There is a tumour that alone accounts for 10% of all cancers diagnosed worldwide and, among men, is the second largest cancer after prostate cancer, while in women it is second only to breast cancer
Bowel cancer, also called colorectal cancer, is a subtle tumour, extremely dangerous as it rarely gives obvious symptoms, except in the final stages of its staging.
This is why it is important to perform regular screening checks after a certain stage of life, the only ones that can really make a difference in prevention and, ultimately, in preserving life.
Statistically speaking, although the intestine is still a single organ, there is a certain differentiation between colon and rectal cancers, as the two types of carcinomas have significant differences in terms of both clinical and, not least, cell degeneration.
Read this page to find out what rectal cancer is, its symptoms, what causes it and what preventive screening can diagnose it early.
Among all cases of bowel cancer in general, rectal cancer has the minority statistic.
In fact, it is estimated that only 1/3 of all bowel cancers are located in the anorectal canal.
The remainder, that is, 2/3 of cases, are cancers of the colon, particularly of its descending part and the sigma.
WHAT IS a RECTAL CANCER?
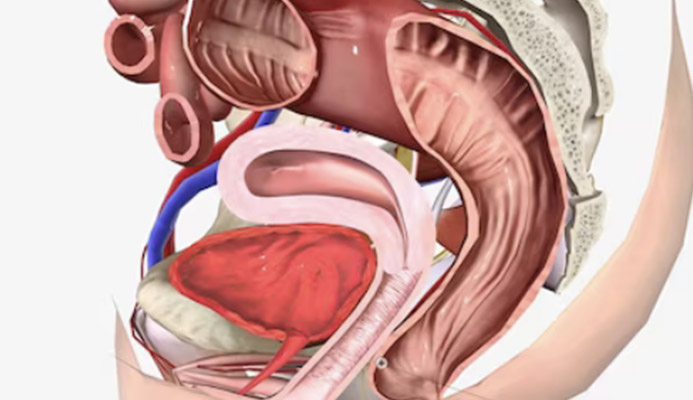
Cancer or carcinoma of the rectum is a neoplasm of malignant origin, occurring in the last part of the large intestine, i.e. the anorectal canal.
Although colon cancer in general is the second most common cancer in the world, for both men and women, rectal cancer holds a minority statistic in colon cancers, about 1/3 of all known clinical cases.
Of all bowel cancer cases in general, rectal cancer has the minority statistic.
The remainder, i.e. 2/3 of cases, are tumours of the colon, in particular of its descending part and of the sigma.
WHAT CAUSES RECTAL CANCER
Cancer of the rectum arises directly from the anorectal mucous membrane, mostly from an adenoma (a polyp) of the rectum.
Not all polyps degenerate into a malignant neoplasm: the oncological potential varies depending on several factors, including the size of the adenoma and its particular cell conformation (the histology of the cells forming it).
Generally, the transformation of an anorectal polyp into cancer is a process that takes a long time, usually years.
The specific reasons for the formation of adenomas are not known to medicine, but it is suspected, not unlike other neoplasms, that the reproductive malformations of the mucous membrane cells are dueto natural ageing and degradation of cell replication and hereditary factors.
Lifestyles, especially diet, can also play a role in triggering rectal cancer.
Diets that are too rich in irritating foods, or in any case foods that constantly inflame and irritate the delicate anorectal mucosa, force the body to regenerate intestinal cells more quickly and to a greater extent, thus increasing the risk that, especially in the adult phase of life, one of them will ‚Äėgo berserk‚Äô, initiating malignant replication or otherwise giving rise to an adenoma.
THERE IS AN AGE PREFERENCE FOR RECTAL CANCER?

Cancer of the rectum, like that of the intestine, predominantly affects individuals, both male and female, after the age of 50.
The reasons for this onset in later life are not yet known to medicine, but it is generally assumed to be due to the known degeneration of chromosome telomeres, which, with natural physiological ageing, degrade and are more likely to replicate cells with defective DNA.
To this, one can add a minority, albeit significant, percentage of patients also under 50, but with known cases of rectal cancer in the family.
Thus, even in this type of cancer, there is the danger of familial inheritance.
Although it is not known to science why, rectal cancer is more prevalent in males than in females, with a ratio of 2 to 1.
WHAT ARE THE SYMPTOMS OF RECTAL CANCER POLYPS?

Cancer of the rectum is a very subtle cancer, as it is in most cases asymptomatic at least in its early stages.
When symptoms do appear, it is almost always an indication of a very advanced stage of the tumour.
This makes preventive screening extremely important, since it is the only examination that can establish whether or not rectal cancer is present in its early stages.
That being said, possible symptoms of the presence of a rectal tumour may be:
- Haematochezia and rectorrhagia, i.e. spotty or copious bleeding from the anus, usually after evacuation (but which can also occur spontaneously)
- Chronic, progressive and worseningdiarrhoea or constipation, which was not previously present in the patient
- Chronically poorly formed stools
- Foreign body sensation in the anus
- Prostatitis, i.e. inflammation of the prostate (gland adjacent to the rectum)
- Bowel tenesmus, i.e. the sensation of not having completely evacuated even shortly after defecation
- Anemas
It bears repeating, however, thatthe most frightening symptom of rectal cancer is precisely the absence of symptoms, even in the presence of constant tumour expansion.
Statistically, most episodes of hematochezia(bloodstains on stool and toilet paper) or rectorrhagia, i.e., copious loss of blood from the rectum, are due not to neoplasms but to benign pathologies.
Such pathologies are mainly due to hemorrhoidal prolapse, that is, pathological hemorrhoids, or anal fissures.
This, however, should not let us rest on our laurels and disregard the fundamental importance of colorectal cancer screening, which is mandatory for everyone after the age of 50.
HOW TO DIAGNOSE a RECTAL CANCER?
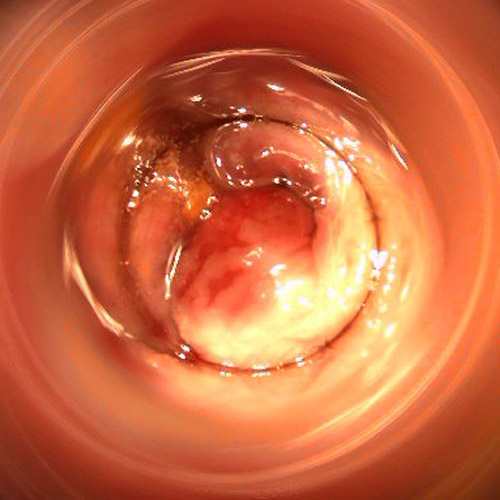
For its diagnosis, rectal cancer requires a compulsory videographic examination of the entire rectal canal.
This examination is carried out by means of a proctoscopy, performed with a video camera that inspects the entire ano-rectal canal, from the rectal ampulla - close to the junction with the sigma - to the anal orifice.
In case of visual confirmation of the tumour's presence, a tissue biopsy must also be performed, taking a sample of the mucous membrane during the examination.
Tumour staging is performed with the indispensable pelvic and abdominal CT scan, to which the physician may also associate a pelvic MRI, which is especially useful for tumours of the lower rectum, i.e. particularly close to the anal canal.
WHAT IS the RECTAL CANCER SCREENING?

Screening for rectal cancer is a non-invasive examination that allows the proctological surgeon to assess the presence or absence of neoformations, both cancerous and adenomatous, in the anorectal canal.
Together with colon cancer screening, which shares the same inspection procedure but uses a different, more invasive examination (colonoscopy), rectal cancer screening is an examination considered to be ‚Äėlife-saving‚Äô, since it is the only one that can establish the presence of a carcinoma in the anorectal area with precision, even in the absence of symptoms.
The screening examination is a visual and operator-dependent examination: it is performed by a physician with strong skills and experience in colon proctology - the branch of medicine that studies and treats pathologies of the intestine and the last tract, the rectum - and is an examination recommended for all subjects, even those in apparent health, who are over 50 years old.
Screening for rectal cancer is different from screening for bowel cancer: although the objective of the two examinations is the same, i.e. to search for the presence of a cancerous neoformation or one that may become one, the goal is different.
In fact, bowel cancer screening covers the entire colon, i.e. from the anal orifice to the cecum, where the large intestine joins, thanks to the ileocecal valve, the ileum of the small intestine.
Rectal cancer screening, on the other hand, specifically examines the anorectal canal, i.e. from the anal orifice to the rectal ampulla (about 12-13 cm in average length).
Rectal cancer screening is different from the faecal occult blood test, which is often recommended as a general screening for colon cancer: it is a precise and specific videographic examination, focusing exclusively on the anorectal canal
HOW the RECTAL CANCER SCREENING IS PERFORMED?

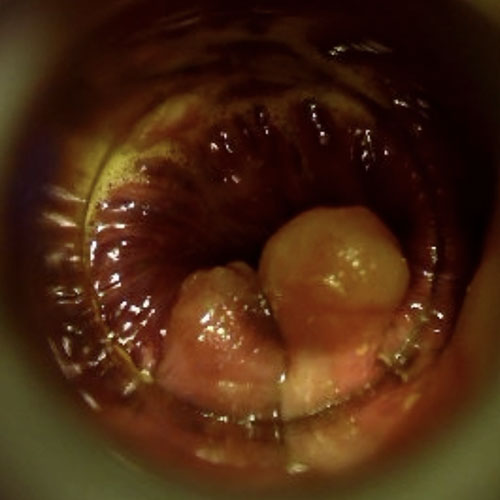
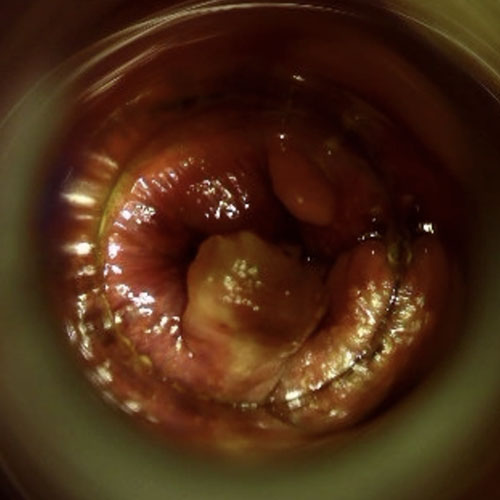
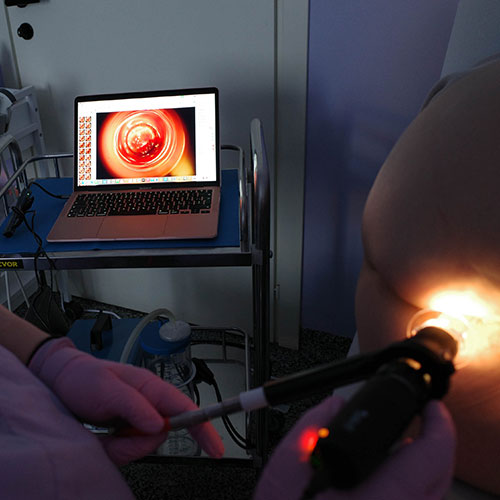
The rectal cancer screening examination is performed using a video, high-definition probe inserted into a 130-mm proctoscopic tube.
The tube is inserted by the operator without pain for the patient, thanks to specific breathing maneuvers and the use of special lubricating ointments containing a little local anesthetic.
The anorectal canal is then illuminated by a light source, nowadays LED, and is widened and stretched by insufflation of air.
The examination is performed retrogradely, that is, starting from the rectal ampulla to the anal orifice, and takes about 10 minutes.
The operating Physician, assisted by the trained technician, records the entire examination on video, looking for polyps or tumor formations present in the anorectal canal, and sees the inspection in real time on the operating screen, connected to a computer.
Modern video cameras can achieve advanced resolutions, higher than 1080p, with magnifications of even more than 20x.
This allows the clinician to have the highest accuracy of details, even the smallest, such as small polyps even smaller than 1mm.
If a suspicious formation, such as a polyp, is detected, the Physician may intervene to remove it using special operating instruments, directly by passing them through the proctoscopic tube.
Modern processing software allows the physician not only to record the examination in digital format, but to extrapolate individual frames, which can then be included in the final medical report for the patient.
Is rectal cancer screening the search for occult blood in stool?

No, rectal cancer screening is a videographic examination, that is, it visually inspects the anorectal canal.
The search for occult blood in the stool is a test instead of a laboratory test, where the patient's stool is analyzed under a microscope for, precisely, blood traces, which could be due to the presence of intestinal lesions.
The fecal occult blood test is not diagnostic confirmatory: it is a test that, if positive, may direct the Physician to further investigation for the patient, but that, by itself, does not give certainty of the presence of a cancerous lesion.
The fecal occult blood test is inherently fallacious, as it looks for any trace of blood, even from benign formations such as fissures or hemorrhoids.
Indeed, it is not recommended for patients with already known hemorrhoidal disease, with already diagnosed anal fissures, with frequent and known diverticulitis, or with chronic auto-immune bowel disease, such as Crohn's disease or ulcerative rectocolitis.
Patients with chronic diarrhea or stubborn constipation, caused by irritable bowel syndrome or untreated constipation, may also have false-positive results on fecal occult blood testing.
It should be remembered that, statistically, a large proportion of detected episodes of occult blood in the stool are attributable to benign formations, such as pathologic hemorrhoids or fissures, and although the test is still absolutely useful for patients over 50, its positivity should not, however, give rise to early concerns.
Is rectal cancer screening equivalent to colonoscopy?

No, rectal cancer screening is a direct visual examination of only the last part of the intestine, that is, the anorectal canal.
It is performed by means of an Electronic Endoscopic Videoproscopy, and not by means of a videocolonoscope.
Videolonscopy is a similar but complete examination of the entire large intestine from the anal orifice to the cecum.
This test is the test of choice for colon cancer screening, and is offered-because of its cost and patient -unfriendly preparation- usually after a positive test for fecal occult blood.
It is possibile to save a lot of money and give a better service to the patient, by first performing a digital proctoscopy examination to assess whether the traces of blood detected in the stool are not instead attributable to a more common hemorrhoidal prolapse or the presence of a fissure.
When is it good to screen for rectal cancer?
Screening for rectal cancer is recommended as a good preventive examination for all individuals after the age of 50 or even earlier if the family has had any established cases of rectal cancer.
Rectal cancer screening is not an alternative to colon cancer screening, which instead requires video colonoscopy for accurate diagnosis.
Instead, it can be a useful test if there is a positive test for occult blood in the stool before performing a colonoscopy, to ascertain whether the blood presence in the stool is due to benign problems, such as pathologic hemorrhoids that have never been diagnosed, and not necessarily a tumor.
I tested positive for fecal occult blood, is it good to perform rectal cancer screening?
Statistically, most cases of hematochezia, that is, bleeding from the anus, are attributable to benign conditions, such as pathological hemorrhoids.
Although colonoscopy is a comprehensive video examination, which can also diagnose rectal polyps or pathological conditions of the rectum, it is an invasive and expensive examination.
Many cases of occult blood in stool on video colonoscopy examination turn out to be caused by benign conditions, such as proctitis, intestinal inflammation, pathological hemorrhoids, and anorectal fissures.
According to this statistic, if the presence of occult blood in stool is detected, it is therefore good to first perform a localized screening at the anorectal canal as the first examination of choice.
If it comes back negative, in the absence of lesions that would justify the presence of occult blood in the stool, then the more invasive colonoscopy examination is a must.
Is rectal cancer screening by electronic proctoscopy invasive?
No, in the most absolute way.
The examination, unlike video colonoscopy - which requires troublesome preparation -is totally painless, and requires no special preparation.
The screening examination can be repeated even several times in a short time, is performed on an outpatient basis, and allows for immediate patient discharge.
In other countries with advanced health care systems, such as the United States, videographic screening of the anorectal canal alone is now the norm for rectal cancer prevention, reserving access to colonoscopy only for cases that are negative on proctoscopic examination.
A rational and sensible choice that is much more accurate than fecal occult blood testing alone, minimally invasive for the patient, and also keeps costs down for the facility that delivers it.
Which physician specializes in rectal cancer screening?
The Physician with great experience in anorectal problems, including rectal cancer, is the Proctologist Surgeon, that is, a Physician perfected in diseases of the anus and rectum.
Therefore, he is the one who should be approached to perform video screening of the anorectal canal.
Do you want to perform rectal cancer screening by video examination? Contact Dr. Luisella Troyer

Dr. Luisella Troyer is a Vascular Surgeon with over two decades of experience and practice in Proctology and prevention of neoplasia of the rectum and anus.
At her clinic in Dubai, Dr. Troyer can perform rectal cancer screening using a modern, fully digital, electronic proctoscope that can immediately report the outcome of the examination.
The screening performed by Dr. Troyer is painless, requires no preparation, and allows immediate discharge of the patient, who can return to work and daily activities soon after.
Rectal cancer screening can be performed by any patient, even those under 50: it is noninvasive and painless, and may be indicated as complete with fecal occult blood testing before a more invasive colonoscopy is performed.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- COLON CANCER IS THE SECOND MOST COMMON CANCER FOR MEN, SECOND ONLY TO PROSTATE CANCER, AND FOR WOMEN, SECOND TO BREAST CANCER;
- RECTAL CANCER IS AN INTESTINAL CANCER LOCATED IN THE LAST PART OF THE INTESTINE, THAT IS, THE ANORECTAL CANAL;
- STATISTICALLY, 1/3 OF ALL INTESTINAL CANCERS ARE RECTAL CANCERS;
- RECTAL CANCER AND COLON CANCER, ALTHOUGH BOTH INTESTINAL TUMORS, HAVE DIFFERENT CHARACTERISTICS;
- RECTAL CANCER IS IN MANY CASES ASYMPTOMATIC, AND OFTEN THE PATIENT WITH IT IS NOT AWARE OF ANYTHING EXCEPT AT AN ADVANCED STAGE OF THE DISEASE;
- RECTAL CANCER IS STATISTICALLY MORE LIKELY AFTER THE AGE OF 50, BUT IT CAN ALSO OCCUR IN YOUNGER INDIVIDUALS, ESPECIALLY THOSE WITH A FAMILY HISTORY;
- RECTAL CANCER SCREENING IS BASED ON A VIDEO EXAMINATION, PERFORMED WITH A SPECIAL PROCTOSCOPIC TUBE;
- RECTAL CANCER SCREENING DOES NOT REPLACE COLON CANCER SCREENING;
- ONLY THE ANORECTAL-RECTAL TRACT IS INSPECTED IN RECTAL CANCER SCREENING, WHEREAS VIDEO COLONOSCOPY EXAMINES THE ENTIRE COLON FROMANUS TO CECUM;
- MOST ANAL BLEEDING AND THE REPORT OF TRACES OF BLOOD IN THE STOOL ARE ATTRIBUTABLE TO BENIGN PROCTOLOGIC DISEASES, SO THE POSITIVE PATIENT MUST REMAIN CALM, AND NOT PANIC

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.