Have you had anal intercourse with your partner, and now you have intended pain in the anus, especially when you have to go to the toilet?
There may be lesions in the delicate anorectal mucosa that, if left untreated, can give rise to persistent anal fissures.
You don't have panic, but keep reading this page: it was written by Dr. Luisella Troyer specifically to give you all the information you need in the case of anal injuries after intercourse.
Remember that, however accurate and scientifically correct they may be, this information is no substitute, however, for a specialized proctologic examination, which, in case of persistent anal pain, Dr. Troyer suggests you do anyway.
The English term ' pegging ' refers to that sexual activity of male penetration, performed bya woman by means ofa post-female penis called a strap-on dildo in technical jargon.
There is no definite record of its adoption in ancient times, but its 'commercial' explosion came in the late 1990s, when a large sex toy manufacturer decided to expand the business beyond female homosexual couples, expanding it to straight couples as well.
The practice of pegging can seriously injure the anal mucosa: it should never be practiced with oversized dildos, should not be done for an excessive period of time, and, most importantly, should be accompanied by uninterrupted and adequate lubrication.
The injuries that a mechanical object can cause to the anal mucosa can be serious and require emergency proctological care, so the practice (if it is welcome) should still be done safely, and in any case stopping at even the slightest hint of pain or bleeding.
What is the anal orifice?
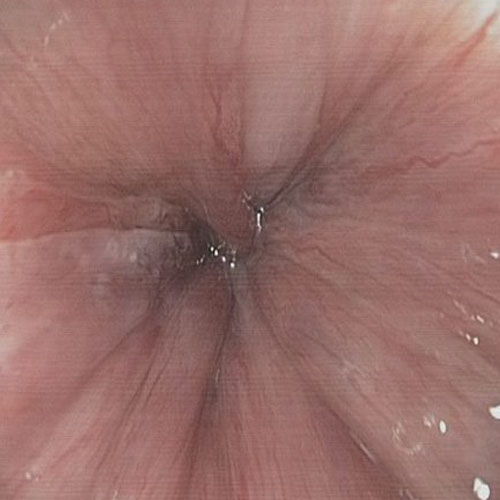
The anal orifice is the last part of the intestine and, in general, the very last part of the long gastrodigestive tube, which makes up the entire human digestive system.
The anal orifice is the body cavity placed diametrically opposite to the mouth, and its function is also opposite: while the oral cavity serves to insert nutrients into the body, the anal orifice is the opening from which the body discharges food waste, which is no longer functional for our metabolism.
Obviously, we are talking about stool, that is food debris composed mainly of indigestible fiber and bacteria.
The anal orifice has two main states: it is tight for much of the day, thus preventing mucus, feces and gas from leaving the body, and is instead opened (released, in medical terms) when there is a need to discharge.
These two states are controlled by two donut muscles that surround the entire anus and part of the rectum, called sphincters.
The sphincters are concentric: the first, the internal sphincter, is a smooth and involuntary muscle, that is, automatically governed by the involuntary nervous system.
In contrast, the external sphincter, which surrounds the internal sphincter, is a voluntary musculature, and can be controlled at will.
The coordination of the two sphincter muscles allows the anal orifice to open and close, depending on functional needs.
Why is the anal orifice so sensitive?
The anal orifice is a particularly delicate and sensitive part of the body.
And this is because its entire wall, which then flows into the anal canal, or the area of skin surrounding it (peri-anal area) is greatly innervated.
This means that the whole area, besides being highly vascularized (thanks to the hemorrhoidal plexuses) is branched with nerve endings, which are also well nourished by the Vasa vasorum of the arterioles.
Here, then, the anus is particularly sensitive to pain, temperature, and also, of course, surface tactile stimulation.
This sensitivity ends at the junction of the anal canal with the rectum, in that well-defined area called the pectinate line.
Beyond that area, nerve receptors are absent, and thus are internally insensitive to all the rest of the intestine.
High sensitivity makes the anus one of the body's erogenous zones, and in fact for millennia this delicate part has also been used, according to personal preference, for sexual activities.
Anal innervation and sensitivity is equal in both men and women, and therefore sexual use of this body part can occur regardless of gender.
The anal mucosa, similarly to the other mucous membranes of the body and in contrast to the skin, is not endowed with epithelial tissue, hence epidermis proper.
This means that, lacking the corneosurface layer, it is more delicate and sensitive to both chemical and microbialagents.
To defend itself, therefore, the anorectal mucosa constantly produces mucus, which originates from the appropriate mucipar glands in it.
Mucus, combined with the presence of the intestinal microbiota (the 'good' bacteria that live in our intestines and help us complete digestion) protects the mucosa, and this protective system must imperatively be preserved and protected.
The habit that many anal-loving people have (both heterosexuals and homosexuals) of providing anal canal cleansing, by means of a preventive enema, performed before every anal intercourse is harmful and therefore not recommended.
Doing so removes the natural mucus layer from the anal canal, thus increasing the risk of injury, irritation and infection.
Anal penetration and sexual activity using the anus

Although it is physiologically developed for the expulsion of feces, the large presence of nerve endings in the anus and orifice has meant that, since time immemorial, the area has also been used by humans as an erogenous point, and thus included in sexual activities.
Anal penetration, performed indifferently by a man on another man or by a man on a woman, is a common sexual practice throughout history, although in some cultures (depending also on the historical period of reference) it has been socially opposed, while in other cultures tolerated or even exalted.
In men, anal penetration is not only judged pleasurable because of the stimulation of the nerve endings of the orifice and anal canal, but also because it often goes to stimulate an important anatomical part in the male reproductive system, namely the prostate.
In women, anal penetration is often perceived as a direct extension of clitoral activity because the proximity of nerve endings is very short, and the nerves therefore can pass the signal to each other by contiguous diffusion.
However, the anal orifice and anal canal are not anatomically well prepared for penetration as, for example, the female vagina and vaginal canal are.
In addition to the structure of the anal mucosa, which is particularly sensitive and delicate (much more delicate than the vaginal mucosa), the main problem is the lack of adequate natural lubrication, something solved, in women, by vaginal fluid.
Although the anal mucosa, thanks to dedicated glands, produces a certain amount of mucus (necessary for stool to flow well during evacuation), it is still not comparable in quantity and quality of lubrication to vaginal fluid.
That is why, usually, before and during anal penetrative activity there is a need for external lubrication, performed with specific oils or, modernly, dedicated lubricating liquids.
Most cases of post-anal pain result from inflammation of the anorectal mucosa and micro-lacerations of the same, which, in healthy patients, usually resolve spontaneously within a few days.
However, given that mucosal inflammation can recall other inflammation, it is important to adequately potrect the regenerating tissues, thus promoting healing.
This is why, after anal intercourse, it is advisable to wash withlukewarm water and a mild detergent (without perfume or soap), cleaning only the anal orifice and peri-anal area, and without attempting to clean the anal canal more internally.
Enema or pressure rinses should be avoided, and any redness or discomfort can be combated with specific soothing calendula or hyaluronic acid creams, which any Proctologist or pharmacist well trained in Proctology can prescribe or recommend.
Cortisone ointments or anesthetic ointments, commonly available in pharmacies, should be avoided unless prescribed by a physician and closely monitored, and of course other traumatic dealings with the anus should be avoided until fully healed.
Should pain and discomfort persist about a week after anal intercourse, proctological examination is absolutely necessary.
Micro-injuries during anal activity: are they dangerous?
The anal orifice is covered by peri-anal skin, which seamlessly becomes mucous about one centimeter from the external attachment.
The mucosa, unlike the skin, is a special skin: in fact, it does not possess epithelium, that is, the outer stratum corneum (the epidermis).
This causes the mucosa to lack the natural surface protection provided by the epidermis, and is therefore much, much more delicate.
The anorectal mucosa is in fact particularly sensitive to mechanical stresses, to acids that are normally well tolerated by the skin, and its healing capacity, if injured, is the slowest of all skin.
Again, the lack of the stratum corneum makes the mucosa particularly vulnerable to infection, whether bacterial, viral, or even fungal.
This weakness is also made worse by another inherent feature of all intestinal tissue: its high absorptive capacity.
In fact, the main function of the colon is to reabsorb liquids and electrolytes not absorbed in the small intestine, thus turning them into feces.
The intestinal mucosa is therefore itself extremely permeable, and naturally prone to absorption.
This facilitates microbial infections, which therefore often have carte blanche to penetrate it and initiate inflammatory processes, giving rise to anitis (inflammation of the anus) or proctitis (inflammation of the anus and rectum).
These inflammations are often triggered precisely by mucosal lesions, even small or very small ones.
During anal intercourse, even when well lubricated, the mechanical trauma of penetration almost always generates micro-injuries in the mucosa that, albeit in a small number of cases, can give rise to true inflammation, thus initiating anitis or proctitis.
Sometimes, especially if there is insufficient lubrication, these lesions can even be larger, becoming real wounds that, if not treated properly, can become chronic in true fissures.
Continuous anal stimulation of penetration can then, although over the long term, lead to a steady increase in intra-abdominal pressure, which can be the trigger for hemorrhoid prolapse.
Anal intercourse is always a trauma to the mucosa, even when performed well lubricated, and, like any other trauma, can lead to damage to a mucus gland, which can result in an anal abscess and subsequent fistula.
Thus, anal intercourse itself is not dangerous, but the possibility of it generating, due to the inevitable mechanical pressure involved, damage to the anal mucosa is unfortunately not avoidable.
Even taking all possible precautions.
Why do I have pain in my anus after intercourse?

Post-penetration anal pain is physiological, especially in individuals who have recently approached this type of sexual practice.
Pain can be essentially due to two causes:
- An exhaustion, albeit reversible, of the sphincter muscles due to the penetrative act;
- One or more lesions that occurred during the act in the anorectal mucosa
Sometimes, pain may be accompanied by burning, itching, pinpricks, and extreme heat sensation in the anal orifice.
This is often an indication of inflammation of the anal and peri-anal area, which is called anitis.
Sometimes, lesions from the sexual act can go even beyond the combed line, and give rise to proctitis, which is inflammation not only of the anus, but also of the rectum.
Usually, in small lesions that are not serious, the inflammation resolves spontaneously in a few days, but sometimes it persists, giving rise to chronic proctitis.
If the injury that occurred during anal intercourse is substantial, the pain is accompanied not only by general burning and discomfort, but also by bleeding, especially during evacuation.
Blood in the stool or on the toilet paper (called hematochezia in medical circles), usually bright red in color, is the obvious symptom of a lesion in the anus or rectum, and if this occurs after sexual intercourse its origin is consequent to the same.
Anal penetration should always be accompanied by appropriate lubrication, ideally maintained throughout the duration of intercourse.
The duration of it should also be proportionate and not excessive, so as not to exhaust the sphincter muscles and increase the likelihood of injury to the anal mucosa.
Serious cases of injury to the delicate anal mucosa occurring during intercourse are almost always attributable to poor lubrication, often accompanied by excessive duration of intercourse.
How can I ease the pain after anal intercourse?

Most cases of pain after anal intercourse resolve spontaneously within a few days.
It takes about 48 hours for the sphincter muscles to dispose of the stress they had with intercourse (and, in the case of the external sphincter, also dispose of the lactic acid produced), while in the case of micro-injuries to the mucosa, they are repaired after a few days.
Thus, therapy is supportive, and is based on the appropriate cleaning of the anal and perianal area with gentle cleanser (there are many commercially available soap-free, nonirritating ones), adequate rest, and the emission of soft, well-formed stools.
In case of excessive burning, you can also use various soothing creams (calendula and propolis creams are excellent), which are meant to relieve inflammation and protect the mucosa while it repairs itself.
Obviously, during recovery it is imperative not to proceed with any other anal sexual activity.
Only a small proportion of post anal inflammation requires more vigorous treatment, but this should only be proposed by the proctologist after the appropriate proctological examination.
In case of anal bleeding, whether light or copious, it is always imperative to see the Proctologist for evaluation of the extent and consistency of lesions to the anorectal canal.
Proctologically pathological patients, such as those suffering from prolapsed hemorrhoids or anal fissures, should refrain from anal intercourse.
Any strain on the diseased mucosa increases the risk of even greater tearing, bleeding, and, insubstantially, worsening the situation.
In the case of proctitis, anitis, the aforementioned pathological hemorrhoidsor anal fissures, it is imperative that the anorectal mucosa not be subjected to excessive tearing or stimulation, and therefore anal sex should be avoided until completely healed (possibly, after medical endorsement).
The pain after anal intercourse did not go away after many days, in fact it got worse, why?
Although the majority of small lesions to the anorectal canal following sexual intercourse resolve spontaneously, a small proportion statistically need specific medical treatment.
When this happens, it is almost always because one or more lesions fail to heal properly, thus generating one or more anal fissures.
In Proctology, anal fissure is defined as a wound of the anorectal canal that does not heal spontaneously after about 6 weeks.
This lack of healing may be dependent on many factors, including a hypertonus of the internal sphincter muscle, with continuous spasms (urged by the fissure itself) worsening the vasculature and thus preventing healing.
In other cases, anal intercourse has torn the hemorrhoidal plexuses, resulting in their congestion and the onset of their prolapse (reversible or not), sometimes reported as painful, especially if adjacent to the anal orifice.
The trauma of penetration can then cause, especially in patients already pathological with hemorrhoids, the onset of a hemorrhoidal thrombus, which is often extremely painful.
Although statistically rare, there is also the risk of the development of an anal abscess, due to damage to a mucus gland traumatized by sexual intercourse.
In this case, the pain for the patient increases day by day until it becomes unbearable, so much so that he or she has to seek emergency proctological care.
This, it should be made clear, is a fortunately rare event, but still possible.
Given, therefore, that the cause of persistent pain after anal intercourse can vary greatly, it is always recommended that the patient, after a certain number of days, contact a Proctologist for a mandatory specialized proctological examination.
In contrast to the upper part of the rectum, that is, after what is called the pectinate line (or serrated line), the anal canal is richly innervated.
This large amount of nerve endings makes it very sensitive: to cold, heat and pain.
This is why the anus is considered, not unlike the sex organs, an erogenous zone, which is often and frequently stimulated during the sexual act (not only by people with homosexual preferences).
In men, such sensory stimulation is enhanced by an anatomical component not present in women: the prostate.
This organ, which is essential for producing the adequate sperm fluid where sperm will 'swim', can be stimulated by penetration through the penis or its surrogate, and this can generate pleasure in men, to the point of causing them to orgasm.
This is why the act of anal sex is not exclusive to homosexual people, but is often practiced by heterosexual couples as well, through the activity called pegging.
However, pegging is actual penetration, and as such it can be dangerous to the integrity of the anorectal mucosa, especially if practiced with little lubricant and with oversized dildos or strap-ons.
Do you have pain in the anus after sexual intercourse, and it hasn't gone away for several days? Dr. Troyer can help you
Dr. Luisella Troyer is a Proctologic Surgeon with years of experience in affections of the anus and rectum.
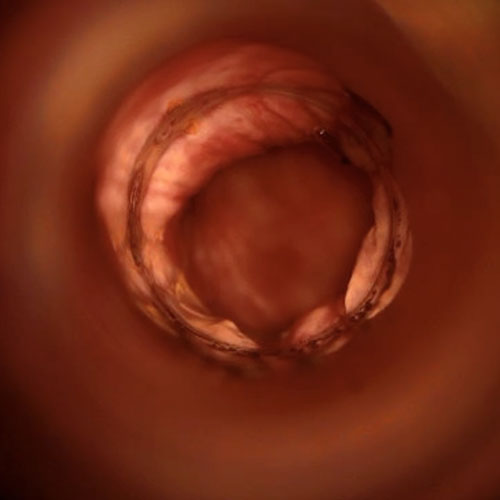
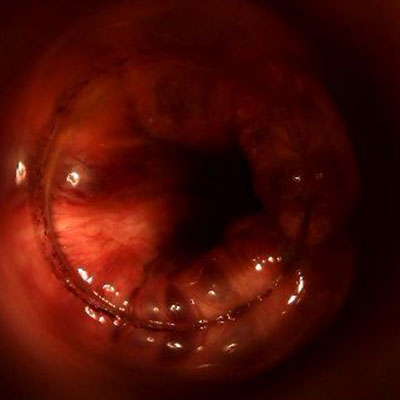
In her clinic in Dubai, Dr. Troyer can help you understand the origin of anal pain after sexual intercourse, and she can investigate thoroughly and accurately in the anorectal canal with her Electronic Endoscopic Videoproctoscopy examination.
To get well, without more pain.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- THE ANAL ORIFICE IS THE VERY LAST PART OF THE INTESTINE, SERVING AS AN OPENING FOR THE PASSAGE AND DISCHARGE OF FECES;
- THE SKIN OF THE PERIANAL AREA BECOMES, ABOUT ONE CENTIMETER AFTER ENTERING THE ORIFICE, ANAL MUCOSA;
- THE ANAL MUCOSA IS DELICATE BECAUSE IT TOTALLY LACKS THE PROTECTION OF THEEPIDERMIS;
- ACIDIFIED FECES, TOO HARD OR ANY MECHANICAL TRAUMA CAN INJURE THE DELICATE ANAL MUCOSA, CAUSING TEARING AND INFLAMMATION;
- ANAL PENETRATION IS AN ANCIENT SEXUAL PRACTICE, PRACTICED NOWADAYS BY BOTH HOMOSEXUAL PEOPLE AND HETEROSEXUAL COUPLES;
- EVERY ANAL PENETRATION CREATES MICRO-INJURIES IN THE ANAL MUCOSA, WHICH CAN BE MORE OR LESS SEVERE DEPENDING ON THE DURATION OF INTERCOURSE AND ITS LUBRICATION;
- THE USE OF LATEX CONDOMS CAN ALSO CAUSE ALLERGIC IRRITATION AND, AS A RESULT, ANITIS AND ANAL BURNING;
- PEGGING IS A SEXUAL PRACTICE WHERE THE WOMAN, WITH THE HELP OF PENIS SURROGATES (CALLED DILDOS OR STRAP-ONS), PENETRATES THE MAN BY STIMULATING THE PROSTATE;
- THE USE OF SEX TOYS AND THE PRACTICE OF PEGGING GREATLY INCREASES THE RISK OF MAJOR TEARING OF THE ANAL MUCOSA, ESPECIALLY IF IT HAS NOT BEEN WELL LUBRICATED;
- POST-PENETRATIVE SEXUAL INTERCOURSE ANAL PAIN RESULTS FROM SPHINCTER MUSCLE SORENESS AND MICRO-INJURIES THAT INFLAME THE ANAL MUCOSA;
- MICRO-INJURIES DURING ANAL INTERCOURSE INCREASE THE RISK OF BACTERIAL AND VIRAL INFECTIONS;
- AFTER ANAL INTERCOURSE IT IS NECESSARY TO ALLOW THE MUCOSA TO REST, CLEANSING IT WITH APPROPRIATE PRODUCTS AND, IF NECESSARY, RELIEVING INFLAMMATION GENTLE CLEANSERS AND THE USE OF APPROPRIATE, SOOTHING CREAMS;
- IF SIGNIFICANT LESIONS HAVE FORMED DURING ANAL INTERCOURSE, THERE IS A POSSIBILITY OF BLEEDING DURING EVACUATION;
- IF PAIN AFTER ANAL INTERCOURSE PERSISTS BEYOND A FEW DAYS, ONE SHOULD NECESSARILY CONSULT A PROCTOLOGIST;
- ONE SHOULD NOT OVERDO ANAL SEX, AS ONE MUST GIVE TIME FOR THE MUCOSA TO HEAL;
- BEFORE ANAL INTERCOURSE, ONE SHOULD NEVER GIVE ENEMAS OR WASH THE ANAL CANAL, AS DOING SO REMOVES THE NATURAL PROTECTIVE LAYER OF MUCUS, THUS INCREASING THE RISK OF INJURY AND INFECTION;
- CONTINUED ANAL INTERCOURSE OVER TIME, ESPECIALLY IF ASSIDUOUS, CAN LEAD TO THE ONSET OF EVEN SERIOUS DISEASES, SUCH AS SPHINCTER EXHAUSTION, PATHOLOGICAL HEMORRHOIDS AND ANAL ABSCESS

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.

















