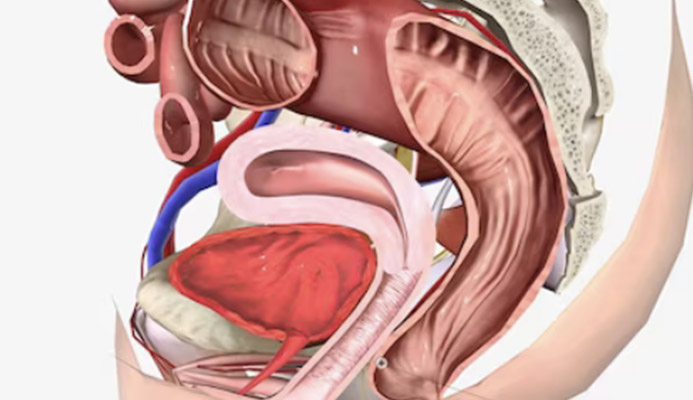
The pelvic floor is all that structure of muscles, ligaments and connective tissue that, just as the name suggests, acts as the ‚Äėfloor‚Äô of our pelvis, essentially enclosing the abdominal-pelvic cavity.
It is a fundamental area of the body, as it encloses and supports organs that are essential to life, such as the urethra, bladder, vagina (or prostate) and the entire anorectal duct.
Although few people know about the pelvic floor, and its importance has only recently been rediscovered by medicine, there are a large number of problems that a pathological condition of its tissues can cause, not only for women but also for men.
These problems can range from the inability to have satisfying sexual intercourse to actual faecal and urinary incontinence, and even chronic constipation.
For these problems, rehabilitation medicine has long since developed various techniques that, as the name implies, aim to rehabilitate the pelvic floor and restore well-being and a goodquality of life to patients.
Read this page to find out all about Dr Luisella Troyer's pelvic floor rehabilitation.
Like all prolapses due to failure of supporting structures, pelvic floor prolapse, if not properly treated, may not improve but only worsen.
That is why diagnosis and possible rehabilitation therapyshouldbe carried out as soon as possible.
Pelvic rehabilitation gives the best results, in fact, in the early stages of prolapse.
WHAT IS THE PELVIC FLOOR?
In anatomy, the pelvic floor refers to the roughly rhomboid area that roughly connects the two ischial tuberosities of the hips.
Anatomically, the pelvic floor can be briefly schematised into three major zones:
- The pelvic diaphragm zone;
- The urogenital diagram zone;
- The zone surrounding the sphincters
The zone of the pelvic floor, which is¬†not protected by the skeleton, is composed of¬†muscles,¬†tendons¬†and¬†connective tissue, joined together in a true¬†‘floor’,¬†on which¬†all the organs of the lower abdomen and pelvis, such as the¬†rectum,anus,¬†bladder,¬†urethra¬†and, of course, the¬†sexual organs, rest.
WHY IS THE PELVIC FLOOR SO IMPORTANT IN HUMAN ANATOMY?
The pelvic floor is of fundamental importance to the body, both male and female, as its tissues support internal organs of considerable physiological as well as reproductive importance.
A major failure of the structure always leads to serious and disabling problems with defecation, urination, and sexual intercourse, significantly impacting quality of life.
The importance of the pelvic floor and all that it supports was ignored by medicine for a long time, and only in more recent times has its fundamental usefulness finally been rediscovered.
WHEN THE PELVIC FLOOR GIVES WAY: FROM PERINEUM DESCENT AND PELVIC ORGAN PROLAPSE
The pelvic floor is a¬†strong but elastic¬†structure that, with the appropriate tendon and muscle¬†‘hooks’, supports itself every day, constantly defying¬†gravity.
This daily effort can be made even more onerous by particular situations and conditions, and has a tendency to worsen over the years, due to the well-knownslowdown in metabolism which, in turn, decreases the quantity and quality of collagen.
There are essentially two main disorders of the pelvic floor: what is called descending perineum syndrome and prolapse of the pelvic organs.
A descending perineum is when the pelvic floor gives way in its elasticity and tone, in fact prolapsing downwards.
Usually, this descent worsens during abdominal straining, such as during defecation (pushing to expel faeces), urination, or during work or sports exertion.
On a clinical level, the descent of the perineum is considered pathological when it exceeds more than 1.4 cm of the anorectal angle in relation to the iliac tuberosities, under resting conditions (i.e. not under strain from urination or straining).
Pelvic organ prolapse , on the other hand, is, as the name implies, the systematic descent and exit of the anatomical structures of theuterus, vagina, bladder and anorectal canal.
Both the descending perineum syndrome and the actual prolapse of the pelvic organs can be present and mild, and thus remain asymptomatic, or become symptomatic, and bring many dysfunctions to the patient, some of them severe and capable of considerably worsening the quality of life.
WHY DOES THE PELVIC FLOOR PROLAPSE?
Essentially, pelvic floor tissues are able to be elastic and strong because of the large amount of collagen present in them.
Collagen¬†is the protein that, as the name suggests,¬†‘glues’¬†tissues together and allows them to¬†adhere, both to¬†bony structures¬†and to other¬†soft tissues.
This fundamental glue is produced by fibroblasts, i.e. special connective tissue cells that have the very job of constantly producing new collagen.
The reason for this continuous production is quickly stated: just like any other¬†‘glue’,¬†collagen, too,¬†loses its initial characteristics¬†over time, to become¬†‘drier’¬†and less functional.
This is why, cyclically, old collagen is disposed of by macrophages and replaced with new collagen.
This process, which is called collagen turnover, is indispensable to our bodies for a multitude of things: to keep the skinfirmly attached to the panniculus adiposus and the muscular tonaca, to keep the connective tissue toned and elastic, and, in turn, to allow the tissues of the pelvic floor to continue to be elastic and strong.
Unfortunately, with age, the metabolism of collagen production declines, and turnover slows.
By slowing down the renewal of collagen, collagen remains in the tissues longer, even when it has become dry and non-functional, thus causing a loss of tissue tone and strength.
This is of fundamental importance not only for our skin (which in fact begins to¬†‘fall off’,¬†forming¬†wrinkles), but also for the tissues which, like those of the pelvic floor,¬†must necessarily remain tight and toned.
To this main cause, one must then add the so-called triggering factors, i.e. events that worsen the sagging of the pelvic floor and indeed often cause itsonset.
Such triggering factors are:
- Chronic constipation;
- Pregnancy and childbirth specifically;
- Obesity
Like all prolapses due to failure of the supporting structures, pelvic floor prolapse, if not properly treated, may not improve but only worsen.
This is why the diagnosis and possible rehabilitation therapy should be carried out as soon as possible.
Pelvic rehabilitation gives the best results, in fact, in the early stages of prolapse.
WHAT SYMPTOMS CAN A PROLAPSED PELVIC FLOOR GIVE?
The symptomatology of descending perineum and pelvic floor prolapse is extremely complex and varied: it ranges from the absence of symptoms to very significant complaints, which severely aggravate the subject's quality of life.
It should be remembered that prolapses of less than one and a half centimetres are usually considered physiological in women already giving birth and over 50 years of age, and usually remain asymptomatic, thus not requiring treatment.
Having said that, here are the most common symptoms of a prolapsed prolapse:
Obstructed defecation or faecal incontinence
As it slides downwards, the pelvic floor also carries the anorectal canal, resting on it.
This can lead to deformation of the rectum and, especially in women, the formation of a rectocele.
This deformation can lead to difficulty in defecation or faecal incontinence, as the sphincters and the relaxation of the anorectal connective tissues arealso affectedby the general wear and tear of the pelvic floor;
Problems with urination and urinary incontinence
Lowering of the pelvic floor also leads to a prolapse of the bladder, which can then give rise to a cystocele.
The problems of such prolapse range from difficulty urinating to actual urinary incontinence;
Erectile problems
By sliding downwards, the bladder tends to crush the prostate, which instead always seems to maintain its anatomical position, thus causing prostatitis.
Chronic prostatitis therefore leads to erectile dysfunction in men;
Difficulties in sexual intercourse for women
By sliding down, the rectum can press on the vagina, thus generating hyper-sensitivity and the consequent difficulty (or impossibility) of thepenetrative sexual act.
These symptoms, it must be remembered, must be taken as a generic outline: they may occur in combination or individually, and their intensity and discomfort for the patient may vary greatly, depending on the degree of prolapseand, no less important, on any restraining therapies that may be in place.
WHAT IS THE DIAGNOSIS OF PELVIC FLOOR PROLAPSE?
The diagnosis of perineum descent and pelvic floor prolapse is made by proctological examination with mandatory pelvic examination.
In addition to the clinical examination, the doctor may also prescribe other specialist examinations, including:
- A video-procedure;
- An anorectal manometry;
- An ultrasound of the pelvis and bladder;
- Uroflowmetry;
- An MRI of the pelvis;
- A defecography
WHAT IS PELVIC REHABILITATION?
Pelvic floor rehabilitation is that whole series of medical and physiotherapeutic treatments that have two main purposes:
- To increase the tone and elasticity of the pelvic floor tissues
- To reduce or eliminate symptoms for the patient
These treatments are essentially divided into four separate sub-therapies that, however, must be integrated into a protocol decided upon by the physician, also taking into account the state of the prolapse and the patient's symptoms.
These therapies are:
- Physiokinesitherapy, i.e. physiokinetic gymnastics to rehabilitate the pelvic floor on a sensory and motor level;
- Electrotherapy, to increase the tone of the pelvic muscles (essential in cases of sphincter hypotonia or urinary incontinence);
- Appropriate dietary and bowel rehabilitation therapy, to ensure soft, well-formed and easy bowel movement;
- Biofeedback therapy, to make the patient regain the appropriate stimuli for urination and defecation
All these therapies make uppackages of protocols that arenecessarily customised, i.e., designed by the doctor in an appropriate amount according to the patient's situation.
If well implemented, pelvic floor rehabilitation therapy can greatly improve a patient's condition, halting prolapse and relieving or minimising symptoms, thus increasing quality of life and return to normal activities, without the fear of faecal or urinary incontinence.
It must be remembered that the best results of pelvic rehabilitation are obtained when it acts on the early stages of prolapse of the perineum.
Therefore, early diagnosis and initiation of the rehabilitation protocol are absolutely essential to achieve the best possible results.
WHEN IS PELVIC FLOOR SURGERY NECESSARY?
Surgery for the resolution of prolapse of the perineum is relegated, with modern protocols, only to severe cases, which are not affected by the rehabilitation treatment.
This is the case when there is a total tissue laceration or complete muscle and tendon exhaustion, which cannot be resolved with rehabilitative physiotherapy.
For example, surgery proves necessary in the case of a perforated rectocele, or severe cystocele.
It must be remembered, however, that even in the case of a surgical indication, pelvic rehabilitation is always necessary, both before and after the operation.
DO YOU SUFFER FROM FAECAL OR URINARY INCONTINENCE AND WANT TO IMPROVE YOUR SITUATION? DR. LUISELLA TROYER CAN HELP YOU

Dr Luisella Troyer is a Vascular Surgeon specialised as a Proctologist, with great experience in the diagnosis and treatment of the descending perineum.
In her clinic in Dubai she can help you diagnose and treat the most disabling symptoms of descending perineum, such as faecal or urinary incontinence.
A dedicated team of physiotherapists, nurses and massage therapists, personally selected and coordinated by the Doctor, can help you return to a state of well-being, thanks to advanced intestinal and pelvic rehabilitation protocols.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- THE PELVIC FLOOR IS THAT ANATOMICAL AREA BETWEEN THE TWO HIPS THAT SUPPORTS ALLPELVIC ORGANS, SUCH AS THE URETHRA, BLADDER, ANUS, AND RECTUM;
- GIVEN THAT HUMAN BEINGS, FOR EVOLUTIONARY REASONS, DO NOT HAVE A BONY STRUCTURE TO SUPPORT THE PELVISES, THE TASK IS PERFORMED BY A COMPLEX 'FLOOR' CONSISTING OF TENDONS, MUSCLES AND CONNECTIVE TISSUE;
- THE PELVIC FLOOR IS AN ELASTIC AND TONED STRUCTURE THAT IS FLEXIBLE BUT RESILIENT;
- THE FLEXIBILITY AND ELASTICITY OF THE PELVIC FLOOR ALLOWS THE HUMAN BODY TO MOVE FREELY WHILE SUPPORTINGTHE PELVIC ORGANS;
- THE TONICITY AND STRENGTH OF PELVIC FLOOR TISSUES ARE MAINLY GIVEN BY THE AMOUNT OF COLLAGEN IN THEM;
- OVER TIME, SLOWER METABOLISM ALSO RESULTS IN LOWER COLLAGEN TURNOVER;
- CERTAIN TRIGGERS SUCH AS PREGNANCY AND CHILDBIRTH CAN FURTHER WEAKEN PELVIC FLOOR TISSUES, WORSENING OR INITIATING ITS PROLAPSE;
- ALTHOUGH PELVIC FLOOR PROLAPSE CAN ALSO AFFLICT MEN, IT IS WOMEN WHO ARE MOST AFFECTED;
- FOR PARTURIENT WOMEN OVER AGE 50, A SLIGHT DEGREE OF DESCENT OF THE PERINEUM IS CONSIDERED PHYSIOLOGIC, AND NOT ALWAYS IN NEED OF TREATMENT;
- THERAPY FOR DESCENDING PERINEUM SYNDROME IS PRIMARILY PHYSICAL, AND IS BASED ON REHABILITATION PROTOCOLS;
- PHYSIOKINESITHERAPY,ELECTROSTIMULATION, BIOFEEDBACK, AND APPROPRIATE BOWEL REHABILITATION ARE COMBINED IN A REHABILITATION PROTOCOL THAT CAN MINIMIZE OR REDUCE THE SYMPTOMS OF PELVIC FLOOR PROLAPSE;
- SURGERY FOR PELVIC FLOOR REPOSITIONING IS RESERVED ONLY FOR SEVERE CASES IN WHICH THERE IS A TISSUE TEAR AND WHICH DO NOT RESPOND TO REHABILITATION THERAPY;
- ONE SHOULD DIAGNOSE AND INTERVENE AS EARLY AS POSSIBLE IN CASES OF PELVIC PROLAPSE, AS THE BEST REHABILITATION RESULTS ARE OBTAINED IN THE EARLY STAGES

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.