY SMALL PERCENTAGE OF FISSURES REQUIRE MEDICAL TREATMENT:MOST HEAL SPONTANEOUSLY, ALBEIT OVER A MEDIUM TO LONG TIME;
- ANAL FISSURE IS USUALLY VERY PAINFUL, ESPECIALLY DURING DEFECATION, AND HAS THE CHARACTERISTIC OF BLEEDING OFTEN;
- ANY WOUND TO THE ANAL CANAL CAN, THEORETICALLY, BECOME A FISSURE;
- FAILURE OF THE FISSURE TO HEAL USUALLY RESULTS FROM HYPERTONE OF THE INTERNAL SPHINCTER MUSCLE , WHICH, BY CONTRACTING IN SPASM, WORSENS THE VASCULARIZATION OF THE AREA AND PREVENTS THE WOUND FROM HEALING;
- FRESH FISSURES CAN BE TREATED WITH THE RIGHT MEDICAL THERAPY, WHILE CHRONIC FISSURES, WITH FIBROTIC MARGINS AND ASSOCIATED WITH CERTAIN SPHINCTER HYPERTONE, USUALLY REQUIRE SURGICAL REVISION;
- SPHINCTEROTOMY IS THE CALCULATED INCISION OF THE INTERNAL SPHINCTER, WITH THE AIM OF LOWERING ITS PRESSURE TONE AND ALLOWING THE FISSURE TO HEAL;
- FISSURECTOMY, ON THE OTHER HAND, IS THE TOTAL REMOVAL OF THE NOW FIBROTIC FISSURE, WITH THE CREATION OF A NEW HEALTHY WOUND THAT WILL BE ABLE TO HEAL

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.

















