Have you ever wondered what is the best way to clean your anus after defecation?
Or are you a lover of anal sex and do not know whether it is necessary to provide anal canal cleaning before intercourse?
The anal orifice is a very sensitive part of the body, which is naturally traversed periodically by feces (stool), then organic waste composed almost exclusively of bacteria.
This characteristic of it makes the natural 'exit hole' of our body very delicate, always in contact with microorganisms and waste, which, however, at the same time can be its very natural protection.
And that therefore they should not be harmed.
On the Internet we often read genuine rubbish about anus cleansing, and even more often this misinformation is also dangerous, as it can give the patient completely inappropriate directions that sometimes cause actual anorectal disorders.
Read this page written by Dr. Luisella Troyer, Proctologist Surgeon, to learn about the best way to cleanse the anus without damage or irritation.
No anogenital cleanser, however gentle, should be used internally in the anal canal.
Cleaning should be limited to the area of the external orifice, removing fecal debris gently, thanks to the foam of the cleanser and the water, which should never be too cold or too hot.
Attempting to 'deep clean' the anal canal with any kind of soap or cleanser always results in irritation and inflammation, which must be avoided.
The anorectal canal is naturally 'dirty,' protected by mucus, the biofilm of our friendly bacteria, and also by fecal debris: this is how it should remain, always.
What is the anal orifice?

In anatomy, the anal orifice is the natural opening of the anal canal, that is, the very last part of the long human gastrodigestive tube.
In turn, the anal canal is the end of the rectal canal, which is the last segment of the large intestine that, in common parlance, is known simply as the colon.
The colon, the last organ of the gastrodigestive system, is a long, thick tube that wraps around the entire abdomen, conventionally divided into five anatomical sections: the ascending colon, the transverse colon, the descending colon, the sigma, and the rectum, i.e., the straight canal (hence the name) that ends right at the anus and the anal orifice.
The anal orifice is composed of both skin, then skin endowed with an epithelial layer (superficial stratum corneum) that, approximately 1-1.5m after the opening of the anus, becomes anal mucosa, seamlessly.
In contrast to the outer skin, the anal mucosa is no longer protected by the stratum corneum, making it much more sensitive and delicate to both chemical agents and, of course, any external pathogenic infections.
How do stools form?

Feces are formed progressively in the intestines from a whitish liquid called chyle.
The chyle, which is poured from the ileocecal valve into the colon, is the result of the depletion of chyme, that is, the nutrient that, loaded with energy, has already been absorbed and metabolized by the small intestine.
In the colon, the branched network of chyliferous vessels that permeate the entire intestinal mucosa progressively absorb the liquids and electrolytes from the chyle, compacting it and slowly turning it into a compact mass that is no longer liquid.
The small scraps of polysaccharides still in the kilo are likewise attacked by a large number of bacteria that live symbiotically in our intestinal mucosa, called the bacterial flora.
There are so many kinds, and these microorganisms help the colon to compact and increase in volume the pound, swelling it and making it solid yes but soft, easy to be expelled.
The friendly bacteria that live in our mucosa also attack bilirubin, a component of bile that is discarded from the breakdown of red blood cells and is sent from the liver to the intestines, just to be disposed of.
Bacteria ferment bilirubin by feeding on the glucoronic acid in it, and turn it into stercobilin, a brown pigment that gives the classic color of healthy stools.
From the cecum of the colon, the chyle, which is slowly transmuted into feces, travels throughout the intestine by the natural movement of peristalsis: synchronized contractions of the intestinal mucosa that push the forming fecal material toward the rectum.
In the rectum, feces are collected in the rectal ampulla: an ectasia of the rectal canal made precisely ampulla-like, which dilates to accommodate feces and, by dilating, gives us the urge to defecate.
Defecation is the last act of this long journey, ending with the opening of the anal orifice and the expulsion of the formed feces.
Sphincter muscles and fecal continence
The opening and closing of the anal orifice, and thus fecal continence, is enabled by two specific muscles located just around the anal canal: the sphincter muscles.
These two particular muscles have a doughnut shape, and are concentric: there is the internal sphincter, in direct contact with the outer wall of the anal canal, and the external sphincter, which wraps around the former.
The internal sphincter is an involuntary smooth muscle: therefore, it cannot be controlled directly, as its contraction is dictated by the involuntary nervous system.
The external sphincter, on the other hand, is a red striated muscle, of fibers common to those of all other muscles in the body, and can be controlled voluntarily.
The two sphincters work in synchrony, in a healthy subject without proctologic or bowel disease: when the rectal ampulla fills with feces, the internal sphincter begins to relax, and there is the urge to defecate.
The external sphincter is commanded at our pleasure, and thus allows evacuation when the social situation permits, or, in return, allows stool to be withheld if the moment does not permit defecation.
The well-being of the anal mucosa is important for the proper functioning of the internal sphincter, as irritation, cuts, and abrasions of the mucosa can lead the muscle to dangerous spasms, which increase its tone (i.e., the tightening capacity of the anus) and, as a result, worse vascularization and oxygenation of the entire area.
In the past, in the countries of the Arabian Peninsula, cleansing after defecation was done, in order to preserve the very precious water, with... The left hand.
It was in fact that hand that had the rather thankless but nonetheless necessary task of cleaning the anal orifice from the remnants of feces.
The hand was then cleaned by 'washing' it with sand.
And certainly, in those days, the reason why one did not therefore use the left hand to greet friends and strangers is definitely sensible.
Since those days, fortunately, much has changed, but the tradition of... has remained. Never give the left hand during a convivial presentation.
The presence of feces in the anorectal canal: a normal physiological situation
The cycle of stool formation seen above is continuous in a human being.
Daily nourishment, which is indispensable for each of us, is constantly converted into energy and chemicals that are essential for the body, and waste is excreted in the form of feces after the long journey of digestion.
In a healthy individual, with a varied and balanced diet, proper hydration and daily fiber intake, an average of 150 grams of stool is produced each day, excreted by daily defecation.
This means that the whole gut is always, constantly working, reabsorbing the kilo fluids and turning it into alvo thanks to the fundamental support of the gut microbiome.
That is why throughout the colon it is absolutely normal to find fecal residues all the time, as they are produced continuously, at least as long as the organism eats and is alive.
And it is good that this happens, because the internal alvo in our colon is the result of bacterial fermentation of our friendly parasites, which also have another fundamental function: they protect the very delicate mucosal wall from attack by other potentially harmful microbes.
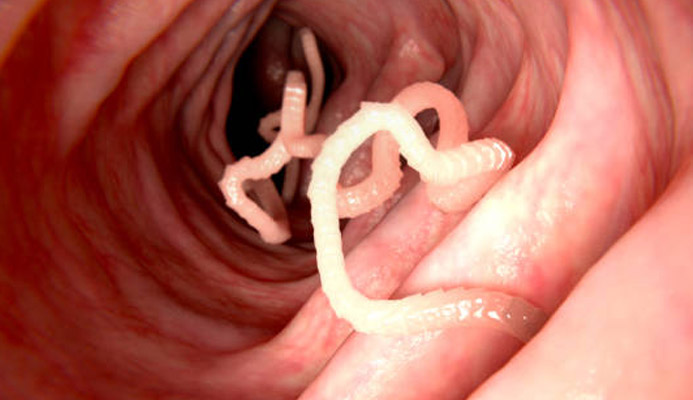
In fact, the presence of the intestinal microbiome actually forms a true protective biofilm of the intestinal mucosa from the cecum to the anal orifice.
This biofilm prevents other bacteria, or even fungi or viruses, from attacking the sensitive mucosa, thus preventing dangerous infections.
The microbiome biofilm is always mixed with fecal debris, and also covers the last part of the intestine, up to the anal canal.
It is precisely in the anal canal that the presence of the microbiome is even more important, which, together with the mucus produced by the muciparous glands, forms a kind of viscous barrier that 'sticks' and thus keeps trapped pathogenic bacteria that may try to undermine the inside of the body.
That is why this biofilm, which involves traces of feces and mucus, must always be preserved and never removed, at least if you do not want to expose the anorectal mucosa to the risk of infection and inflammation.
Anus cleansing: an ancient history, and not always so... Clean

Human evolution allowed the genus Homo to slowly rise to a bipedal position, but this evolution, which happened over millions of years, is still very short-lived compared to the advent of life on Earth (which happened billions of years ago).
Even compared to the other great apes, of which it is a member, Homo Sapiens is the only living species that has managed to achieve a full upright gait, but this evolutionary achievement still came at a cost.
Among many, that of developing hypertrophism of the buttocks and thighs, necessary to keep the whole body supported.
The anal orifice, in humans, is therefore located at the end of the buttocks, that is, at the point of their junction.
This, let's say, 'hollow' position, dissimilar to that of other mammals, results in the presence of residue after defecation, which, although it usually occurs in the straining position (i.e., squatting), still stains the perianal area and part of the buttocks.
If fecal debris within the anorectal mucosa is a normal and physiological, and therefore beneficial, presence, the same cannot be said of debris that instead remains attached to the perianal skin and buttocks.
There, fecal debris, in contact with the outer skin, can give rise to excessive bacterial fermentation, which, if excessive, can lead to the development of skin inflammation and irritation.
This fact, coupled also with the danger of soiling clothing with anus soiled with debris (notoriously unpleasant to smell) has meant that, since time immemorial, humans have tended to clean their anus after every defecation.
In times past, in really remote periods, natural leaves or water sources (if present) were used, but some ancient civilizations used the most diverse 'detergents': even desert sand, in the absence of water!
The use of toilet paper as we understand it now is of Chinese origin, dating back to the 14th century.
Before that time, our ancestors often cleaned their anuses always with leaves, soft sea sponges (as in the case of the Romans) or, simply, with their bare hands.
The use of paper in the Western, let's say, 'modern' world, dates back to the early 1600s, when it slowly took the place of the small pieces of cloth or waste paper that, especially in Europe, were available in lavatories, as early as the late Renaissance.
The advent of printed paper and the spread of newspapers from the 15th century onward not only gave a great boost to peoples' knowledge and information, but also gave them a good, inexpensive and affordable medium for... Cleansing their anus.
The historic 'inventor' of modern toilet paper is universally recognized in the figure of Joseph C. Gayetty, who proposed it in 1850: an American who first devised an inkless, soft roll of paper for anal cleansing.
It almost makes one smile to report it now, but the first name for toilet paper was not 'hygienic', but rather 'medicated': this was because Gayetty was convinced that the presence of ink on newsprint, at the time used as a cheap and practical 'toilet', caused hemorrhoidal prolapse.
Physicians at the time did not take the innovation well, and branded Gayetty and her 'medicated paper' as quackery.
In fact, they were both right: 'medicated paper' did not cure hemorrhoids at all but was still a great help for consumers, as the soft packets of paper strips were much more comfortable than rough newspapers.
Toilet paper was produced in strips and packets until 1879, when the Scott Paper Company began producing it in rolls.
It remained a 'soft' paper--only on paper, as yes definitely already soft than newspaper paper, but still impartially rough with modern paper.
Roughly 'current' toilet paper was produced in 1942, distributed in two plies, not a single compact ply.
From that year on, veils and softness increased, but basically the product remained the same.
Alongside ordinary toilet paper, however, similar but moistened products, such as cleansing wipes and the like, have appeared.
They are products conceptually similar to traditional toilet paper, yet designed to overcome the inherent 'dry cleaning' limitation that its use entails.
On the Internet, a great library of information but also a place where it often circulates unverified (and unreliable), one reads all too frequently of articles recommending so-called ' anal washes ' or 'anal lavage' before or afteranal intercourse.
Such advice, unfortunately also often given by health informants or even Doctors, is absolutely deleterious, and should be ignored.
The only cases in which the anorectal canal should be let's say so 'clean' are before video colonoscopy surgery, before examination of the abdominal aorta or a specific colonproctological surgery.
Washing the inside of the anorectal canal for hygienic purposes is detrimental to the anorectal mucosa, as it takes away the natural friendly bacterial biofilm, as well as mucus and also fecal debris, formed by the intestinal microbiota, which act as a 'plug'for the invasion of harmful microorganisms.
Performing so-called 'evacuative enemas' before anal intercourse is also not recommended: enemas and laxatives should be used only as a last resort, exclusively to prevent the formation of a fecaloma after long periods of constipation.
Their use acidifies stools, irritates the intestinal mucosa, and significantly decreases natural physiological peristalsis, thus laxing the colon.
How should the anus be cleaned? Toilet paper or cleansing with water?
Anus cleansing can be done by gentle removal of fecal debris with soft toilet paper (or moistened wipes) or, alternatively, by direct cleansing with water and detergent.
There are pros and cons of both techniques, which are easy to guess:
Toilet paper has the following pros:
- It is inexpensive and of almost widespread distribution;
- It can be taken anywhere, and it can be found anywhere;
- It is quick to use and does not require running water;
In contrast, we have:
- Although modern rolls are soft, they still perform abrasion, albeit gentle;
- It does not completely remove all residues, but only the largest ones;
- The remaining micro-residues can give rise to inflammation;
- Some very delicate people have irritation even with very soft ply toilet paper
Using the cleasing with water and detergent, on the other hand, has the following advantages:
- Enables thorough and abrasion-free cleaning
- Detergents of all kinds can be used
- Suitable for very delicate people
By contrast:
- It needs a dedicated facility
- It needs a running water source
- It cannot always be present outside the home
In a healthy person without any particular proctologic pathology, the use of toilet paper is not necessarily vited, contrary to what you may read online: it can be used, always remembering that a very soft, white paper without decorations and dyes should be preferred.
Cleaning the anus should be done gently by stapling the debris and not rubbing it against the skin, being careful not to rub past the perianal edge.
This cleaning system, however, does not guarantee the total removal of the external residue of feces, and even if done with very soft or moistened paper, it can still irritate the perianal skin and mucosa of the anal attachment.
Cleansing with water and detergent is therefore recommended, especially if you are at home or in a comfortable and familiar environment.
Now we are going to see how.
How should one cleanse the anus after defecation?
Anal cleansing is done with water and a cleanser, which should NOT be a soap.
In commercial circles, 'soap' refers to a sodium or potassium-based product, mixed with various other substances, whose main purpose is to dissolve and thus remove fat from skin tissues.
In almost all modern soaps, in addition to the lipolytic principle, there is also a surfactant component, which is essential to prevent fat from settling back on the tissues.
All soaps, due to their inherent lipolytic nature, attack not only the dirt on the skin, but also the hydrolipid film of the skin itself.
The hydrolipid film, also called the acid mantle, is the natural protection that surrounds our entire body, formed by sebum combined with sweat.
This thin, invisible film is a deadly barrier to viruses, bacteria and parasites, which are killed as soon as they settle on it because of its slight acidity.
The perianal area is naturally covered by the hydrolipid film, but this is interrupted at the junction of the anal mucosa.
An overly aggressive soap, loaded with surfactants, is therefore to be avoided for the anal and perianal area: it can create irritation by stripping away the hydrolipid film and inflaming the mucosa near the orifice.
Cleansing, therefore, should be done with cleansers specifically for the ano-genital area: there are a variety of them on the market, and they have the characteristic of having a low number of surfactants, not containing perfumes or skin irritants.
Almost all of them also have a phytotherapeutic active ingredient, with soothing action for the perianal skin, such as extracts of calendula or propolis.
Some also contain molecules of hyaluronic acid, a well-known natural skin moisturizer.
These cleansers, although very gentle and nonaggressive of the delicate hydrolipid film, should still be used methodically and in moderation.
One should not use too much of it, just the right amount: after every defecation and, for natural daily hygiene, once a day, possibly in the morning or evening.
Never overuse them because, although gentle, even ano-genital cleansers, if used too often, can damage the hydrolipid film and cause sensitization phenomena.
Any ano-genital cleanser is designed exclusively for the external area of the anal orifice, and therefore its use must be mandatorily confined to that area.
This means that cleansing should only cover the perianal area and orifice opening, and the inner canal area should never be cleaned.
The habit that some people have, the result of bad health information, of 'deep' cleaning, with a soapy finger, the anal canal, is absolutely to be avoided.
Doing so not only risks tearing of the mucosa, but also definitely irritates it, removing the natural bacterial biofilm and mucus that act as protection for the tissues.
Water used for cleansing should be room temperature or weakly lukewarm, never too hot or too cold.
For proper cleansing, simply wet the perianal area, apply very little specific cleanser (they are usually very concentrated, and only a small amount is needed), gently massage the area around the anus, leave for a few seconds, and rinse.
Drying the anus should be done with a towel made exclusively of 100 percent cotton, preferably white, not rubbing but gently dabbing only the outer perianal area and buttocks, avoiding trying to dry the inside of the anus.
This type of cleansing is necessary and sufficient to avoid irritation, inflammation, proctitis and anitis, and to maintain egregious daily hygiene of the anal area.
The anus should be dried, after proper cleansing, only with 100% pure cotton towels, preferably undyed.
Cotton does not irritate the perianal skin, is gentle, and the absence of dye pigments (which could sensitize the skin) ensures the safety of the operation.
Drying should be gentle, never rubbing the anus but dabbing gently, without excessive force.
Only the anal orifice and perianal rim should be dried, by dabbing, and never internally the anus.
Can cleansing enemas be given for the anal canal, such as before sexual intercourse?
The practice that many people practice, both heterosexual and homosexual, of performing a 'preventive cleaning' of the anal canal before anal sex is absolutely to be avoided.
As mentioned earlier, the anorectal canal is naturally protected by the bacterial biofilm of intestinal flora as well as mucus and fecal debris itself.
Any alteration to this natural physiological situation always results in irritation of the mucosa, which becomes not only inflamed but susceptible to attack by pathogenic microorganisms, which can therefore infect it.
It should be remembered that in any anal intercourse the likelihood of mucosal micro-lacerations is very high, and therefore it is precisely from those, accomplice to the possible lack of protection of bacterial biofilms and mucus, that the pathogens of Sexually Transmitted Diseases can enter.
The advice usually around on the Internet, unfortunately sometimes bestowed even by health professionals, on how and with what to 'clean' the anal canal before intercourse does not correspond to the principles of good medical practice, has no scientific basis, puts one's health at risk, and should therefore be ignored.
For proctology patients: how should anal cleansing be done?
In Medicine, a 'proctologic patient' is defined as a patient with one or more proctologic diseases or otherwise disruptive conditions to the anorectal area.
For example, a patient with hemorrhoidal prolapse, an anal fissure, ongoing proctitis or anitis, ano-genital warts that have not yet been removed, anal mucosal prolapse, etc.
This includes patients who have recently undergone proctologic surgery, such as a hemorrhoidectomy according to Milligan-Morgan, or any other anus or rectum surgery.
These patients are particularly fragile and delicate in the ano-rectal area, as the surgery they have undergone has, unnecessarily, injured some of the tissue, which therefore must rebuild and heal.
For these patients there are special post-surgical cleansers, which are usually prescribed by the Surgeon after surgery, whose composition is still already gentle, and which very often do not need to be applied by hand, but can also be sprayed in mousse.
There are many on the market, all of excellent quality, but the specific indication must be given by the Surgeon in postoperative advice.
Remember that the anorectal canal and anus are naturally 'dirty' places, and so must remain
Evolution has allowed us to develop an excellent gastrodigestive system, capable of feeding on almost anything, thus helping us in that great capacity for adaptation typical of our genus Homo.
The colon is an exceptional organ: it has many functions, the main one of which is the recovery of fluids and electrolytes, but it is also amazing because it completes its metabolic work with the help of other life, namely the colony of our friendly bacterial flora that thrives in the intestinal mucosa.
The gut microbiome is essential to complete the digestion process: our friendly bacteria 'eat' polysaccharide residues that are not absorbed by the villi in the small intestine and which, if not disposed of, would irritate the mucosa and create hyper-glycemic conditions in the body.
Not only that, but the microbiome also attacks and ferments biliary waste elements such as hemoglobin, which the kidneys cannot filter as it is insoluble in water.
At all times, our intestinal mucosa, which also makes up the anorectal canal, is always covered with friendly bacteria as well as mucus and fecal debris.
These very elements (bacteria, mucus, and fecal debris, which are then the residue of bacterial fermentation) are the only protection the mucosa has against attacks from bacteria, parasites, and viruses that may attack it from outside.
Trying to 'clean' a place that, instead, should be physiologically 'dirty' is an unnatural act, always leading to situations of inflammation or irritation.
This is why you should not worry about how 'clean' your anal canal is, but should only limit yourself to cleansing the anus and perianal border with gentle and suitable cleansers.
And, most importantly, to do so only when actually needed.
Do you have proctological problems? Dr. Troyer can help you

Dr. Luisella Troyer is an Italian Proctologist Surgeon in Dubai, with more than 30 years of medical practice.
Dr. Troyer is perfected in all anorectal disorders, such as hemorrhoidal prolapse, anal fissures, ano-genital warts, anal itching, proctitis, and anitis.
In her clinic on , Dr. Troyer completes every proctological examination with Electronic Endoscopic Videoproctoscopy: a modern, painless examination that allows the entire anorectal canal to be observed with great precision, on screen.
An irreplaceable aid for the physician to diagnose all types of proctologic pathology, sparing the patient the often abused colonoscopy.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- THE ANAL ORIFICE IS THE LAST PART OF THEINTESTINE AND THE ENTIRE LONG HUMAN GASTRODIGESTIVE TRACT;
- FOOD, CHEWED BY THE MOUTH, BEGINS A LONG JOURNEY THAT LEADS IT TO BE ABSORBED AND ASSIMILATED, UNTIL THE FORMATION OF FECES IN THE COLON;
- FECES ARE THE END RESULT OF DIGESTION, COMPOSED OF EITHER SUBSTANCES THAT ARE USELESS TO US, ALREADY STRIPPED OF NUTRIENTS, ORMETABOLIC CHEMICALS THAT WE NEED TO DISPOSE OF;
- ABOUT 80 PERCENT OF FECES IS COMPOSED OF BACTERIA AND THEIR FERMENTATION MATERIAL;
- STOOLS ARE BROWN AND SOFT PRECISELY BECAUSE OF THE ACTION OF THE BACTERIA, WHICH ATTACK POLYSACCHARIDE RESIDUES AND TURN BILIRUBIN INTO STERCOBILIN;
- THE ANUS AND ANORECTAL CANAL ARE NATURALLY PROTECTED FROM BACTERIAL BIOFILM, MUCUS AND ALSO FECAL DEBRIS;
- DEFECATION IS THE EXPULSIVE ACT OF FECES, WHICH LEAVES RESIDUE ON THE PERIANAL RIM AND BUTTOCKS;
- HUMAN BEINGS NEED TO CLEAN UP FECAL DEBRIS AFTER DEFECATION, AND THROUGHOUT HISTORY HAVE ALWAYS BEEN INGENIOUS ABOUT HOW TO DO SO;
- THE USE OF COMMON TOILET PAPER DATES BACK TO THE MID-19TH CENTURY;
- MODERN TOILET PAPER IS VERY SOFT AND GENTLE, BUT IT CAN STILL IRRITATE SENSITIVE SKIN, AND IT LEAVES UNAVOIDABLE FECAL MICRO-RESIDUES;
- CLEANSING THE ANUS BY MEANS OF WATER AND DETERGENT WOULD ALWAYS BE PREFERRED;
- SPECIFIC, GENTLE CLEANSERS SHOULD BE USED FOR ANAL CLEANSING THAT DO NOT ALTER THE ACID MANTLE OF THE PERIANAL SKIN;
- ANAL CLEANSING SHOULD STOP OUTSIDE, AND NO CLEANSER SHOULD EVER BE USED INSIDE THE ANAL CANAL;
- SOME VERY GENTLE CLEANSERS ARE AVAILABLE IN SPRAYABLE MOUSSE;
- ONE SHOULD NOT CLEANSE THE ANUS WITH WATER THAT IS TOO HOT OR TOO COLD;
- ANORECTAL 'DEEP CLEANSING' WASHES ARE ABSOLUTELY TO BE AVOIDED;
- PREPARATORY WASHES AND ENEMAS BEFORE ANAL SEX ARE ALSO TO BE AVOIDEDs

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.