Crohn's disease is one of the most debilitating auto-immune diseases that can affect the human gastrointestinal system.
n Italy, it affects about 392 people per 100,000 population, and is one of the leading causes of chronic intestinal inflammation with complications that require frequent surgical access.
Read this page to learn about the causes of Crohn's disease, its diagnosis, and the state of research for effective treatment.
La malattia di Crohn è spesso mal diagnosticata, poiché ha sintomi simili a quelli di altre patologie infiammatorie del colon, di eguale origine autoimmune, come ad esempio la rettocolite ulcerosa.
Questa difficoltà di diagnosi spesso peggiora la condizione dei pazienti che, senza capire esattamente cosa hanno, ritardano le terapie antiinfiammatorie e immunosoppressorie.
What is Crohn's disease?
Crohn's disease, or regional enteritis, is an autoimmune disease of the entire gastrointestinal duct, named after American Gastroenterologist Dr. Burril Bernard Crohn who first accurately described its symptoms and condition in the 1930s.
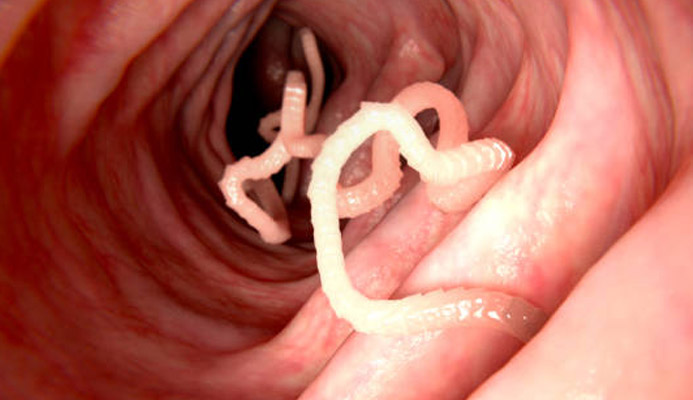
It manifests as a violent inflammation that can affect the entire gastrointestinal tract, triggering chronic inflammation of the mucosa and the formation of true ulcerations, often requiring emergency surgical access.
Worldwide, the number of patients suffering from Crohn's disease has been steadily rising (by about 20 times) over the past decade.
What are the causes of Crohn's disease?
Crohn's disease is an autoimmune disease, so it is triggered by an abnormal attack by the immune system on the very fibers and tissues of the body, in this case the gastrointestinal duct.
This self-attack causes constant inflammation of the intestinal mucosa, resulting in more or less severe lesions that can degenerate into true ulcers.
As with all other autoimmune diseases, the exact origin of why this abnormal behavior occurs is currently unclear to Medicine, but a genetic predisposition, mixed with hypothetical environmental factors, is still suspected.
Research has established that mutations in the CARD15 and NOD2 gene, located on chromosome 16, are certain culprits for predisposition to the disease, although it is believed, however, that they are not the only ones, and there are many others involved.
However, genetic predisposition, even it's now proven, still does not establish the certainty of disease onset.
In fact, only a limited percentage (roughly 1 in 200) of patients with a genetic predisposition will later develop, statistically, the symptoms of Crohn's disease.
Risk factors related to diets and lifestyles are then added to genetic and hereditary factors.
Excessive consumption of animal protein and milk or related food, in fact, has been established as an element related to increased likelihood of developing the disease.
The use of the contraceptive pill as a trigger has been a topic of scientific discussion since the 1960s, when, coinciding with the massive spread of this method of contraception in the U.S., there was a considerable increase in the disease in the female population.
This combination, however, has not yet been scientifically proven, so it remains onlya mere supposition.
The possible relationship between abnormal mutation of intestinal bacterial flora with the onset of Crohn's disease has also only been surmised but not clarified.
In recent times, the theory of greatest research support is that Crohn's disease is an extreme response of the body to a massive and dramatic drop in intestinal immune responses.
A kind of 'adaptive compensation' of a deficient immune system that, absurdly, attempts to compensate itself but produces a hyper-response that is harmful to the body.
When does Crohn's disease occur?
Usually, symptoms of Crohn's disease occur as early as childhood, with a major peak in the age from adolescence to early adulthood.
Nevertheless, Crohn's disease can still develop at any age of life, even after the age of 50, without precise correlation with the patient's age group.
What are the symptoms of Crohn's disease?
Crohn's disease is seen by many as a syndrome, as its symptoms are really wide-ranging, and can vary greatly from patient to patient.
This makes diagnosis difficult, as many patients go without proper treatment for years before they finally have an explanation for their symptoms.
The important thing to note is that Crohn's disease involves periods of remission that alternate with periods of recurrence, in a cycle that is often impossible to predict beforehand.
The most common symptom of Crohn's disease is that of chronic diarrhea: always present, it is often accompanied by abdominal and joint pain, often associated with spasms and cramps.
Leakage of blood (hematochezia) from the anus during defecation is a related symptom, as is the perennial fever that usually arises in the evening and then wanes in the morning.
II problem of chronic diarrhea is a serious one, as the patient with Crohn's disease can go as high as twenty and more discharges during the day in acute periods, causing chronic anitis and proctitis, with the formation of anal fissures, abscesses, and fistulas.
These symptoms are caused by the continued formation of ulcers in the intestinal tract, which, as they do not regress, give rise to the problems described above.
Although the disease focuses almost exclusively on the gastrointestinal mucosa, some symptoms can affect outside this area as well.
In fact, canker sores in the mouth, ulcers on the skin, and cause severe depression can appear.
How is Crohn's disease diagnosed?
Diagnosis of Crohn's disease can often be difficult, as its symptoms may also appear common to other disease conditions such as ulcerative rectocolitis and irritable bowel syndrome.
The first-line examination, which is successful in identifying Crohn's disease in more than 70% of cases, is colonoscopy.
During the examination, in addition to observation and evaluation of the state of the intestinal mucosa, small tissue samples (a biopsy) can also be taken to perform useful laboratory tests.
Colonoscopy is often combined with contrast-enhanced Nuclear Magnetic Resonance Imaging, which has proven extremely useful in detecting local inflammation that is the origin of symptoms.
Is there a treatment for Crohn's disease?
At present, as with all other autoimmune diseases, modern Medicine has no definitive cure for Crohn's disease.
Therefore, the possible therapy is only supportive, trying to improve the patient's living condition and isolate (over time and locally) inflammatory bowel episodes.
Therapy therefore aims to reduce chronic inflammation while regularizing normal bowel function, preventing (over possible) inflammatory recurrences.
These goals are usually obtained with the use of antibiotic, anti-inflammatory, and immunosuppressant therapy.
Fortunately, there are powerful new immunosuppressive drugs available, such as azathioprine, 6-mercaptopurine, and methotrexate, which are capable of directly inhibiting the lymphocytes responsible for intestinal inflammation, thus achieving immediate immediate benefits.
With the use of these new immunosuppressants, it is possible to guarantee the patient an infinitely higher quality of life than in the past, with a reduction in violent recurrences and, consequently, less recourse to Surgery.
Nevertheless, the use of Surgery still proves indispensable when an attack does not respond effectively to drug treatment, and triggers substantial ulceration of a given intestinal tract.
A stenosis caused by mucosal inflammation, which carries a risk of a true intestinal infarction, must also be treated with Surgery, as must the occurrence of peri-anal abscesses and anal fistulas.
Who is the Physician who can diagnose and treat Crohn's disease?
Crohn's disease is the responsibility of Colonproctology and Gastroenterology, so the Physician to whom one should refer if the symptoms of the disease are suspected is the Colonproctology Surgeon or Gastroenterology Physician.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- CROHN 'S DISEASE , FORMERLY KNOWN AS CROHN'S DISEASE , IS AN AUTOIMMUNE DISEASE THAT AFFLICTS THE TISSUES OF THE INTESTINAL WALL;
- ALONG WITH ULCERATIVE RECTOCOLITIS, CROHN'S DISEASE IS AMONG THE AUTOIMMUNE-BASED CHRONIC INFLAMMATORY BOWEL DISEASES THAT AFFLICT A GREATER PERCENTAGE OF HUMANS;
- CROHN'S DISEASE SYSTEMATICALLY DAMAGES THE INTESTINAL WALL AS LYMPHOCYTESPRODUCED BY THE IMMUNE SYSTEM ATTACK THE CELLSULEDELLAMIUCOSA ITSELF, CAUSING INFLAMMATION;
- IN THE CURRENT STATE OF MEDICAL RESEARCH, ALTHOUGH GENETIC MUTATIONS HAVE BEEN FOUND TO BE RESPONSIBLE FOR THE DISEASE, IT IS ESTIMATED THAT THERE ARE MANY MORE, SO THE EXACT ETIOLOGY IS NOT CURRENTLY KNOWN;
- LIKE MANY OTHER AUTOIMMUNE DISEASES, THERE IS CURRENTLY NO CURE THAT CAN ERADICATE THE DISEASE; HOWEVER, SUPPORTIVE THERAPIES ARE AVAILABLE;
- THE PURPOSE OF THERAPY FOR CROHN'S DISEASE IS TO RELIEVE THE PATIENT'S SYMPTOMS, AND PREVENT NEW VIOLENT ATTACKS;
- THERAPY FOR CROHN'S DISEASE IS BASED ON THE ADMINISTRATION OF ANTIBIOTICS, ANTI-INFLAMMATORIES, AND IMMUNOSUPPRESSANTS;
- WHEN DRUG THERAPY FAILS, SURGERY IS NECESSARY TO REMOVE THE NOW CHRONICALLY INFLAMED SECTION OF INTESTINE

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.