
Do you know what is the number one disease that affects human beings all over the world?
n fact, this supremacy has been contested, practically since time immemorial, by two specific afflictions that, curiously enough, concern the beginning and end of the long human gastrodigestive system: dental caries and pathological hemorrhoids.
Probably you didn't know but hemorrhoidal prolapse is, along with dental caries, by far the most common disease in every country in the world, whether developed or developing.
This figure should immediately make you realize what a 'target' pathological hemorrhoid patients can be for commercial purposes: a huge catchment area, just waiting to be 'satisfied' with a good.
A good that is possibly low cost, easily usable, and promises results of immediate relief.
Unfortunately, this exquisitely commercial reasoning underlies many of the sales strategies of an almost endless array of pharmaceutical companies, which for decades have been clogging the market with all sorts of creams, ointments or salves with supposed beneficial effects on hemorrhoidal prolapse.
In almost all cases, these 'beneficial effects' are entirely palliative, and in any case never resolving the hemorrhoidal pathology, which, as we will now go on to see in this article, cannot be resolved with a simple cream.
Read this page written by Dr. Luisella Troyer, Proctologist Surgeon, to find out if the hundreds of creams and ointments that, on a daily basis, invade TV, newspapers and the Internet with their pounding advertisements can really be an effective remedy for hemorrhoidal prolapse.
Ah, Dr. Troyergives you a lightning spoiler, right at the beginning of the article: no, they are never a remedy.
And now we will go to see why.
The beneficial effect that some ointments commonly available in pharmacies allow is purely momentary, and is caused by the presence of a small percentage of lidocaine, a well-known local anesthetic.
But once the anesthetic's effect has passed, the symptoms of hemorrhoidal prolapse begin again, since no topical cream can cure the original cause of hemorrhoidal disease,which remains the mechanical extrusion of the plexuses into the anal canal, given by the exhaustion of the supporting tissues.
What are hemorrhoids?
Hemorrhoids are natural arteriovenous plexuses located within our anal canal, that is, the very last part of the rectum, leading to the opening of the anal orifice.
They are soft pads formed by veins and arteries fused together in what is called anastomosis in medical jargon.
There are three main hemorrhoid plexuses: left lateral, right anterior and right posterior, plus two other small plexuses termed secondary.
The task of hemorrhoids is to vascularize the entire anal canal and, secondarily, to contribute to fecal continence by helping the internal sphincter (the involuntary sphincter) tighten the anus well in a resting condition.
In a healthy human being without proctological problems, hemorrhoids are not even perceived, and do not create any problems.
It is only when the plexuses become inflamed and, due to a long series of causes and triggers, extrude outside the anal canal that we speak of hemorrhoidal pathology, or hemorrhoidal prolapse.
What is hemorrhoidal prolapse?

A hemorrhoidal prolapse occurs when one or more hemorrhoidal plexuses become enlarged, swell excessively with blood, and, due to the force of gravity, extrude downward toward the anal orifice.
Hemorrhoidal prolapse does not yet have a definite and certain cause, but Medicine hypothesizes two main causes: exhaustion of the supporting tissues of the hemorrhoids (the mechanical theory) and increased intra-abdominal pressure, which in turn causes swelling of the plexuses and increased blood flow (the hemodynamic theory).
With hemorrhoidal prolapse, the hemorrhoids slowly extrude from their original position and move closer to the anal orifice, emerging from it in severe and final cases of the condition.
Chronic constipation is that pathological condition that prevents the normal evacuation of soft, well-formed stools on a daily basis .
Constipation, also called constipation, has many causes, some times congenital (e.g., from abnormal length of the colon) other times given by wrong eating habits.
Constipation is a known trigger of pathological hemorrhoids, as the continuous effort in pouching that the patient must make to try to expel stool that is too hard causes an increase in intra-abdominal pressure.
This increase exhausts the supporting tissues that anchor the hemorrhoids to the wall of the anal canal, causing, in the long run, the onset of their prolapse.
Why do hemorrhoids prolapse and come out of the anus?
As mentioned just above, Medicine has not yet found an unambiguous explanation for hemorrhoidal prolapse, but the two main theories, namely mechanical and hemodynamic, are suspected to be part of the same problem.
Natural aging generates a slowdown in metabolism and, as a result, a decrease in the quality and quantity of collagen and elastin, essential proteins in our connective tissues that make hemorrhoids remain firmly anchored to the anal wall.
On the other hand, chronic increases in intra-abdominal pressure, e.g., during pregnancy, childbirth, certain sports and strenuous work, or simply given by chronic and never adequately treated constipation.
This increase in intraabdominal pressure leads to an increase in vascular pressure, which in turn swells the hemorrhoidal plexuses more and more and, also complicit in mechanical exhaustion, leads to the onset of prolapse.
Can one be predisposed for hemorrhoids?

Medicine has long established that hemorrhoidal disease itself is not hereditary, but instead the quality of the tissues of the venous system, particularly the inner wall of the veins, is hereditary.
And hemorrhoids are also veins, so venous endothelial tissue mixed with arterial tissue.
From this, it can be understood that if there is a family history of venous disease, such as mother or father with chronic venous insufficiency, there is an increased risk of developing hemorrhoidal disease.
Granted, however, there needs to be a trigger, or even multiple triggers, such as increasing age, sedentary lifestyle, childbirth, or chronic constipation (just to name a few) to initiate prolapse.
What are the triggers of hemorrhoids?

Speaking of hemorrhoids, triggering factors are defined as all those secondary factors, that is, acquired in the course of life, that can either worsen the primary causes or cause prolapse to be 'triggered' in the first place.
The triggers of hemorrhoids long known to Medicine therefore are:
- Chronic constipation;
- Pregnancy and childbirth;
- Overweight and obesity;
- Sedentary living;
- A low-fiber diet and proper hydration;
- Some sports, such as weightlifting and cycling;
- Some time-consuming work in the orthostatic position;
- Some fatigue work, which requires daily lifting of weights
These factors can also add up, depending on the patient's lifestyles, making the likelihood of the onset of hemorrhoidal prolapse even worse.
Any cream or ointment, regardless of its quality and active ingredients, if used for too long in the anal and peri-anal area causes, in the long run, skin sensitization, resulting in dermatitis.
Anitis (inflammation of the anus and peri-anal area) caused by the immoderate use of soothing creams for hemorrhoids is a very frequent problem in patients with hemorrhoidal disease, and therefore should be avoided, trying to limit the use of topical preparations.
Inordinate use of cortisone creams, then, worsens the delicate bacterial balance of the anal and peri-anal area: all steroid molecules are in fact immunosuppressants, as well as being particularly greedy 'food' for fungi, yeasts and molds.
Prolonged use of steroid creams on the anal and peri-anal area therefore often results in violent episodes of anal candidiasis, as well as can also pave the way for opportunistic infections, such as those due to the HPV virus.
What are the symptoms of pathological hemorrhoids?

Pathological hemorrhoids manifest symptomatically with a range of complaints whose severity varies with the severity of the plexus prolapse itself.
Although the symptomatology can therefore vary greatly, even depending on the patient, generally these elements are present:
Bleeding, usually at defecation
Bleeding, with hematochezia (bright red blood loss) is a hallmark of pathological hemorrhoids, and is caused by the rubbing of feces, especially hard stool, right on the processed outer wall of the hemorrhoids during defecation.
Hematochezia may be dripping, leaving bright red blood residue and streaks on stool or toilet paper, or it may manifest as small clots of already clotted blood, which the patient notices only by wiping.
Often this symptom puts genuine terror on the patient, who thinks he or she is suffering from malignant diseases, and prompts him or her to rush urgently to the Doctor;
Burning during defecation
Burning during defecation is another typical symptom of prolapsed hemorrhoids, and is manifested by the passage of bacteria, with which the feces are laden, over the injured mucosa of the hemorrhoids.
The burning begins to expand as early as defecation, and usually passes within a few minutes of the end of the act, but sometimes (especially if hemorrhoids are associated with intense proctitis) it can last for hours after evacuation;
Anal itching
The anal mucosa, unlike the outer skin, does not have a stratum corneum to protect it, such as during inflammation.
Therefore, in an attempt to protect itself, the body increases the production of mucus, which is that viscous substance that lubricates the anorectal canal and, at the same time, performs automatic mucosal protection.
Hemorrhoids are seen by the body as an inflammation of the normal physiological condition, and therefore the mucosa, to protect itself, increases mucus production.
The hyper-production of mucus generated by hemorrhoidal prolapse makes the anal canal and anus very moist, and this leads to maceration of the skin, which becomes inflamed and thus develops proctitis, that is, topical dermatitis of the anorectal canal.
In turn, proctitis also extends to the anal orifice, causing peri-anitis, resulting in burning, redness, heat sensation, and anal itching.
Is there a classification for the severity of hemorrhoids?
Yes, there is a severity scale based on four stages, of progressive order according to the volume of prolapse:
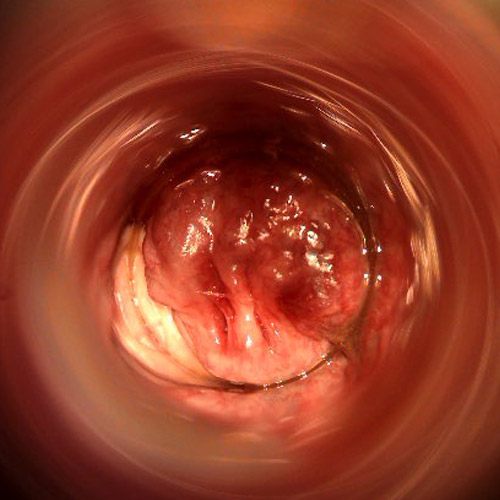
Stage I hemorrhoids
Hemorrhoidal prolapse is minimal, and the hemorrhoids are all still found to be inside the anal canal, and therefore not observable from the outside.
They rarely give rise to bleeding, which can still be there, while the sensation of an external body in the anus, which patients often report, especially after defecating, is more likely;
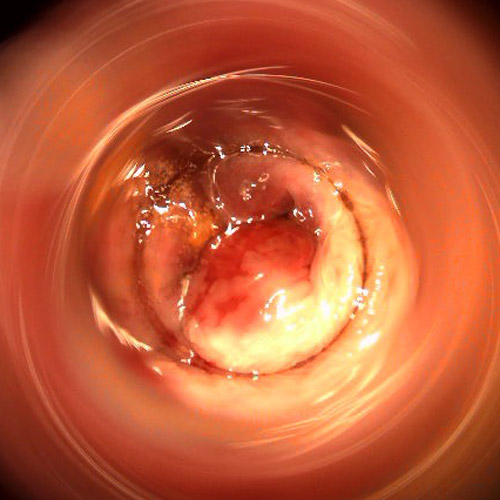
Stage II hemorrhoids
Hemorrhoidal prolapse extrudes out of the anus only during defecation or some straining, then spontaneously re-enters soon after.
Bleeding during defecation, burning and itching, caused by excessive mucus production, may be present.
Painful hemorrhoidal thrombus may appear, the result of a thrombophlebitis process right in the extruded plexuses;
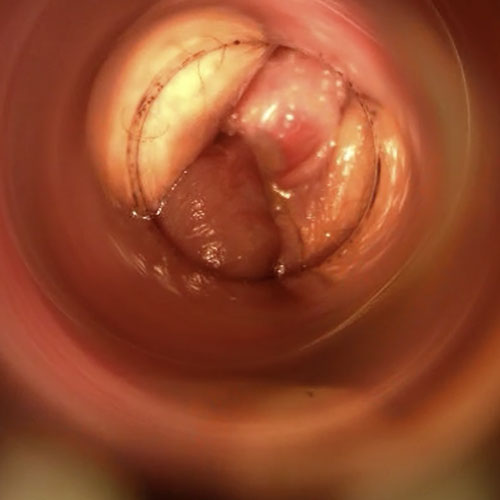
Stage III Hemorrhoids
The hemorrhoidal prolapse extrudes completely out of the anal orifice, but can still be repositioned inside with appropriate manual maneuvering.
Bleeding, pain on defecation accompanied by almost constant burning and itching at the anal orifice are typical symptoms of this stage, in which painful hemorrhoidal thrombus formation is always possible;
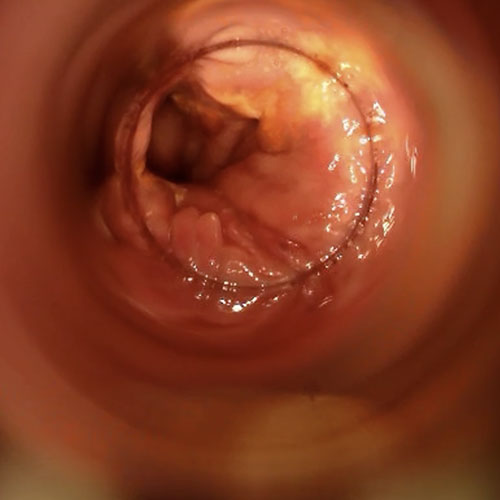
Stage IV hemorrhoids
The hemorrhoidal prolapse is permanently extruded from the anal orifice, and cannot be repositioned even by manual maneuver.
Symptoms are the same as stage III, only with the increased likelihood of infection and large inflammation of the entire peri-anal area, which often make even normal daily living difficult.
As the most common condition in the world along with dental caries, hemorrhoids are a very attractive business for pharmaceutical companies.
Reinforcing the sense of an almost endless production of topical products (almost all of which are Over-the-Counter) is the embarrassment and fear of many patients, who prefer to try 'do-it-yourself' solutions rather than go to the Proctologic Surgeon.
For many, it is more acceptable and confidential to attempt to treat themselves with topical creams rather than make a proctological examination.
It is precisely this - senseless - fear and shame that is often the cause of unjustifiable delays in the initiation of treatment, with progressive increase in the volume and severity of prolapse, which often reaches such high levels that it severely affects the patient's daily life.
What is the treatment for hemorrhoids?

Therapy for pathological hemorrhoids is directly proportional to their state of severity, and the residual elasticity of the plexus tissues.
Mild hemorrhoids in patients who are still young can be treated effectively with the right dietary therapy and the use of flavonoids, relying on the possibility of regeneration of the body's elastic tissues.
In many cases, by softening the stool and flushing the congestive hemorrhoids, they retract and return, within limits, to their normal anatomical position.
Then, in addition to medical therapy, there are some minimally invasive surgical therapies, which can be performed on an outpatient basis, to reduce the prolapse condition.
Some of them are now obsolete, such as elastic ligation, while others have not fully yielded the hoped-for results, such as selective dearterization with HeLP technique.
These techniques have been almost completely supplanted by sclerosant therapy with the new stabilized scleromousse, which can also be performed conveniently in an outpatient setting.
High-grade hemorrhoids, grade III and above, until a few years ago required necessary surgery, performed with a hemorrhoidectomy technique according to Milligan-Morgan.
This type of surgery, which is radical and effective but decidedly uneventful postoperatively, is slowly being supplanted by sclerosing therapy with scleromousse, with infinitely lower costs and almost equal statistical results (more than 95% of patients permanently cured).
The indication for either treatment is given, of course, by the Proctologist Surgeon after the proctologic examination and the necessary proctoscopy, now replaced, in top practices, by Electronic Endoscopic Videoproscopy.
How useful are creams and ointments against hemorrhoids?

Hemorrhoids are basically a vascular and, therefore, a hydraulic problem.
The failure of the supporting and anchoring tissues of the hemorrhoid plexuses, the exhaustion of them, and the inability of the body to rebuild them effectively generates a slow but progressive downward prolapse due to the omnipresent force of gravity.
The more the hemorrhoids swell with blood, the more their weight increases, and as a result the tissues holding them to the anal wall, already tried and exhausted, collapse even more.
At the current state of Medicine, there is still no certain and reliable medical therapy capable of regenerating, or rather prompting the body to effectively regenerate, the now damaged hemorrhoidal connective tissues.
Apart from the mild stages of prolapse in patients who are still young, where excellent results can be achieved by modifying the diet and flaring the hemorrhoidal congestion, the chronic stages of pathological hemorrhoids must all be treated with destructive therapy.
Whether surgical, by means of Milligan-Morgan hemorrhoidectomy, or medical by means of the new sclerosing therapy with scleromousse, the hemorrhoidal plexuses must still be removed.
That being said, it comes logical to think that no cream or ointment can do this.
Regardless of its quality and the pharmaceutical company that produced it.
There is no type of cream, ointment, or salve that can sclerotize or remove the hemorrhoidal plexuses that are swollen with blood and from the now frayed connective tissue.
The ointments that are commonly advertised, often with a massive marketing campaign, are soothing at best, sometimes even anesthetizing because of the small percentage of lidocaine in the preparation.
In addition to this, their function is nothing in treating the primary cause of hemorrhoids, namely prolapse of the plexuses and their blood swelling.
Why could the advertising and sale of hemorrhoid ointments be allowed?
Because any ointment sold as a remedy for hemorrhoids is careful not to call itself a 'cure' for hemorrhoidal disease.
In Medicine, 'cure' means the complete and final remission of all symptoms, and a return to physiological normalcy.
Hemorrhoid ointments obviously cannot guarantee this, and in fact it is always clearly stated on their packaging and on their bugiardino that they perform symptomatic treatment for pathological hemorrhoids.
In Medicine, 'symptomatic treatment' means nothing more than a palliative remedy, which relieves symptoms but has no effect on the cause of the disease.
In doing so, pharmaceutical manufacturers obtain approval from the local Ministry of Health or Drug Administration to sell a simple palliative ointment, which aggressive marketing, however, also playing and leveraging the population's health ignorance, often passes off as a phenomenal remedy.
In fact, given that almost all of these 'anti-hemorrhoid' creams are simply Over-the-Counter (i.e., over-the-counter, non-prescription drugs), the figure who should warn the patient about the limitations of such treatments is the pharmacist.
Unfortunately, for mere commercial interests (and often, for lack of proper medical training), pharmacists sell products that are unsuitable for the patient, which do not solve the cause at all but rather, often, worsen the problems, causing the patient to delay the proctological examination and the initiation of real therapy for the definitive resolution of hemorrhoids.
Hemorrhoids are the number one disease in the world, always remember that
Always remember that hemorrhoids, along with dental caries, are the most common disease among humans.
Their incidence may vary in the population, but remains consistently high in all countries of the world.
The real numbers of hemorrhoidal disease are difficult to obtain, as it is often under-diagnosed or never diagnosed at all, due to the refusal of many patients to be seen by the Doctor.
But we are still talking about very high numbers of potential patients.
Numbers that, in fact, are intercepted by pharmaceutical companies, which sell a simply absurd amount of ointments, creams and ointments of all kinds, but which are all incapable of curing the original cause of hemorrhoids.
Sort of like the hundreds of cosmetic ointments for phantom 'cellulite' or the hodgepodge of endless cosmetic products to combat skin wrinkles.
Million-dollar businesses, which always appeal to an easy-to-understand concept: it's nice to think that an ointment costing a few tens of euros solves a big problem.
In fact, Medicine works precisely according to opposite principles: usually, big problems require very energetic solutions, and never the other way around.
Remember this whenever you see an advertisement that aims to make you believe that you will get wellness for a mechanical, chronic problem simply by applying a cream to it.
Is there any medication that can treat hemorrhoids?
No, no medication can cure the root cause of hemorrhoids, which always remains prolapse due to exhaustion of the supporting tissues of the plexuses.
However, there are excellent drugs, to be used only by prescription, that can tone the internal tissue of hemorrhoids and contribute, albeit within limits, to the decongestion of inflammatory hemorrhoid states.
These are flavonoid-based drugs, which Medicine has long since established as extremely useful, on an exquisitely tonic level, for the treatment of mild stages of hemorrhoidal prolapse.
However, these drugs are almost useless on advanced stages of prolapse, where the only sensible option is hemorrhoidectomy or sclerosing therapy with scleromousse.
So what to do to heal hemorrhoids?

Permanent healing from hemorrhoids is possible, but there is only one way to initiate it: perform a proctologic examination with an experienced and trained Proctologist Surgeon.
Only the proctological examination, with the necessary Electronic Endoscopic Videoproscopy, can determine the exact level of prolapse, and indicate to the physician the right therapy suitable for the patient.
The use of creams, ointments, gels, and over-the-counter products in general is essentially useless in treating the root cause of pathological hemorrhoids, which is and always remains exquisitely mechanical.
There are many effective medical and surgical therapies for pathological hemorrhoids, but they are not achieved by going to the pharmacy, nor by slathering the prolapse with a cream.
This needs to be clear to every patient, just as it needs to be clear once and for all (including to health personnel in pharmacies) that products for symptomatic treatment should be sold in moderation, and only in cases of immediate need.
A proctological medical examination should always be recommended regardless, before any administration of creams, ointments and various topical products.
Do you suffer from hemorrhoids in Dubai? Dr. Troyer can help you, give her a call

Dr. Luisella Troyer is a Proctology Surgeon with over 30 years of experience in Proctology.
At her Dubai clinic, Dr. Troyer can help you diagnose the degree of your hemorrhoids and offer definitive and effective treatments to resolve them.
Relying on Medicine and Surgery, according to principles of science and conscience, and not on symptomatic creams or ointments, which do not treat the original causes of prolapse.
The Doctor is first and foremost a Physician who has dedicated her entire life to protecting life itself, and to alleviating the suffering of patients.
Also, and perhaps most importantly, of all the patients who are constantly disparaged about the problem of hemorrhoidal prolapse and who, often ineffectively, for years and years spend money, time, pain, and effort on often wholly ineffective treatments that only serve to increase their level of discouragement and frustration.
your proctologist surgeon of excellence in Dubai

Dr. Luisella Troyer is an italian Vascular Surgeon, specialised in Proctology and Colonproctology, operating in Dubai.
In the modern, well-equipped clinic in Dubai, Dr. Troyer provides specialist medical examinations in Vascular Surgery and Colonproctology, to diagnose and solve proctological problems such as:
- Pathological haemorrhoids;
- Haemorrhoidal thrombus;
- Anal fissures;
- Anal warts;
- Peri-anal abscesses and anal fistulas;
- Chronic constipation;
- Irritable Bowel Syndrome;
- Faecal incontinence;
- Rectocele;
- Descending perineum syndrome
In the clinic in Dubai, Dr. Troyer also performs minimally invasive treatments, such as the treatment of prolapsed haemorrhoids with the innovative sterilised air-stabilised scleromousse.
For her proctological diagnoses and examinations, Dr. Troyer uses the excellence of diagnostic technology, such as the modern high-definition videoproctoscope for Electronic Endoscopic Videoproctoscopy.
All operators and assistants of Dr. Troyer speak English, Arabic and Italian.
So remember...
- HEMORRHOIDS ARE VASCULAR PLEXUSES FORMED BY ARTERIES AND VEINS JOINED TOGETHER AND POSITIONED INSIDE THE ANAL CANAL;
- THE MAIN PURPOSE OF HEMORRHOIDS IS TO SUPPLY THE ENTIRE ANAL CANAL WITH BLOOD AND, SECONDARILY, TO CONTRIBUTE TO FECAL CONTINENCE;
- THERE ARE THREE MAIN HEMORRHOID PLEXUSES: LEFT LATERAL, RIGHT ANTERIOR AND RIGHT POSTERIOR;
- UNDER NORMAL CONDITIONS, HEMORRHOIDS DO NOT GIVE ANY PROBLEMS;
- WHEN HEMORRHOIDS SWELL EXCESSIVELY WITH BLOOD AND EXTRUDE OUTSIDE THE ANAL CANAL, IT IS CALLED HEMORRHOID PATHOLOGY;
- EXTRUDED HEMORRHOIDS MAY BECOME INFLAMED AND CONGESTED, GIVING SYMPTOMS SUCH AS BURNING ON DEFECATION, ANAL PAIN AND DISCOMFORT, BLEEDING, AND ANAL ITCHING;
- THE UNAMBIGUOUS CAUSE OF THE ONSET OF HEMORRHOIDAL DISEASE IS NOT KNOWN TO SCIENCE, BUT THERE ARE TWO MAIN THEORIES, THE MECHANICAL AND THE HEMODYNAMIC, WHICH ARE NOT NECESSARILY IN CONFLICT WITH EACH OTHER;
- FAMILIARITY WITH CHRONIC VENOUS INSUFFICIENCY IS A RISK FACTOR FOR THE ONSET OF PATHOLOGICAL HEMORRHOIDS;
- CHRONIC CONSTIPATION, PREGNANCY, CHILDBIRTH, CERTAIN SPORTS OR STRENUOUS WORK, OR CHRONIC BOWEL DISEASE SUCH AS IRRITABLE BOWEL SYNDROME MAY BE TRIGGERS FOR THE ONSET OF HEMORRHOID PROLAPSE;
- MILD STAGES OF HEMORRHOIDAL PROLAPSE CAN BE EFFECTIVELY RESOLVED WITH THE RIGHT DIET AND THE USE OF FLAVONOID AND INTERNAL HEMORRHOIDAL TISSUE TONIFYING DRUGS ;
- ADVANCED STAGES OF HEMORRHOIDAL PROLAPSE ARE TREATED WITH SURGERY AND HEMORRHOIDECTOMY OR SCLEROTHERAPY WITH STABILIZED SCLEROMOUSSE;
- THERE IS NO TOPICAL OINTMENT ON THE MARKET THAT CAN TREAT THE UNDERLYING CAUSE OF HEMORRHOIDS, WHICH REMAINS THE DEGENERATION AND EXHAUSTION OF THE SUPPORTING TISSUES OF THE HEMORRHOID PLEXUSES;
- THE OINTMENTS COMMONLY FOUND ON THE MARKET HAVE A MERE SOOTHING AND, IN SOME CASES, ANESTHETIZING EFFECT, BUT ARE NOT CAPABLE OF CURING THE CAUSES OF HEMORRHOIDS, WHICH REMAIN MECHANICAL;
- PROLONGED USE OF ANY KIND OF CREAM CREATES, IN THE LONG RUN, SENSITIZATION OF THE PERI-ANAL AREA, WHICH CAN GIVE RISE TO VIOLENT DERMATITIS;
- IF YOU EXPERIENCE THE SYMPTOMS OF PATHOLOGICAL HEMORRHOIDS, THE SENSIBLE THING TO DO IS NOT TO RELY ON OVER-THE-COUNTER PRODUCTS, BUT TO CONSULT A PROCTOLOGICAL SURGEON FOR THE NECESSARY PROCTOLOGICAL EXAMINATION

This article was revised and updated by Dr. Luisella Troyer on:
Tuesday 4 February, 2025
Dr. Luisella Troyer is a Vascular Surgeon, specialising in Vascular Surgery and Proctology.
Since her training as a resident, Dr. Troyer has been interested in the study and treatment of proctological pathologies, especially haemorrhoids and haemorrhoid prolapses.
In the course of his practice as a Surgeon, he has accumulated about 5000 operating theatre hours as a first operator, of which about 120 were Milligan-Morgan haemorrhoidectomies.
He is one of the first Doctors to have studied and experimented with scleromousse therapy for pathological haemorrhoids, which he has judged to be the treatment of choice for the non-traumatic treatment of haemorrhoidal prolapses, with resolution statistics of over 95% and therefore often comparable with surgical access.

















