Do you experience frequent episodes of rectorrhagia (blood coming out of the anus, especially during or shortly after defecation), coupled with abdominal and pelvic pain, and frequent sensation of anal burning, as well as rectal tenesmus?
There is a particular type of rectal injury that has been known to science since the late 1800s, which falls within the broad group of proctologic disorders of traumatic origin.
A solitary ulcer of the rectum is a wound with almost always very painful symptomatology, which often puts the patient in great prostration, who does not understand where, exactly, the often very intense pain he feels is coming from, especially during evacuation.
Read this page to find out what this fairly rare ulcer is, how it is diagnosed, and what can be done to treat it.
The intestinal mucosa, including that of the rectum, like all other mucous membranes in the body, does not have the protective layer of the epidermis (the stratum corneum, formed by solified and stratified keratin ).
This means that, unlike the outer skin, the intestinal mucosa is much, much more delicate and sensitive, both to irritation from trauma and chemicals.
Hardened stools, typical of the constipated person, are often the cause of tears in the anorectal canal, with the formation of true ulcers, which struggle to heal especially if their presence creates spasms and hypertonus of the sphincter muscles.
The overactivity of the puborectal muscle and the continuous passage of hardened, stone-like stools are the cause, in most cases, of the formation of the solitary ulcer of the rectum.
What is solitary ulcer of the rectum?
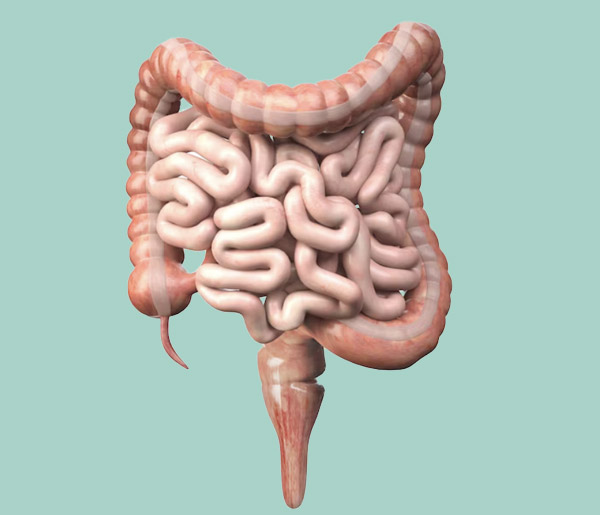
A solitary ulcer of the rectum is a lesion of the rectal canal, specifically the upper rectum, usually at or shortly after the rectal ampulla.
It presents as a deep and often very extensive wound, which sometimes is not so 'solitary' as it is accompanied by other lesions, and almost always by widespread inflammation (acute inflammation) around its edges.
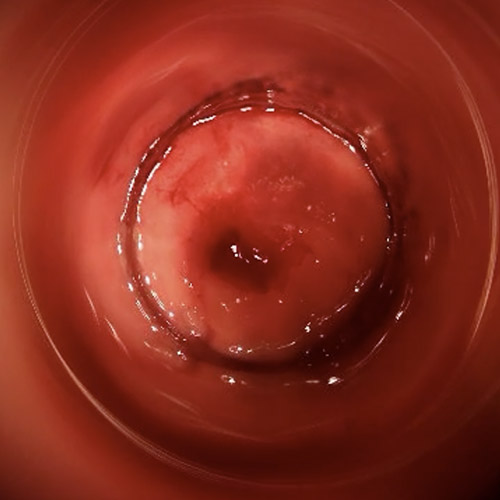
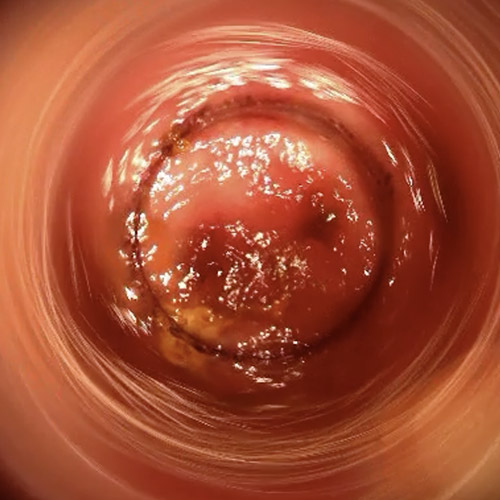
On visual examination, this particular lesion has all the characteristic signs of a true ulcer: bleeding (including spontaneous bleeding), inflamed and, if present for a long time, fibrotic edges, dark red course if still properly vascularized, with whitish background if, on the other hand, it has now morphed into a chronic fissure, in which granulation tissue is clearly visible.
Solitary ulcer of the rectum was first observed by the scientific method in the late 1800s, but its complete anatomo-pathology was accurately described in 1969.
What caused the solitary ulcer of the rectum?

Modern Medicine, after decades of speculation on the origin of this rare, but painful, proctologic condition, has established quite clearly that it is essentially dependent on constipation, and the intra-abdominal hyper-pressure it entails.
In fact, the continuous passage of hard, goat-like stools, typical of the constipated patient, the continuous trauma of the supporting structures of the rectal canal, and the systematic strains during pontication are the main causes of solitary rectal ulcer.
Not surprisingly, almost all (more than 90%) of patients who develop this type of rectal lesion suffer from chronic constipation that is never or poorly treated, while related perineal droop can be present in up to 60% of cases.
Hyper-activity of the puborectal muscle, due in turn to the high intra-abdominal pressure involved in chronic constipation, would thus seem to be the main reason for the occurrence of this particular ulcer.
Other mechanical and traumatic causes, such as constant and, often, too vigorous anal intercourse, or the use of large sex toys, may be considered other possible, if less likely, causes of the development of solitary rectal ulcer.
How common is solitary ulcer of the rectum?

Of all anorectal lesions, solitary rectal ulcer is quite rare: in fact, it is estimated to affect 1 in 100,000 individuals.
There is not much difference between genders, while the common thread in almost all patients with this lesion is chronic constipation, present in more than 90% of cases.
The change in the eating habits of modern people and their historical diet based on many vegetables and selected proteins, with the advent of fast food and low-cost hyper-caloric diets, has also had deleterious effects on the general intestinal regularity of the population, with a marked increase in chronic constipation, which has occurred in recent decades.
This increase in constipation most likely coincides with a related increase in cases of solitary rectal ulcers.
This hypothesis of an increase in cases of solitary rectal ulcers due to a change in diet is compatible with the observation of pathologies that were once uncommon in the young and very young (proctitis, pathological haemorrhoids and anal fissures), which are now much more prevalent due to the increase in cases of constipation.
Solitary rectal ulcer is also more common statistically between the second and third decade of life.
Correction of chronic constipation is imperative to allow the solitary rectal ulcer to heal.
Topical therapy, with cortisone and mesalazine products, although of great help in healing the lesion, is still not sufficient to ensure a decrease in intra-abdominal pressure.
Constipation is a real disease, which is the cause not only of solitary rectal ulcer, but also of many other proctologic conditions such as hemorrhoidal prolapse, prolapse of the rectum , and anal fissure formation.
In order for a solitary rectal ulcer to heal, therefore, the Proctology Physician must carefully investigate the patient's lifestyles and habits, modifying them and, if necessary, also planning rehabilitation of the bowel, based on biofeedbackand electrostimulation.
What are the symptoms of solitary rectal ulcer?

The symptoms of solitary rectal ulcer are quite insidious, as they are often confused with those of other intestinal diseases.
In contrast to anal fissure, which has often very clear symptomatology, solitary rectal ulcer has variable symptoms, sometimes not immediately describable with sufficient specificity by the patient.
In general, the main symptoms are:
- Rectoragy, sometimes even important;
- Sensation of abdominal and pelvic pain and constriction, which the patient, however, cannot well identify at its exact point of origin;
- Pain during defecation or soon after (rare symptom);
- Anal burning and generalized sensation of discomfort in the pelvis;
- Anal anitis and itching, caused by overproduction of mucus from the rectal canal;
- Tenesmus and foreign body sensation in the anus
These symptoms do not have to be present all at once, and their severity status is highly variable from patient to patient, also in relation to the severity of the constipation that, in most cases, generated the ulcer.
Chronic constipation is a condition largely dependent on dietary habits, which are acquired from childhood.
At one time, in the European Mediterranean countries (Italy, Spain, Greece, partially also France) the meager economic possibilities of the population, combined with a high cost of livestock for field work and an inherent difficulty in fishing, people were essentially obliged to eat mainly vegetables, fruits and cereals.
Protein intake was delegated almost exclusively to legumesand, only rarely, to fish and poultry meat, while red meat from large cattle,used primarily as a valuable labor force and thus not for food, was extremely rare.
To expensive dairy products (cream and butter), cheaper vegetable oils were preferred, such as the ubiquitous olive oil, at the time one of the main crops as it was able to take root almost everywhere.
This diet is called the 'Mediterranean diet,' and it is considered one of the most balanced diets possible for human beings, which moreover does not require large investments in animal husbandry.
This diet is also beneficial for the intestines, as it constantly supplies them with fiber, which keeps stools soft, full-bodied and easy to evacuate.
With the changing economic conditions of the country, the onset ofmass industrialization and the widespread increase in affluence, which led to hyper-caloric consumerism, this diet has gradually been lost, so that today it has all but disappeared as the dietary 'standard' of the population.
Unfortunately, the decrease in the amount of broad-leafed and green vegetables and the concomitant increase in sugarand animal protein, which are now very cheap, has also led to an increase in chronic constipation, which in turn causes hyper-absorption of fluids from the alvus in the colon and the concomitant emission of particularly hard stools.
These hard stools, passing through the sigma, which naturally 'curves' the intestine toward the rectum, impact the mucosa of the same, injuring it and giving rise to spasms of the pubo-rectal muscle, which worsens the vascularization of the wound and turns it into a solitary ulcer of the rectum.
How is solitary ulcer of the rectum diagnosed?
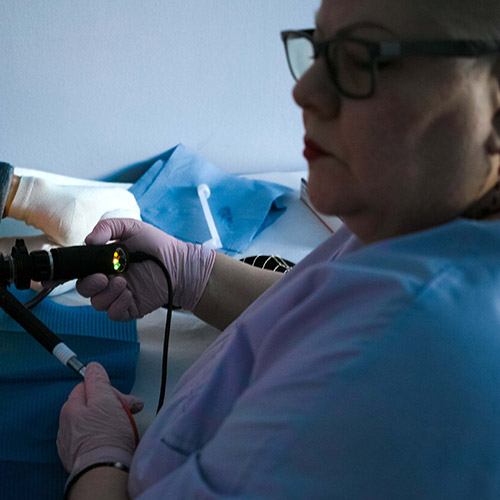
Given that solitary rectal ulcer is a lesion that afflicts, in almost all cases, the anterior part of the upper rectum, to diagnose it anoscopy is not enough, but there is a need for proctoscopy, performed with a proctoscope of at least 120-130mm in length.
Proctoscopy should be performed by inserting the instrument all the way into the rectal ampulla, and can be performed with or without the aid of a camera (a recommended choice, however, as it increases diagnostic accuracy).
On visual examination, the solitary ulcer of the rectum usually appears as a dark red, bleeding lesion, enveloped by a large area of inflamed mucosa, and sometimes also accompanied by other scattered lesions, coinciding with a true proctitis.
Rectal prolapse with descent of the perineum may also be associated with the ulcer, which occurs with between 10% and 60% of case histories.
How can a solitary rectal ulcer be treated?
Given that, as mentioned a little above, solitary ulcer of the rectum is almost always caused by abdominal hyper-pressure in turn generated by chronic constipation, therapy involves the mandatory correction of the patient's constipation.
By correcting constipation and reducing intra-abdominal pressure, hyper-activity of the puborectal muscle is concomitantly reduced, reducing rectal mucosal trauma.
Again, making stools soft facilitates their expulsion and prevents tearing of the delicate anorectal mucosa, which is often injured by the very passage of stools that are too hard.
Topical anti-inflammatory drugs (mesalazine or cortisone-based) can be combined to help the mucosa regenerate, but still alone they are not enough to resolve the ulcer, which always requires correction of the constipation.
Such correction, which often results in a long journey for the patient, involves diet and lifestyle modification as well as bowel and sometimes pelvic floor rehabilitation.
Pelvic floor rehabilitation can be performed through specific exercises and electrostimulation, while the biofeedback technique can be of great help for bowel rehabilitation.
Only in case of complete failure of this conservative therapy, or where a now severe and advanced stage of rectal prolapse is present, is the surgical option considered, which involves rectopexy (surgical lifting and suspension of the rectum) and, in case of concurrent mucosal prolapse, also prolassectomy.
It should always be emphasized, however, that even the surgical solution does not exempt from bowel rehabilitation and constipation correction, which must be compulsorily performed as a corollary of therapy.
In the medical field, anal bleeding has a specific name, namely rectorrhagia.
When the bleeding is moderate, let's say minor, it instead takes the standard of hematochezia.
Traces of blood on stool, toilet paper, or dripping bleeding from the anus, especially after evacuation, puts genuine terror in patients, who often run to the Doctor (sometimes, even to the Emergency Room) very alarmed.
In reality, most anal bleeding is from entirely benign conditions, such as pathological hemorrhoids, anal fissures (of which solitary rectal ulcer is, roughly, a subcategory) or even from proctitis.
Fortunately, cases of rectorrhagia caused by carcinoma of the bowel or anus are really the minority, and often the symptom occurs only in the end stage of cancer.
Here is the Physician who can diagnose and treat the solitary ulcer of the rectum?
The Medical specialist who can diagnose and treat solitary rectal ulcer is the Proctologist Surgeon, that is, the health professional who is particularly trained and educated in diseases of the rectum and anus.
Do you think you are suffering from a solitary rectal ulcer? Dr. Troyer can help you
Dr. Luisella Troyer is a Proctologist Surgeon with years of experience in diseases that can afflict the rectum and anus, including solitary rectal ulcer.
In her clinic in Dubai, Dr. Troyer can easily diagnose solitary rectal ulcers using Electronic Endoscopic Videoproctoscopy: a modern, noninvasive, totally digital examination that can clearly highlight, in high definition, the presence of any type of lesion in the anorectal canal.
With Dr.'s therapies, both pharmacological and constipation rehabilitation, you will be able to treat the possible presence of solitary rectal ulcer, not only resolving discomfort and pain that such an injury entails, but also getting back to feeling good about your intestines.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- SOLITARY RECTAL ULCER IS A LESION OF THE UPPER RECTUM CAUSED BY OVER-ACTIVITY OF THE PUBORECTAL MUSCLE, WHICH IN TURN IS CAUSED BY THE STATE OF CHRONIC CONSTIPATION;
- THRUSTING AND IMPETUOUS SEXUAL ACTIVITY CAN ALSO CAUSE THE APPEARANCE OF THIS PARTICULAR RECTAL LESION;
- STATISTICALLY, SOLITARY RECTAL ULCER IS QUITE RARE, AFFECTING ABOUT ONE IN 100,000 PEOPLE;
- TO DIAGNOSE SOLITARY ULCER OF THE RECTUM, TRADITIONAL ANOSCOPY IS NOT ENOUGH, BUT PROCTOSCOPY, PREFERABLY ELECTRONIC, IS NEEDED;
- ON VISUAL EXAMINATION, THE SOLITARY RECTAL ULCER HAS A DARK RED COLOR, BLEEDING, WITH BORDERS IN INFLAMMATION AND THE SURROUNDING MUCOSAL AREA INFLAMED AND CONGESTED;
- IF PRESENT FOR A LONG TIME, THE SOLITARY ULCER OF THE RECTUM MAY BECOME FISSURED, BECOMING A LESION WITH A WHITISH BACKGROUND AND HARD, FIBROTIC MARGINS, TYPICAL OF A FISSURE;
- THE MAIN SYMPTOMS OF SOLITARY ULCER OF THE RECTUM ARE ANAL BLEEDING, ESPECIALLY DURING OR SHORTLY AFTER DEFECATION, SENSATION OF TENESMUS AND FOREIGN BODY IN THE ANUS, PAIN OF THE PERINEOCHETHE PATIENT STRUGGLES TO IDENTIFY ACCURATELY, PROCTITIS AND ANITIS, DUE TO MACERATION OF THE MUCOSA AND PERIANAL SKIN AS A RESULT OF OVERPRODUCTION OF MUCUS FROM THE INTESTINE;
- THERAPY FOR SOLITARY ULCER OF THE RECTUM INVOLVES THE MANDATORY CORRECTION OF CONSTIPATION, IN TURN PERFORMED BY MODIFYING THE PATIENT'S DIET AND LIFESTYLE, AND POSSIBLY INTESTINAL REHABILITATION;
- TO DIETARY CORRECTION, TOPICAL CORTISONE AND MESALAZINE PRODUCTS SHOULD BE ADDED, WHICH ARE USEFUL IN FACILITATING ULCER HEALING;
- ONLY WHEN CONSERVATIVE THERAPIES HAVE NO EFFECT, THE SURGICAL SOLUTION IS RESORTED TO

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.