Do you often suffer from violent attacks of bowel, leading to periods of actual diarrhea, alternating with periods instead of constipation?
Do you notice that bowel activity travels in parallel with your state of anxiety, your stress level, your problems at work, or your family quarrels?
Irritable bowel syndrome is a condition that affects a huge amount of people every year, and has therefore often been called 'the new modern disease' of the gut, although its origins are also known in the past.
Read this page to find out what irritable bowel syndrome is: what it originates from, how it can be diagnosed, and how it can be treated.
What is irritable bowel syndrome?
In Medicine, irritable bowel syndrome is a gastrointestinal dysfunction, with symptoms that can vary greatly from patient to patient, but still has definite effects on normal bowel physiology and regular daily defecation.
Also often called spastic colitis or dystonic colitis, it manifests as a series of concatenated gastrointestinal symptoms, which have the characteristic of being intermittent in the long run, with periods of remission and others instead of violent recrudescence.
Given that, this particular intestinal pathological condition has a wide variety of symptoms but the etiology is still uncertain, the term 'syndrome' rather than 'disease' is used.
What are the symptoms of irritable bowel syndrome?
Irritable bowel syndrome is well known in medical circles to have a very large number of symptoms, not all present in every patient, not all manifested at the same time, not all of the same severity.
After all, the origin of the pathology, although still uncertain, is strongly suspected to be psychosomatic in nature, and if this is correct, the wide variety of symptoms, which changes from patient to patient, is also understandable.
That being said, the symptoms most commonly present in patients with irritable bowel syndrome are:
- Alteration of stool, with periods of true diarrhea alternating instead with periods of constipation;
- Bowel pain, spasms, and cramps, either related to defecation or sometimes occurring spontaneously, often in conjunction with major events or high-stress situations;
- Depression and social isolation due to not knowing if and when a new bowel attack will happen, often judged by the patient to be unpredictable;
- Onset and exacerbation of symptoms in conjunction with events or situations of some importance, such as a new job, a new relationship, a vacation, a school exam, any event that is perceived as potentially important (not exclusively in a negative sense);
- Sleep disturbance and easy irritability, often due to uncertainty about bowel situation
As you can well see, then, IBS is composed of a varied set of symptoms, and not all of them can be manifested during a bowel crisis.
On the concept of 'intestinal crisis' then, a separate discussion must be opened.
All patients suffering from IBS, in fact, are not perpetually 'sick'.
Their intestinal health status is highly variable and difficult to predict: they go from absolutely normal situations to real 'bowel crises', often extremely violent, which can last for several days or several weeks.
Almost always, these crises occur shortly before or immediately after events deemed important or dramatic, and this supports the hypothesis of the psychosomatic origin of the pathology.
Are there symptoms of other diseases related to IBS?
Yes, like any other defecation alteration, irritable bowel syndrome, in the long run, brings with it a whole range of related proctologic conditions.
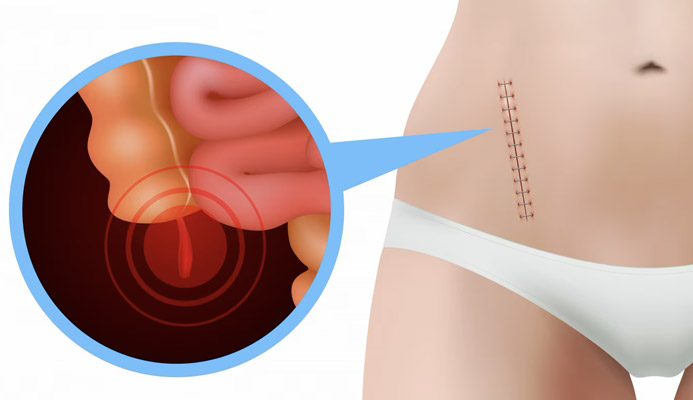
Continuous periods of diarrhea alternating with periods of constipation often cause increased intraabdominal pressure, leading to subsequent damage to the anorectal canal.
Pathological hemorrhoids are a very common problem for long-term patients with irritable bowel syndrome, just as they are well acquainted with conditions of proctitis and anitis, the result of the tearing and inflammation of the mucosa following violent diarrheal attacks.
The formation of fissures (always due to mucosal tears caused by stypsic or diarrheal alvo), nonetheless prolapse of the rectum, should also not be ruled out.
Although the exact etiology of IBS is not yet known, its connection with neural activity and its deep interconnection with the patient's psychological well-being are now established arguments.
It is no accident that diarrheal attacks or otherwise intestinal problems of patients with IBS often occur close to critical or important work, emotional or otherwise psychological situations.
A new job, a problem at work, a sentimental shock, problems with a partner or companion, in short: any situation of non-normality, which causes stress and anxiety, is often enough to trigger an attack.
The explanation for the phenomenon has already been surmised and, although still not complete, may help in its understanding: when we become agitated, to 'calm down' our brain produces large amounts of cortisol, a relaxing hormone.
However, this molecule, although it has the property of calming us, has a nefarious effect on the colon mucosa: it irritates it, as well as damages the intestinal flora.
The result is a diarrheal crisis, or at any rate pesudo-grastroenteritis.
A very common phenomenon in patients with irritable bowel syndrome.
When does irritable bowel syndrome occur?
Irritable bowel syndrome usually begins to manifest during youth.
In fact, cases of very young, adolescent patients already experiencing the first symptoms of spastic colitis syndrome are not uncommon.
Sometimes, and not uncommonly, these symptoms begin even before adolescence, that is, in the pediatric stage.
All of this supports the hypothesis that the pathology is psychosomatic, and that it is an unconscious response of the body to external stimuli and impulses common even in childhood.
What are the real causes of irritable bowel disease?
IBS does not yet have a definite and certain origin.
The main hypothesis to dysfunction is that of psychosomatic origin, with particular regard toward visceral hypersensitivity and stressful conditions (not only in conjunction with perceived negative events).
After all, the deep connection between brain and gut activity has long been established, although the actual physiological mechanism is still not entirely clear.
It has also been found that particular dietary regimens can worsen the condition of the IBS patient.
This suggests that, however, upstream there is a natural predisposition and some intestinal sensitivity, which worsens and sharpens under given psychological impulses.
How is irritable bowel syndrome diagnosed?
The diagnosis of IBS is clinical, in which an extremely important role is played by the medical history.
Often, it is precisely during the history taking that the physician is put on the right diagnostic path by listening carefully to the patient's medical history, which usually reports complaints and dysfunctionality typical of IBS as early as a young age.
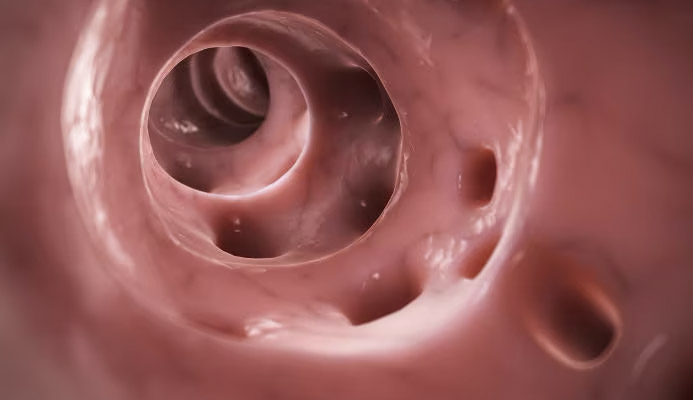
The examination then continues with a clinical abdominal examination where, in most cases, the physician can accept the presence of a colic string, significant colonic stiffening, and the presence of aerophagy.
The examination is concluded with the Electronic Endoscopic Videoproscopy examination, where the Proctology Physician proceeds to analyze the anorectal canal to highlight any related pathologies such as pathological hemorrhoids, fissures, an anitis or proctitis situation.
If necessary, the physician may also prescribe to accompany other specialized evaluation tests, such as colonoscopy or a complete blood count, essentially to rule out the presence of other autoimmune diseases that might have similar symptoms, such as Crohn's disease and ulcerative rectocolitis.
Until 1622, the actual function of the colon was obscure to the Medicine of the time.
It was thought, generically, that the last part of the intestine that we now call precisely the colon (once called by the old name of large intestine) was devoted to the processing of feces, but its real and primary function as a fluid reabsorbing organ was not known.
And this was because the lymph cycle, with the whole fundamental system of lymphatic vessels, was not known to Medicine.
It was the Cremonese Surgeon Gaspare Aselli, together with his most trusted pupils, who first discovered the existence of an incredibly branched network of very thin vessels (the chyliferous vessels) that permeated the entire small intestine, and whose task was precisely the absorption of fat from the chyme (the nutrient-rich food absorbed by the intestinal villi).
This revolutionary discovery initiated Lymphology, that branch of Vascular Surgery that deals with the study and treatment of the lymphatic system and lymphatic pathways.
Is there an effective treatment for irritable bowel syndrome?
Given that the exact etiology of irritable bowel syndrome is not, at present, known to Medicine, the only suitable therapy to provide relief of symptoms and restore a good quality of life for the patient is dietary-behavioral therapy.
Prescription medication is always to be avoided and should be confined exclusively as palliative support during acute stages, while instead phytotherapeutic medication (such as the excellent extracts of mallow, fennel, chamomile, charcoal, mint oil, etc.), combined with the intake of quality probiotics (milk enzymes) should be preferred.
The diet must also be perfectly tailored to the patient: foods and foods that can irritate the colon even more (especially those capable of fermenting, such as dairy products and dairy derivatives in general) should be avoided, and fiber-rich foods should be preferred instead.
The level of anxiety and stress must also be controlled and kept within acceptable limits, resorting if necessary also to the help of a professional Psychologist.
In general, the patient's anxious state should be kept low, and at the same time the bowel should be helped to return (and maintain) normal activity.
However, this can take time: bowel rehabilitation in IBS cases is a long and sometimes complex journey, and the patient must necessarily be informed of the presumed long duration of treatment.
Which Physician can diagnose and treat IBS?
The Clinical specialist with great experience in IBS is the Proctologist Surgeon.
The Proctologist Surgeon is the Physician who specializes in all diseases of the intestine, rectum and anus, and is the essential health professional to diagnose and plan a suitable protocol of treatment for the patient suffering from IBS.
your proctologist surgeon of excellence in Dubai
Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- IRRITABLE BOWEL SYNDROME IS A SET OF SYMPTOMS THAT LEAD TO FREQUENT DYSFUNCTION OF THE BOWEL;
- THE ORIGIN OF IBS IS NOT YET KNOWN TO SCIENCE, BUT IT IS PRESUMED TO BE PSYCHOSOMATIC IN NATURE;
- IRRITABLE BOWEL SYNDROME OCCURS IN CYCLES, WITH PERIODS OF RECURRENCE AND PERIODS INSTEAD OF REMISSION;
- THE SYMPTOMS OF IBS VARY WIDELY FROM PATIENT TO PATIENT, BUT GENERALLY INCLUDE ABDOMINAL SPASMS AND PAIN, DIARRHEA ALTERNATING WITH CONSTIPATION, DEPRESSION, AND EASY IRRITABILITY;
- THE PSYCHOSOMATIC ORIGIN OF IBS MAY REQUIRE PSYCHOTHERAPY INTERVENTION BY A PSYCHOLOGIST;
- TREATMENT OF IRRITABLE BOWEL AIMS TO FLUSH THE BOWEL, AND BRING IT BACK TO NORMAL ACTIVITY;
- THE DIAGNOSIS OF IBS MUST NECESSARILY EXCLUDE OTHER SYMPTOMATICALLY SIMILAR CONDITIONS, SUCH AS ULCERATIVE RECTOCOLITIS OR CROHN'S DISEASE;
- IN THE LONG TERM, BOWEL DISORDERS CAN LEAD TO THE ONSET OF PROCTOLOGIC DISORDERS, SUCH AS PATHOLOGIC HEMORRHOIDS, PROCTITIS ANAL FISSURE

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.