Are you experiencing great pain in your anus and rectum, which no longer even makes you walk easily, and makes your every evacuation a pain?
After each discharge, do you see blood on your stool or toilet paper, and upon touching your anus, do you feel painful growths?
This painful situation usually requires urgent medical and sometimes surgical care.
You may be suffering from what, in medical jargon, is called a hemorrhoidal crisis.
Find out what a hemorrhoidal crisis is, and what you can do to get immediate comfort from the pain.
Often, the presence of blood on stool or toilet papergenuinely terrifies the patient, who immediately thinks he or she has some form of cancer in the anus or rectum.
In reality, although hematochezia (anal bleeding) may be a symptom of carcinoma of the rectum or colon, it is statistically much more likely that it you know depended on the tearing of inflamed and prolapsed hemorrhoids.
That is why, in case you notice bright red blood on your stool or toilet paper, it is important to remain calm and not to be alarmed, and then to book a specialized proctological examination as soon as possible.
What is a hemorrhoidal crisis?

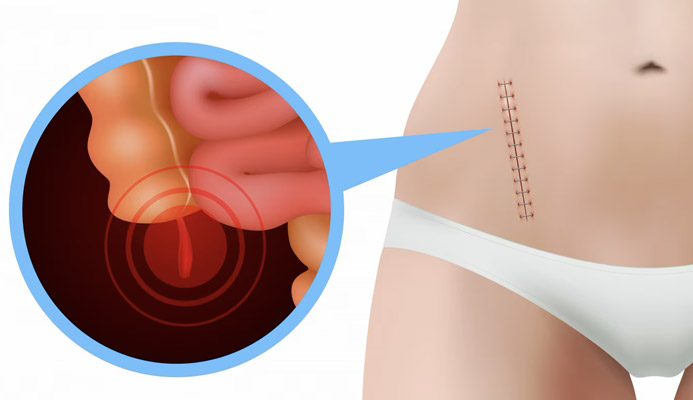
In medical terms, hemorrhoidal crisis refers to inflammation and congestion of already pathological hemorrhoids, with the formation of a painful hemorrhoidal thrombus (a blood clot within a plexus of the hemorrhoids).
This condition is extremely painful for the patient: the pain of the thrombus, combined with the congestion of the hemorrhoids and their inflammation, makes defecating extremely problematic, and sometimes the pain goes so far as to undermine even natural, everyday body movements, often totally immobilizing the subject.
Burning, itching, and bleeding during evacuation are the related symptoms almost always present, worsening the overall clinical picture.
The experience of hemorrhoidal thrombus is considered by patients who have experienced it, similarly to the pain caused by perianal abscess, to be one of the greatest possible sufferings in Proctology.
This condition of great distress usually makes the patient seek immediate medical care, even after years and years of procrastination in treating prolapsed hemorrhoids (the trigger for hemorrhoid crisis).
What are hemorrhoids?
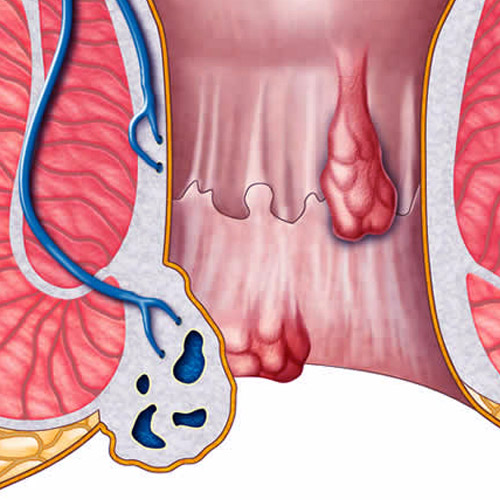
Hemorrhoids are arteriovenous plexuses, much like pads where veins and arteries are fused together (anastomosed, in medical terms).
They are natural vascular elements present in our anal canal, and their main task is to oxygenate the tissues of the anus and anal orifice.
Secondly, hemorrhoids assist the anal sphincters in fecal containment.
We all have three main hemorrhoidal plexuses: left lateral, right anterior, right posterior, to which are added, more externally toward the anal orifice, two small secondary plexuses.
In normal situations, hemorrhoids do not give any trouble and are therefore not even perceived, performing their task silently.
Only when there is a problem that leads to their inflammation, congestion, and extrusion (prolapse) from their original location is it more properly referred to as pathological hemorrhoids, or hemorrhoidal disease.
Why do hemorrhoids get sick?
Exactly why hemorrhoids swell and prolapse out of their original anatomical location is not yet known to science.
Nevertheless, time has ascertained the development of two distinct theories, not necessarily in conflict with each other:
- The mechanical theory, which sees hemorrhoids enlarging and processing due to a natural failure of the elastic tissue of the anorectal mucosa, mainly due to increasing age, decreased collagen production (or the low percentage of the same decided on a genetic basis), and increased intraabdominal pressure, typical, for example, of constipated patients;
- The hemodynamic theory, which sees the hemorrhoids enlarging and extruding out of the anal canal due to the increased amount of blood present in the plexuses (a hyperflow, properly so called), with poor quality of the internal tissues of the hemorrhoids, which easily wear out in the presence of little collagen
As mentioned just above, the two theories are not at odds with each other, and they can coexist in explaining the onset of hemorrhoidal prolapse.
In addition to these two main causes, there is a wide array of triggers, now known to science for many years, that can initiate hemorrhoidal prolapse:
- ‚ĀÉ Chronic constipation;
- Chronic diarrhea;
- Irritable colon, with alternating periods of constipation and diarrhea;
- Pregnancy and natural childbirth;
- Cycling, motorcycling and horseback riding;
- Weightlifting and body building;
- Obesity;
- Sedentary living and low physical activity;
- Some types of very wearing jobs (porter, bricklayer, carpenter, mover, etc.);
- Some types of sports that involve great intraabdominal pressure
Sometimes, these triggers add up to each other, thus increasing the risk of the onset of hemorrhoidal disease.
The pain of hemorrhoidal thrombus is often reported as exhausting, acute, disabling, and capable of almost completely immobilizing the patient, who often cannot even walk normally.
Fortunately, the acute phase of hemorrhoidal crisis usually lasts only a few days and then fades over time.
This is because the thrombus is slowly reabsorbed by thebody, although this may mean waiting several weeks (usually, four or more).
That is why, in severe cases of hemorrhoidal thrombosis that cause intense pain to the patient, immediate relief can be given with outpatient incision, and rapid release of the thrombus.
What are the symptoms of pathological hemorrhoids?

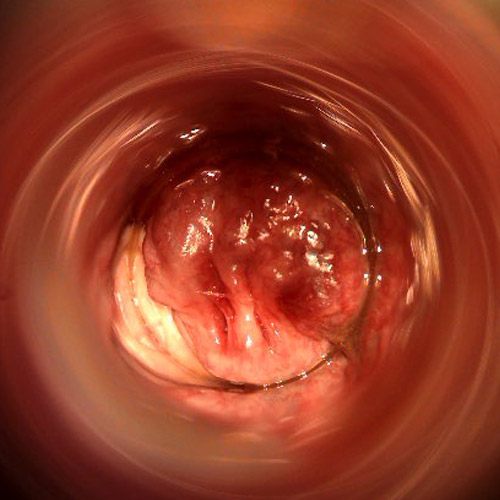
The main symptoms of diseased hemorrhoids are the result of their swelling, with associated prolapse from their original anatomical site, and subsequent extrusion into the anal canal.
This prolapse from this very common symptomatology:
- ‚ĀÉ Bleeding, with 'bright red' blood loss during or shortly after evacuation, caused by tearing of the hemorrhoidal wall as stool passes (especially if it is hard, typical of the constipated patient);
- Prolapse and extrusion of hemorrhoids, which may leak from the anal canal and be clearly perceptible to the touch;
- Hyper-production of mucus, the body's natural act of defense toward processed tissues, which soils clothing and makes the anus constantly 'wet';
- Irritation and inflammation of the anus and perianal area, given by the dampness of overproduction of mucus, often causing anitis and proctitis;
- In cases of hemorrhoidal thrombosis, intense anal pain, often felt as unbearable
The very last symptom is what triggers the so-called hemorrhoidal crisis.
Hemorrhoidal thrombus: what is it, and why does it hurt so much?
A hemorrhoidal thrombus is a blood clot that forms in one of the prolapsed and congested hemorrhoidal plexuses.
This is the most painful and dreaded complication of hemorrhoidal disease, creating great discomfort for the patient and prompting him or her, in most cases, to seek immediate medical help, even after years of laxity about the condition of his or her hemorrhoids.
In bulging hemorrhoidal plexuses, thrombus formation causes 'throttling' of the already limited (almost stagnant) circulation, with immediate sensation of pain, swelling and congestion.
This pain, not unlike that experienced in cases of thrombophlebitis, is judged to be intense and excruciating by patients, and is not limited exclusively to the act of defecation, but continues afterward, in fact preventing the patient from even regular walking.
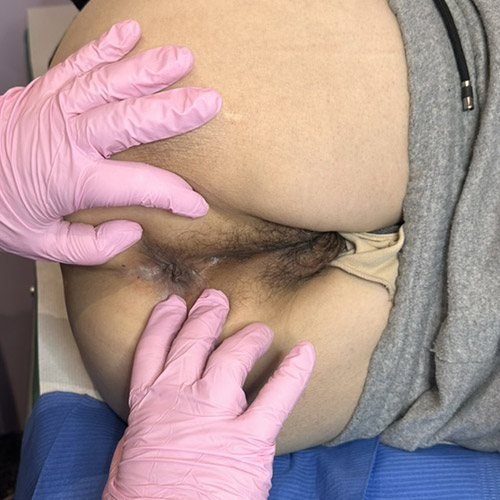
On visual examination, the hemorrhoidal thrombus appears purplish, sometimes almost dark, and is always located over a hemorrhoidal plexus, which in turn is inflamed and congested.
Digital inspection by the physician is often complicated, as the patient experiences great pain at even the slightest touch.
The thrombus is then associated with all the remaining symptoms of pathological hemorrhoids such as hematochezia (bleeding during defecation), burning, itching, and foreign body sensation in the anus.
If there is a positive side to a hemorrhoid crisis, it is surely that it usually prompts the patient to finally seek specialized medical help, and to stop procrastinating the proctological visit.
Almost all cases of high-stage hemorrhoids, which are now chronic and perpetually congested, are due precisely to the carelessness of patients who, out of shame or fear of pain, have constantly put off the proctological visit.
With the result of furthering the likelihood of developing painful hemorrhoidal thrombosis.
Why does a hemorrhoidal thrombus form?

The causes of hemorrhoidal thrombus formation can vary, but often this complication occurs in already pathological patients who have systematically ignored their condition and, with it, prolapse reduction treatments for years.
However, cases of thrombus occurring even without a prior pathological condition of particular significance, perhaps after sporadic episodes of constipation, are not uncommon.
One of the triggers for hemorrhoidal thrombosis is ablutions with water that is too cold (an unfortunately common behavior of patients with pathological hemorrhoids), which congests the already poor blood circulation in the hemorrhoidal plexuses and promotes clot formation.
Sometimes, hemorrhoidal thrombus can form after a particularly acute episode of constipation, with the emission of stools that are too hard.
Bicycling, motorcycling, horseback riding, and weightlifting, by increasing intraabdominal pressure, can also be triggers for hemorrhoidal thrombus, and subsequent hemorrhoidal crisis.
What is the therapy for hemorrhoidal thrombus?
Therapy for hemorrhoidal thrombus varies according to its severity, i.e., both its painfulness, reported by the patient, and its volume.
Small and not particularly painful thrombi can be treated with conservative medical therapy, which relies on dietary correction, adequate daily hydration, prescription of local cream emollients, and intake of flavonoids either topically or as systemic supplements.
The premise of this therapy is that all hemorrhoidal thrombi, albeit with time, are reabsorbed, and thus the treatment is supportive to the patient to facilitate healing and relieve pain.
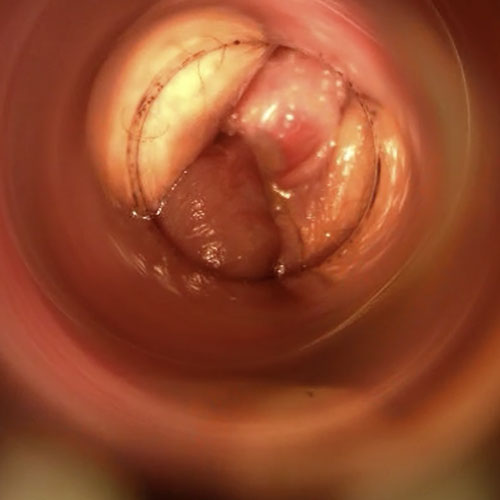
Large or particularly painful thrombi have surgical incision as an indication.
The incision, made by a Proctologist Surgeon, by means of prior local anesthesia, allows the thrombus to come out immediately, and consequently the immediate end of pain.
The small incision is not sutured but only cauterized, and full healing of the area takes place over the next few weeks without any particular trauma.
The patient is prescribed soothing creams and gentle cleansers as well as, of course diet care and appropriate daily hydration, which is essential to make stools soft and easy to evacuate.
Obviously, in the case of both conservative therapy and surgical incision, once the thrombus is reabsorbed and the hemorrhoidal congestion is flared, it will be mandatory to intervene on the prolapse, either by medical or surgical treatments.
Does hemorrhoidal thrombus incision give immediate pain relief?
Yes: the incision and removal of the thrombus performed under local anesthesia by the Proctologist Surgeon results in an immediate end to the acute pain of thrombosis, and thus instant relief.
After the incision there may remain a physiological burning sensation, a little postoperative edema, and a little congestion, which is completely normal and will reabsorb in the weeks following surgery.
The patient can still return to his or her normal daily and work activities, indeed: the return to walking is facilitated and requested by the Physician, and speeds up recovery time.
Is hemorrhoid thrombus treatment a cure for hemorrhoids?

No, in the most absolute way.
Surgery on the surgical hemorrhoidal thrombus is an emergency therapy to resolve the thrombosis that causes enormous pain to the patient, but has no curative effect on the prolapsed hemorrhoidal plexuses.
That is why, once healed, the patient will still need to address and solve the hemorrhoidal problem once and for all, such as with sclerosing therapy with scleromousse.
If the root problem, the hemorrhoidal prolapse, is not solved, there is always the possibility of developing new, painful thrombus in the future.
Who should be referred to for the treatment of hemorrhoidal thrombus?

The appropriate health professional to diagnose and treat a hemorrhoid crisis is the Proctologist Surgeon, who is usually a Vascular Surgeon.
Indeed, emergency treatment of excessively painful and bulky hemorrhoidal thrombi requires surgical expertise, not just medical expertise.
Often, gripped by anguish and pain, the patient resorts to the emergency room in an attempt to find support for the condition often judged unbearable, but it should be remembered that the first emergency admissions of hospitals are, of course, reserved for cases where there is precisely an urgent and life-threatening condition.
As painful as it is, a hemorrhoidal thrombus is not life-threatening, and therefore access to the emergency room should be avoided, especially in the situation of great difficulty and great influx that our hospitals have unfortunately suffered for years.
Therefore, the sensible thing to do if you experience symptoms of a hemorrhoidal thrombus is to book a proctologic examination with a Proctologist Surgeon, and not to clog emergency rooms.
Place where a Proctologist Surgeon is rarely present (for obvious reasons of demand), which is therefore poorly suited to find right support.
Are you suffering from a hemorrhoidal crisis in Dubai? Dr. Luisella Troyer can help you

Dr. Luisella Troyer is a Vascular Surgeon specializing in Proctology, with more than 5,000 operating room hours behind her, and 30 years of practicing medicine.
If you experience the great pain of a hemorrhoidal thrombus, Dr. Troyer can help you diagnose and treat it, including surgical incision (where clinically indicated).
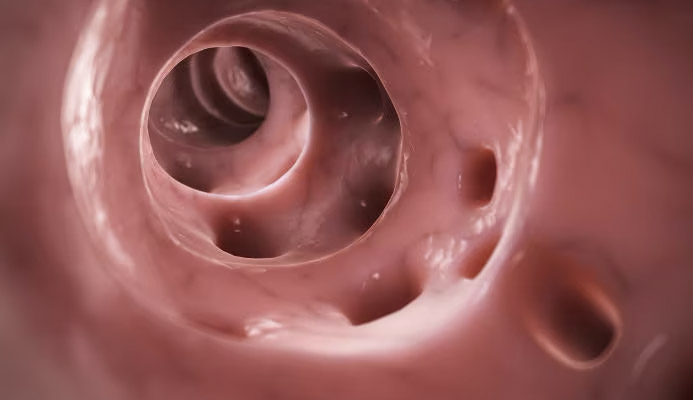
In the Dr. Troyer's clinic in Dubai there is a modern, fully electronic proctoscope, with which Electronic Endoscopic Videoproctoscopy can be performed painlessly, for an accurate analysis of your anorectal situation, which will help the Doctor to propose the right treatment.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- HEMORRHOIDS ARENATURAL ANATOMICAL VASCULAR PLEXUSES PRESENT IN OUR ANAL CANAL;
- IN NORMAL SITUATIONS, HEMORRHOIDS DO NOT CAUSE ANY DISCOMFORT, AND IN FACT CONTRIBUTE TO FECAL CONTINENCE;
- WHEN HEMORRHOIDS ENLARGE AND PROLAPSE OUTSIDE THE ANUS, IT IS CALLED HEMORRHOIDAL DISEASE;
- THE CAUSE OF HEMORRHOID DISEASE IS NOT YET WELL DEFINED, BUT A GENETIC PREDISPOSITION OF TISSUE QUALITY, NATURAL PHYSIOLOGICAL AGING, AND OTHER TRIGGERS (SUCH AS CHRONIC CONSTIPATION) ARE SUSPECTED TO BE THE MAIN CONDITIONS THAT CAUSE HEMORRHOID PLEXUSES TO PROLAPSE;
- HEMORRHOIDS CAN PROLAPSE INTERNALLY AND EXTERNALLY TO THE ANAL CANAL: THE LATTER PROLAPSE IS PARTICULARLY PAINFUL BECAUSE THE ANAL ORIFICE AREA IS MUCH MORE INNERVATED THAN THE DEEP CANAL;
- HEMORRHOIDAL THROMBUS IS A BLOOD CLOT THAT FORMS AS A COMPLICATION OF AN UNTREATED OR NEGLECTED HEMORRHOIDAL PROLAPSE;
- THE DYNAMICS LEADING TO THE FORMATION OF A HEMORRHOIDAL THROMBUS ARE UNCLEAR, BUT SEDENTARY LIFESTYLEAND LOW MOTOR ACTIVITYSEEM TOPLAY A MAJOR ROLE IN ITS OCCURRENCE;
- A HEMORRHOIDAL THROMBUS IN EXTERNAL HEMORRHOIDS IS USUALLY EXTREMELY PAINFUL, WITH PAIN OFTEN JUDGED BY THE PATIENT AS UNBEARABLE;
- THE SIZE OF THE PROLAPSE AND THROMBUS SEEMS TO HAVE LITTLE RELATION TO ITS PAINLESSNESS: THERE ARE EXTREMELY PAINFUL SMALL THROMBI AND LARGER, ALMOST PAINLESS THROMBI;
- THERAPY FOR HEMORRHOIDAL THROMBUS CAN BE CONSERVATIVE, IF THE PATIENT DOES NOT HAVE MUCH PAIN, OR NECESSARILY SURGICAL, BY MEANS OF THROMBECTOMY;
- OVER TIME, ALL HEMORRHOIDAL THROMBI REABSORB, BUT THROMBECTOMY IS SOMETIMES NECESSARY TO GIVE IMMEDIATE RELIEF TO THE PATIENT, WHO OFTEN COMPLAINS OF UNBEARABLE PAIN;
- HEMORRHOIDAL THROMBUS CAN MAKE DEFECATION DIFFICULT OR ALMOST IMPOSSIBLE, BECAUSE OF THE GREAT PAIN IT CAN CAUSE DURING PONTICATION;
- TREATMENT OF THE HEMORRHOIDAL THROMBUS IS SYMPTOMATIC, BUT THE PATIENT MUST NECESSARILY THEN TREAT THE HEMORRHOIDAL PROLAPSE, AS THERE IS ALWAYS THE DANGER OF FURTHER THROMBIZATION OF THE HEMORRHOIDS, IN THE FUTURE;
- THE VASCULAR SURGEON PERFECTED IN PROCTOLOGY IS THE APPROPRIATE PHYSICIAN TO DIAGNOSE AND TREAT A HEMORRHOIDAL THROMBUS;
- AVOID TREATING THE HEMORRHOIDAL THROMBUS WITH OVER-THE-COUNTER CORTISONE CREAMS AND ANESTHETICS, BUT RATHER SEE A Proctologist Surgeon AS SOON AS POSSIBLE

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.