Do you suffer from itchy anus, or notice reddish streaks of blood on the toilet paper?
 
Do you always have the sensation of discomfort in the anal region, with tingling, burning that intensifies when you go to the body?
Inflammation of the mucosa and skin of the anus and perianal area is a very common condition, which in turn is caused by an upstream dysfunction that almost always coincides with an alteration in stool.
 
Read this page written by Dr. Luisella Troyer, Proctology Surgeon, to find out what is what is referred to in medical jargon as anitis or proctitis.
The anorectal mucosa, like the other mucous membranes of the body, is a particularly delicate and sensitive tissue.
This is because, unlike the skin, it does not have a protective stratum corneum (the epidermis).
Here, therefore, the anorectal mucosa is more exposed to attack by microorganisms and chemical aggression, much more so than the skin, and can easily become injured or inflamed, giving rise toanitis or proctitis.
What is the anus, and why does it become irritated?
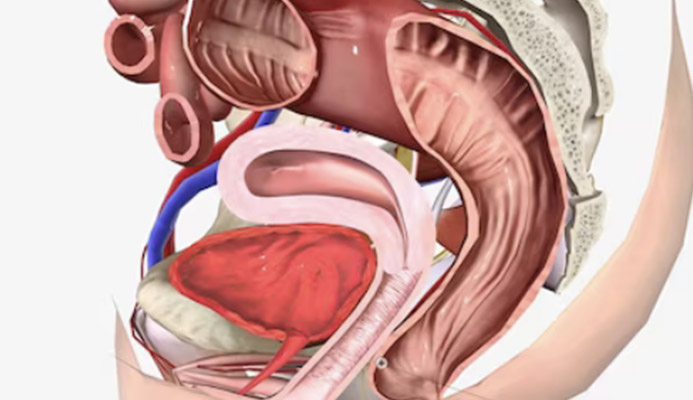
The anus, also called the anal orifice, is the final opening of the gastrodigestive tube, the very last part of the intestine.
Its purpose is well understood and known, and it is to expel fecal waste, including gas produced by intestinal fermentation, out of the body.
The anus is basically a hole, surrounded internally by anal mucosa, which seamlessly then becomes peri-anal skin in a gradual and nuanced transition.
The walls surrounding the anus form the anal canal, which varies in length from person to person but is usually 2-3 cm long.
Beyond this extent, the anus becomes the rectum, that is, the last part of the entire intestine just below the rectal ampulla, where feces are collected before being expelled.
The junction line between anal and rectal canal is called the combed line (or pectinate line), because of the curious vertical pleating of its walls.
The anus and anal canal, as opposed to the rectum, is heavily vascularized and innervated, and this large nerve ending has as its end point precisely the pectinate line, beyond which we are virtually numb.
As the final opening of the intestine, the anus is an extremely elastic structure: its mucosa and peri-anal skin can open and stretch even widely, thus allowing stool to pass through, without pain during evacuation.
The closing and opening of the anus is enabled by two specific, doughnut-shaped muscles called sphincter muscles.
We have two: the internal sphincter, adjacent to the anorectal mucosa, and the external sphincter, which surrounds the internal one.
The internal sphincter is an involuntary muscle, which automatically contracts or relaxes, and tightens or opens the anus according to physiological need, that is, evacuation.
The external sphincter, on the other hand, is a voluntary muscle, which we can freely control and which is useful for holding stool when the situation does not allow us, for example, to defecate at will.
Thus, the anal orifice is the natural outlet of our intestines, and every day it transits feces, that is, the organic wastes of our nourishment, opening or tightening thanks to the sphincters.
This continuous passage of feces is physiological, and does not create problems for the anus, but in certain situations it can become pathological instead, triggering an inflammatory response of the anal mucosa and peri-anal skin.
What is anitis?
In Medicine, 'anitis' refers to inflammation of the anus and peri-anal area.
Such inflammation involves redness, burning, tingling, itching and, if of moderate severity, also swelling of the mucosa and a feeling of heaviness, sometimes even of a foreign body in the anus.
Anitis is a symptom, and not an actual disease: it means that the mucous membrane of the anus or the skin of the peri-anal area has been injured, irritated, or otherwise aggressively attacked by chemical or microbial agents to such an extent that it becomes inflamed and damaged.
Basically, anitis is nothing more than a dermatitis of the anal and peri-anal area, and the symptomatologic features with a common dermatitis that may affect other areas of the body are clearly evident and recognizable.
Anitis can be of two specific types: acute or chronic.
- Acute anitis, as the name implies, occurs in the presence of a single traumatic event that, often suddenly, tears or otherwise irritates the anal wall or peri-anal area.
For example, an episode of constipation, with the evacuation of particularly hard stools, or a diarrheal discharge, with the expulsion of unformed, liquid, acidified stools;
- Chronic anitis, on the other hand, occurs when, for a long series of reasons, the episode that caused the acute anitis does not recur, the anal mucosa and/or skin does not heal, and there is thus the presence of chronic inflammation.
This usually occurs as a result of chronic conditions that have become chronic over time, e.g., in the case of chronic diseases of the colon: irritable bowel syndrome, ulcerative rectocolitis, Crohn's disease, pathological hemorrhoids that have never been treated, anal warts, etc.
In any case, anitis is the natural response of the anal mucosa and skin to an external attack: in an attempt to repair damaged cells, our body sends large amounts of blood to the anal area, giving rise to swelling, while external bacteria, seizing the greedy opportunity of a 'leak' in our external defense (the skin) attack us, giving us pain, burning and all the other symptoms outlined above.
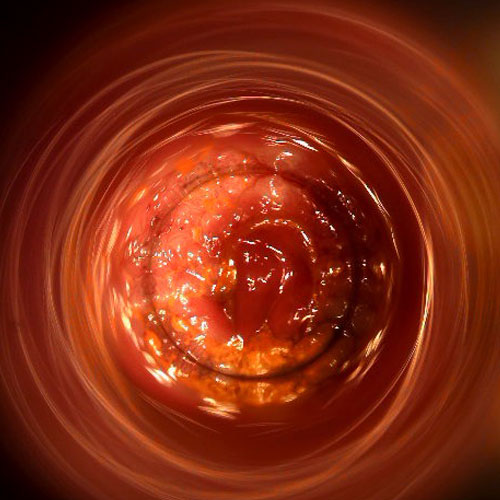
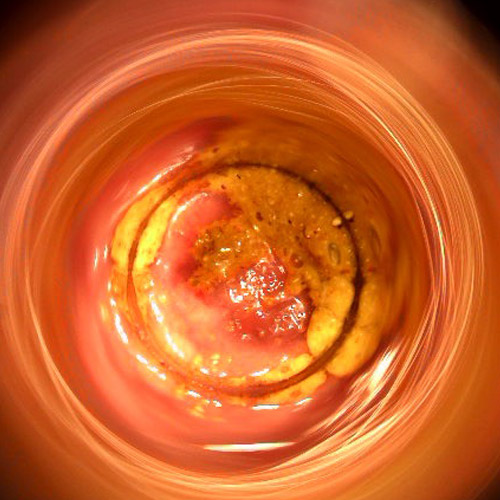
What is proctitis?

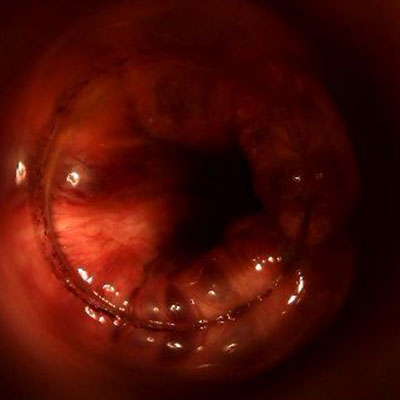
Proctitis is an inflammation similar to anitis, but unlike the latter it does not just extend to the peri-anal border and anal canal, but continues well beyond the pectinate line, thus involving the rectum.
It is, in essence, an extension and aggravation of anitis, with greater area of mucosa involved.
Again, proctitis is a symptom, and not a pathology per se: generally, it is the consequence of major injuries to the mucosa of the rectum, such as after violent diarrheal discharges, or after expulsion of particularly hard stools, which have torn the delicate anorectal mucosa.
In proctitis, the rectal mucosa attempts to defend itself against the bacterial attack external to the lesions by producing large amounts of mucus which, sliding down by the force of gravity, can reach as far as the anal canal, causing yellowish and particularly dense discharge which, if not properly cleaned, in the long run causes maceration of the outer skin, perpetuating and aggravating the anitis.
Why does diarrhea cause inflammation of the anus and rectum?
In Medicine, 'diarrhea' is defined as the expulsion of unformed, liquid or otherwise semi-solidified stool.
This condition is to be considered pathological, and is always a cause of an upstream problem affecting the colon, namely the large intestine.
Such a problem can be of various kinds: inflammatory, caused by a chemical, bacterial, or viral attack; infectious (e.g., salmonella poisoning); congenital as a result of particular diseases (e.g., celiac disease); as a response to other auto-immune diseases, such as ulcerative rectocolitis and Crohn's disease; and so on.
Diarrhea is thus a defense of the body, which attempts to expel the toxins or microorganisms causing the infection externally, with acute discharges of malformed stools as they are not fully reabsorbed of their fluids.
In fact, the function of the colon is precisely to reabsorb the fluids from the chyle (the food already processed by the small intestine), to turn them into alvo, that is, stool.
During an episode of diarrhea, fluid reabsorption is not possible, as stools are expelled long before they are consolidated, hence their liquid or semi-liquid consistency.
Diarrheal stools, in addition to being liquid, are also highly acidified.
This injures and irritates the delicate anorectal canal, which becomes inflamed and reddened as they pass through, thus causing gowns and proctitis.
Episodes of chronic diarrhea, i.e., diarrhea in turn caused by a never or misdiagnosed, or neglected (e.g., irritable bowel syndrome) condition cause constant irritation of the anorectal canal, with real micro and macro lesions that, over time, can lead to chronic proctitis, with the onset of complications such as anal fissures and pathological hemorrhoids.
Pathological hemorrhoids and their inflammation

Hemorrhoids are pad-like vascular plexuses formed by arteries and veins joined together in what is called, in medical jargon, anastomosis.
Normally found within the anal canal, the three main hemorrhoidal plexuses (right anterior, right posterior, and left lateral) have the function of properly vascularizing the entire area of the anus, while simultaneously contributing to fecal restraint.
For various reasons, causes, and triggers, hemorrhoids often leak from their original location, prolapsing and extruding from the anal canal, giving rise to what is called hemorrhoidal pathology.
Pathological hemorrhoids, extruded and swollen with blood, are easily torn by feces, and can therefore become irritated and bleed, becoming painful, burning, and bothersome.
This constant irritation, if not properly treated, prompts the body to produce large amounts of mucus in an attempt to protect the anorectal canal.
In turn, mucus, produced in large quantities, can leak from the anus (also facilitated by the often suboptimal closure of the anus caused by hemorrhoidal prolapse), leading to maceration of the skin and thus causing bothersome anitis.
Anal fissure and chronic inflammation that does not heal
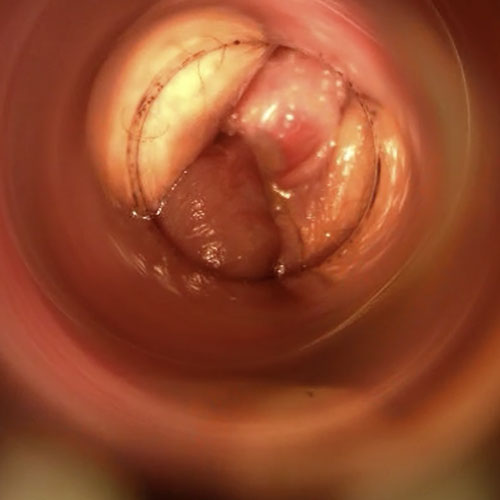
An anal fissure is a wound, or injury in medical jargon, of the peri-anal area and anal canal.
The characteristic feature of this wound, which is always vertical and parallel to the natural pleating of the anus, is that its healing is slow, very slow or, in the most severe cases, totally absent.
Almost always, failure to heal results from vascular complications that do not allow adequate oxygenation of the wound, and consequently the inability of cells to regenerate.
Often, this lack of vascularization is caused by continuous spasms of the internal sphincter muscle (in turn, generated by the presence of the fissure), in what is medically called sphincter hypertone.
A wound that does not heal in the anus causes constant pain, especially during evacuation, hematochezia (bleeding from the anus), burning, and itching, with associated chronic anitis.
This is because the body attempts to protect the lesion by overproducing mucus and sometimes forming a papilla of mucous membrane, swollen with blood, which becomes irritated and easily inflamed.
The open anus and the moist anus

A open anus is a pathological condition of the anus, which occurs when the orifice fails to close and thus closes completely, remaining half-open.
It is a situation caused by an upstream problem, almost always related to the sphincters, which obviously causes knock-on problems, going so far as to seriously affect the patient's quality of life.
Anus beante involves varied symptomatology of different severity: from mucus discharge, intestinal gas to stool leakage, thus resulting in true fecal incontinence.
The beating anus is also the primary cause of the so-called wet anus, that is, the pathological condition in which the anus is never dry and tight, but perpetually moistened by rectal mucus, which leads to rapid maceration of the mucosa and perianal skin, resulting in chronic anitis.
How do you treat anitis and proctitis?

Treatment for anitis and proctitis requires a rigorous medical history, and identification of the original cause of inflammation.
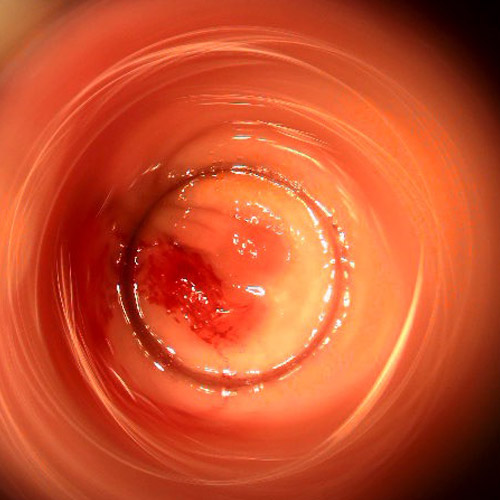
The patient's medical history should be carefully analyzed, and the clinical examination should also be combined with specific diagnostic tests, such as proctoscopy and any other tests that the physician deems appropriate to get to the exact origin of the inflammation of the rectum and anus.
The symptomatic treatment of anal and/or rectal inflammation must proceed hand in hand with the elimination of the cause that generated the irritation, otherwise, as is obvious, it may recur in the future.
Which physician specializes in the treatment of anitis and proctitis?

The physician specializing in all diseases of the rectum and anus is the Proctologist Surgeon.
A health care figure particularly trained in the study and care of the last part of the intestine, able to perform specialized diagnoses and examinations (such as modern Electronic Endoscopic Videoproctoscopy), which are essential to establish the true condition of the patient's anorectal canal, and thus provide the right diagnosis and therapy.
Do you suffer from frequent inflammation of the anus and are you from Dubai? Rely on Dr. Luisella Troyer

Dr. Luisella Troyer is a Vascular Surgeon in Dubai, specializing in Advanced Proctology.
In her clinic in Dubai you can find the best noninvasive proctological therapies and exams, such as modern Electronic Endoscopic Videoproctoscopy.
An indispensable examination to assess, painlessly and without preparation, the status of the anorectal canal, which can be stored electronically and reviewed several times for comparison, thus increasing diagnostic and therapeutic accuracy.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- ANITIS IS AN INFLAMMATION OF THEANAL ORIFICE AND CANAL, WHICH MAY ALSO EXTEND TO THE PERI-ANAL AREA;
- PROCTITIS IS AN INFLAMMATION NOT ONLY OF THE ANUS, BUT ALSO OF THE RECTAL CANAL;
- BOTH ANITIS AND PROCTITIS ARE DERMATITIS LOCALIZED TO A VERY NARROW AREA, NAMELY THAT OF THE ANORECTAL CANAL;
- THERE ARE MANY REASONS WHY THE ANORECTAL CANAL MAY BECOME INFLAMED AND REDDENED, BUT THE MOST COMMON ARE RELATED TO PROCTOLOGIC DISEASESANDALTERED ALVUS;
- PATHOLOGICAL HEMORRHOIDS OFTEN BRING FREQUENT ANITIS AND PROCTITIS, AS DO ANAL FISSURES;
- ANITIS CAN BRING INTENSE ANAL ITCHING, WHICH PERSISTS UNTIL THE UNDERLYING CAUSE OF INFLAMMATION IS RESOLVED;
- BEATING ANUS ANDFECAL INCONTINENCE CAN LEAD TO CONTINUOUS EMISSION OF FECAL DEBRIS AND MUCUS, WHICH, IN THE LONG RUN, LEADS TO MACERATION OF THE SKIN, RESULTING IN THE APPEARANCE OF ANITIS;
- IF YOU SUSPECT THAT YOU HAVE ANITIS, AVOID THE USE OF OVER-THE-COUNTER CORTISONE CREAMS AS MUCH AS POSSIBLE, BUT BOOK A SPECIALIST PROCTOLOGICAL EXAMINATION AS SOON AS POSSIBLE

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.