Do you experience an uncomfortable burning sensation when you poop?
Is this burning so intense that sometimes it affects the quality of your evacuation, and does it frighten you so much that you have perhaps developed some kind of constipation?
Evacuation is a time of relaxation for our bodies, which is rightly perceived as necessary and, ideally, fulfilling.
Experiencing burning or discomfort during the act of evacuation is not normal, and can often compromise good physiological habits in the long run.
Read this page written by Dr. Luisella Troyer to learn what burning during evacuation is, and what can be done to resolve it.
One should always avoid starting self-managed therapies in case of anal burning, even worse if one decides to make use of over-the-counter creams or ointments.
Unfortunately, the pharmacological business of hemorrhoids is enormously greedy for many unscrupulous companies, such as one (well known) that constantly hammers with advertisements for a cream for hemorrhoidal prolapse.
Such a cream, in addition to not curing in the least the root cause of hemorrhoids (the exhaustion of tissues caused by abnormal hyper-pressure of the abdomen), deludes the patient with a palliative effect, given by the presence of lidocaine(a local anesthetic).
Of course, when the anesthetic's effect is over, the discomfort of prolapsed hemorrhoids returns.
Defecation, an indispensable physiological act for our well-being

Defecation is that natural and necessary physiological act that allows our body to discharge the waste from food, which is not needed by our metabolism and lacks nutrients, called stool.
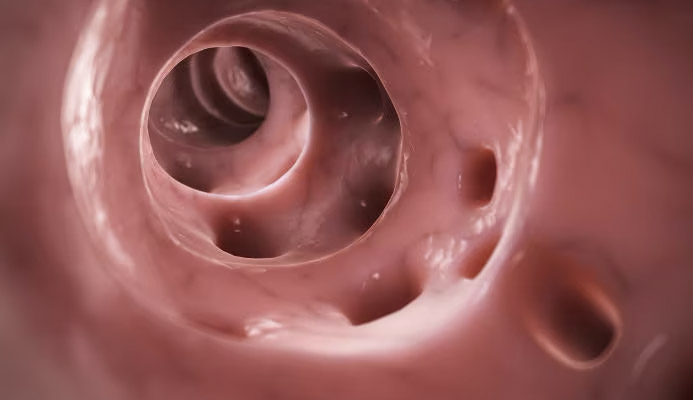
During defecation the sphincter muscles relax, the anal orifice opens, and from the rectal ampulla the feces are pushed out, effecting the discharge.
This process is perceived as relaxing, fulfilling, and generally liberating.
No pain or burning should be felt, and there should be no bleeding or excessive mucus residue.
The feces leaking from the anus should be consistent in shape, soft, cylindrical, with an odor that is not overly pungent and variable in color, but neither too light nor too dark.
Under normal conditions, defecation is a daily act (morning or evening matters little, and varies according to one's physiological habits), although variations to this daily regularity are very frequent and not necessarily pathological.
Any condition that deviates from these characteristics should therefore be viewed with suspicion, and considered a red flag for possible dysfunction or pathological conditions.
Why does one experience burning when defecating?
Experiencing a burning sensation during defecation is not a normal symptom, and therefore not part of the physiological act.
When one experiences a burning sensation during defecation, it is always because, in the anorectal canal, there is a lesion, irritation, inflammation or otherwise a pathological condition that has inflamed the delicate inner mucosa.
Often, those who experience burning during evacuation report that it manifests itself most intensely precisely at the passage of stool into the anal orifice, then subsides once the act is completed.
This is indicative of a lesion or otherwise injured area that, upon passage of feces (substantially laden with bacteria) reacts with the burning sensation.
What are the causes of burning during evacuation?

Burning during evacuation is a symptom, indicating damage to the tissues of the anorectal mucosa or peri-anal skin.
This damage can be caused by a long list of pathological conditions, among which we can mention as main ones:
- Pathological and prolapsed hemorrhoids;
- Anal fissure;
- Proctitis or anitis;
- Anal warts;
- The condition of 'wet anus'
In general, any event involving tearing or inflammation of the anal mucosa or peri-anal skin can give rise to the symptom of burning during evacuation.
Statistically, most cases of burning are reported by patients with chronic pathological hemorrhoids, poorly or never treated in the past, resulting in frequent recurrences, alternating with periods of remission.
Under normal conditions, defecation should be a daily, satisfying and relaxing act.
There should be no pain, no particular exertion during ponding, nor, of course, bleeding or burning.
When this happens, it is always a good idea to consult a Proctology Physician, for the necessary proctological inspection.
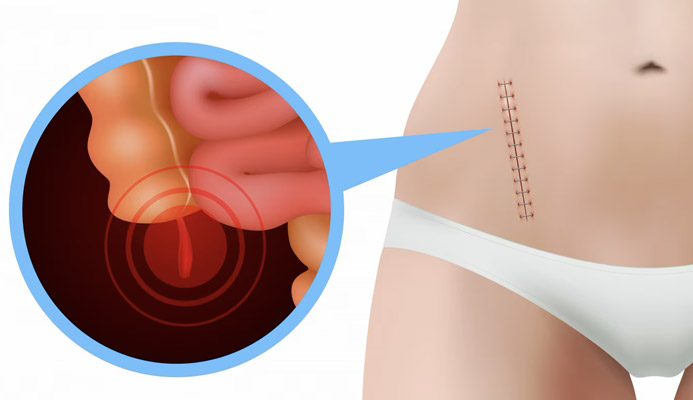
Pathological hemorrhoids and burning during evacuation
Hemorrhoids are vascular conformations found in normal human anatomy, located within the anal canal.
They are essentially pads formed by veins and arteries joined together (anastomosed, in medical jargon), which have the primary purpose of vascularizing the entire anal canal.
Under normal conditions, hemorrhoids do not give any problems, and they remain inside the anal canal without causing any discomfort.
It happens, however, that due to triggering factors or genetic predisposition, the tissue of the hemorrhoids becomes strained, leading to their congestion and prolapse, thus giving rise to hemorrhoidal pathology.
Hemorrhoidal pathology is a chronic and, if left untreated, degenerative disease.
This means that if the hemorrhoidal prolapse is not treated, it will worsen over time, increasing and descending lower and lower until it extrudes from the anal orifice, giving rise to the most severe stage of pathological hemorrhoids, namely grade IV (hemorrhoids that can no longer be reduced).
Prolapsed hemorrhoids are extremely delicate: swollen with blood, they constantly come in contact with stool, which can tear them and, therefore, bleed.
These injuries, like any other wound, can cause pain and burning, which becomes more sustained just as feces, laden with bacteria, pass through.
Anal burning during evacuation, often combined with hematochezia (anal bleeding) is thus one of the symptoms that should make one suspect a hemorrhoidal prolapse, and thus prompt the patient to a proctological examination.
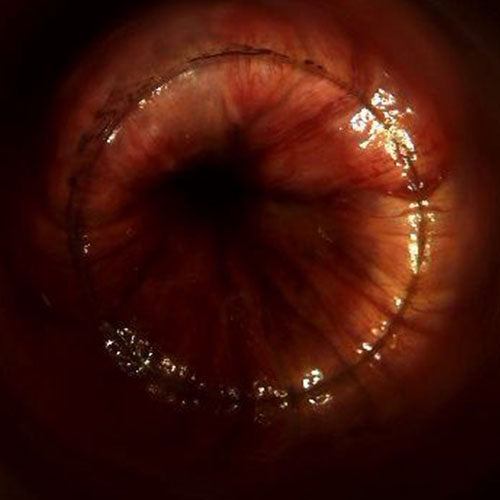
The anal fissure
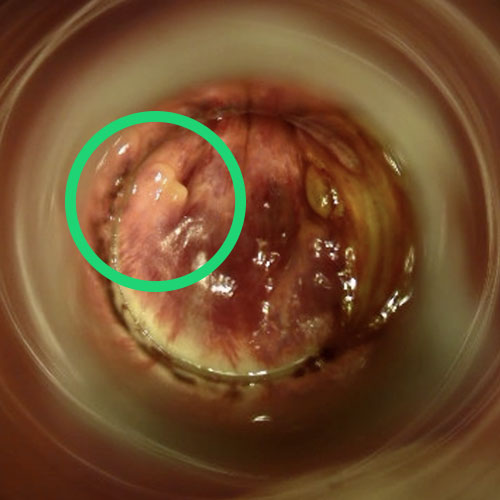
An anal fissure is a lesion of the anal canal or anal orifice characterized by slow or no healing at all.
It always forms vertically, and generally follows the pleats of the anus.
Medically, a fissure is assimilated to a true ulcer, as it shares basic features with the latter, such as:
- Slow or absent healing;
- Formation of chronic granulation tissue;
- Hardening of margins and reduced vascularization of the bottom of the sore
Ragade originates from a small lesion in the anal canal or anal orifice that, under certain conditions, fails to heal due to a lack of adequate tissue oxygenation.
Such vascular insufficiency is often caused by continuous spasms of the internal sphincter (an involuntary, doughnut-shaped muscle), which, precisely stimulated by the fissure, contracts in a hypertonus that decreases blood flow, preventing the wound from healing.
Basically, the fissure feeds itself, like a biting its own tail.
Being an open lesion, often bloody and sometimes so deep that it reaches all the way to the sphincter muscle, on contact with feces the fissure gives severe pain, coupled with equally great burning.
The pain and burning of the fissure is difficult to bear, and often lingers for hours after evacuation, greatly decreasing the patient's quality of life.
Along with pathological hemorrhoids, fissure is the most common benign lesion of the anal canal, requiring specific proctologic treatments.
Dermatitis of the anal and rectal canal: anitis and proctitis
Dermatitis is a condition of skin inflammation (phlogosis, in medical jargon) caused by a variety of factors, both irritative and infectious (e.g., a bacterial or parasitic attack).
In dermatitis, the skin becomes red, the area swells with blood and often appears sore and itchy.
When dermatitis afflicts the anal orifice or peri-anal skin, it is more properly called anitis.
When the inflammation goes further up the rectum, it is more appropriately referred to as proctitis.
Anitis and proctitis, in addition to pain and itching, also give as a symptom that of burning during defecation, due to the passage of stool over the delicate anorectal mucosa, which is inflamed and reddened.
There are many causes for which the anus and rectum can become inflamed and red, but among the main ones we can mention: pathological hemorrhoids, anal fissure, fecal incontinence with continuous stool loss, condylomatosis, parasitosis (e.g., candidiasis), or due to chemical irritation (e.g., inappropriate use of particularly aggressive detergents).
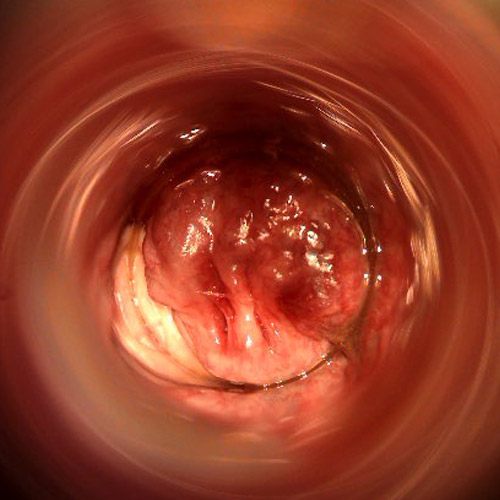
Condylomatosis
Anal warts (anal condylomata) are pre-cancerous lesions that are a symptom of HPV (Human Papilloma Virus) infection.
They essentially come in two forms: flat warts and sharp warts ('cockscomb' as they are called in the jargon).
They can affect the entire ano-rectal canal, including the peri-anal and genital skin, from which they often move by self-inoculation by the patient (who touches or shaves himself, carrying the virus to other districts of the body).
They are generally asymptomatic lesions, but in a smaller percentage of cases they can lead to burning, itching, and discomfort of the anal and peri-anal area, as well as bleeding from rubbing.
The mucosa adjacent to condylomata also may attempt to defend itself from virus aggression by increasing mucus production and, consequently, giving rise to the wet anus phenomenon, which in turn is a pioneer of proctitis and anitis.
The open anus and fecal incontinence
In Proctology, a 'open anus' refers to an anal orifice that, in the inactive phase, instead of being tightly clamped, remains partially open, thus leaking mucus, gas, and fecal debris.
There can be a wide variety of reasons for this incontinence, but they are usually associated with an injury or otherwise damage to the sphincter muscles.
This damage in turn has different causes: in most cases, the injury is given during childbirth, and the resulting hyper-pressure of the pelvic area.
Then there are pathological conditions that can damage the anal sphincters, such as pathological hemorrhoids and their prolapse, anal abscesses, and anal fistulas, as well as surgeries designed to resolve precisely such issues, which sometimes (playfully) leave permanent scar conditions.
Then there are congenital and autoimmune pathological conditions, such as chronic bowel diseases (ulcerative rectocolitis or Crohn's disease, for example) that can play a major role in fecal incontinence.
Also not to be underestimated are causes of purely neurological origin, such as those brought on by spinal cord injury, a stroke, or the ever-present diabetic neuropathy.
What to do when you experience burning during evacuation?
As mentioned earlier, burning during defecation is a symptom of an injury, or otherwise inflammation, of the anorectal mucosa or peri-anal skin.
The cause of this inflammation is the goal of medical investigation, which must be conducted by the referring specialist, namely the Proctologist Physician.
Therefore, if you experience burning during evacuation, the sensible thing to do is to make a specialized proctological examination with a Proctologist Physician.
In fact, the Proctologist is the health specialist perfected in all affections of the anus and rectum, with great experience in diagnosing the causes of anal burning.
It is to him, therefore, that you must turn to understand the order of the burning, and to have the appropriate therapy prescribed.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
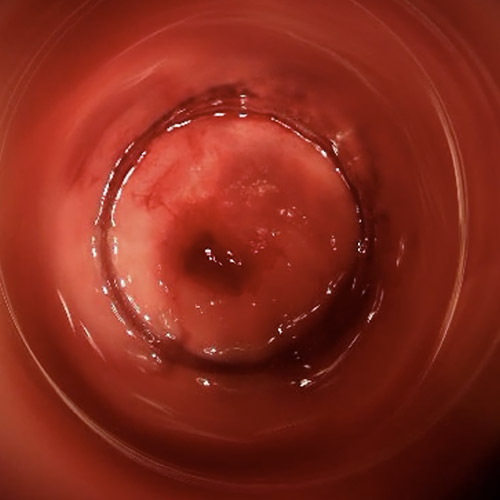
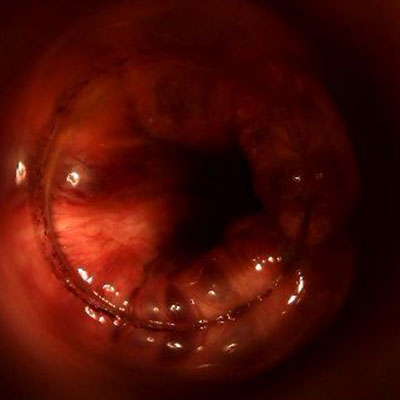
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- DEFECATION IS USUALLY A DAILY ACT, WHICH SHOULD NOT CAUSE PAIN, BURNING, OR BLEEDING;
- BURNING DURING EVACUATION IS NOT NORMAL, AND SHOULD ALWAYS RAISE SUSPICION OF DAMAGE OR IRRITATION OF THE ANORECTAL TISSUES;
- PATHOLOGICAL HEMORRHOIDS CAN LEAD TO INFLAMMATION OF THE ANAL MUCOSA, RESULTING IN BURNING;
- ANALFISSURE IS A LESION OF THE ANAL CANAL, WHICH OFTEN CAN RESULT IN BURNING AND BLEEDING;
- ANITIS IS A DERMATITIS OF THE ANUS AND PERI-ANAL AREA, AND BURNING ISONE OF ITS TYPICAL SYMPTOMS;
- MACERATION OF THE PERI-ANAL SKIN DUE TO FECAL INCONTINENCE OFTEN CAUSES VIOLENT DERMATITIS, RESULTING IN ANAL BURNING

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.